My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.105 n.9 Madrid Oct. 2013
https://dx.doi.org/10.4321/S1130-01082013000900014
LETTERS TO THE EDITOR
Methicillin resistant Staphylococcus aureus liver abscess related with colorectal cancer
Absceso hepático por Staphylococcus aureus resistente a la meticilina relacionado con un cáncer colorrectal
Key words: Staphylococcus aureus. Methicillin resistance. Liver abscess. Colorectal neoplasm.
Dear Editor,
Pyogenic liver abscess (PLA) is a clinical entity usually related to hepatobiliary tract disease or intra-abdominal infection (1). Recently, the association to non-metastatic colorectal cancer have been reported worldwide, mostly in eastern Asian countries (2,3). Staphylococcus aureus is an uncommon cause of liver abscess, but recovery of methicillin resistant Staphylococcus aureus (MRSA) is extremely rare (4,5). To our knowledge, we describe the first reported case of MRSA liver abscess associated to non-metastatic colorectal cancer in Europe.
Case report
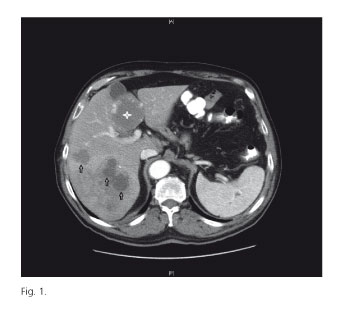
A 76-year-old Caucasian man was admitted to the hospital for a 7-day history of fever, and several episodes of bloody diarrhea in the last month. His past medical history was relevant for hypertension and dyslipidemia, but he denied recent hospitalization, recent antibiotic use, intravenous or subcutaneous drug use, or recent travel. The physical examination showed an ill-appearing male with mucocutaneous pallor, and the abdomen was soft with no palpable masses. Significant laboratory data included neutrophilic leukocytosis (15.8 x 109/L, neutrophils 85%), and an elevated C-reactive protein level (176.2 mg/L). Blood and stool cultures were negative. Abdominal US showed typical hemangiomas, coexisting with multiple hypoecogenic lesions suggestive of liver abscesses. Contrast-enhanced CT was performed for better evaluation of hepatic lesions (Fig. 1). CT-guided percutaneous aspiration of one of the abscesses was performed, and result of pus culture was positive for MRSA. Based on abscesses size (< 3 cm), patient was treated with a 4-week course of IV linezolid, and his clinical condition improved rapidly. Follow-up CT showed resolution of liver abscesses, persisting only typical hemangiomas. Colonoscopy was performed, showing a tumor of the rectum consistent with an infiltrating adenocarcinoma. The patient underwent neoadjuvant therapy prior surgery, and later adjuvant chemotherapy.After 6 months of follow-up, the patient remains in good health, with no recurrence.
Discussion
Etiologies and pathogenesis of liver abscesses have changed significantly over the past several decades. Recently, many cases of PLA associated with non-metastatic colorectal carcinoma have been reported worldwide. Interestingly, 80% of reported cases occurred in Eastern Asian countries, especially Japan, China, and Korea. Mucosal defects present on colonic lesions allowing a route for bacteria invasion into the portal system with subsequent hematogenous spread to the liver is regarded as the key process (6). Staphylococcus aureus has been a reported pathogen in less than 10% of liver abscesses, but reports of methicillin resistant strain are even fewer. This finding makes unclear if liver abscesses caused by Staphylococcus aureus (including methicillin resistant strains) follow a different natural history than those caused by enteric flora. Treatment of PLA has also evolved over the last decade such that percutaneous drainage is now the most common approach, with the potential to enhance systemic antibiotic therapy by providing bacterial speciation and antimicrobial sensitivities (7). Systemic antibiotic therapy alone, has also been shown to be effective as primary treatment of PLA in well-selected patients with small abscesses (< 3 cm). This case illustrates an unusual etiology of colorectal cancer-related PLA, and highlights the tremendous problem of MRSA, which requires global strategies for control and prevention of the infection.
Luis Enrique Lezcano-Gort, Alba Calderón-Pecellín and Joaquín Antón-Martínez
Department of Internal Medicine. Hospital General San Pedro de Alcántara. Cáceres, Spain
References
1. Branum GD, Tyson GS, Branum MA, Meyers WC. Hepatic abscess. Changes in etiology, diagnosis, and management. Ann Surg 1990;212:655-62. [ Links ]
2. Lee JK, Kum J, Ghosh P. Nonmetastatic cancer of the colon associated with pyogenic liver abscess. Am J Gastroenterol 2008;103:798-9. [ Links ]
3. Qu K, Liu C, Wang ZX, Tian F, Wei JC, Tai MH, et al. Pyogenic liver abscesses associated with nonmetastatic colorectal cancers: An increasing problem in Eastern Asia. World J Gastroenterol 2012;18:2948-55. [ Links ]
4. Wong VW, Cheung YS, Wong J, Lee KF, Lai PB. A community-acquired methicillin-resistant Staphylococcus aureus liver abscess. Hong Kong Med J 2010;16:227-9. [ Links ]
5. Smith BM, Zyromski NJ, Allison DC. Community-acquired methicillin-resistant Staphylococcus aureus liver abscess requiring resection. Surgery 2007;141:110-1. [ Links ]
6. Lim WC, Lim CC. Silent colorectal carcinoma and pyogenic liver abscess. J Gastroenterol Hepatol 2004;19:945-6. [ Links ]
7. Mezhir JJ, Fong Y, Jacks LM, Getrajdman GI, Brody LA, Covey AM, et al. Current management of pyogenic liver abscess: Surgery is now second-line treatment. J Am Coll Surg 2010;210:975-83. [ Links ]