Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.105 no.10 Madrid nov./dic. 2013
https://dx.doi.org/10.4321/S1130-01082013001000009
CLINICAL NOTES
Acute pancreatitis and superior mesenteric artery syndrome
Pancreatitis aguda y síndrome de la arteria mesentérica superior
Denisse Joan Sihuay-Diburga, Anna Accarino-Garaventa, Jaime Vilaseca-Montplet and Fernando Azpiroz-Vidaur
Department of Gastroenterology. Hospital Universitario Vall d' Hebron. Universidad Autónoma de Barcelona. Barcelona, Spain
ABSTRACT
Superior mesenteric artery syndrome (SMAS) has been proposed as a rare cause of proximal bowel obstruction resulting from compression of the third portion of the duodenum secondary to narrowing of the space between the aorta and superior mesenteric artery. The main risk factors associated with SMAS are significant weight loss, corrective spinal surgery and congenital or acquired anatomic abnormalities. Its association with acute pancreatitis has been reported in very few cases. We present a critical review of this topic, with the report of a patient allegedly diagnosed of SMAS and acute pancreatitis.
Key words: Superior mesenteric artery syndrome. Pancreatitis.
RESUMEN
El síndrome de la arteria mesentérica superior (SAMS) se ha propuesto como una causa rara de obstrucción intestinal alta, resultado de la compresión de la tercera porción del duodeno por la disminución del espacio existente entre la aorta y la arteria mesentérica superior. Los principales factores de riesgo asociados son la pérdida de peso importante, las cirugías de corrección de la columna y anormalidades anatómicas congénitas o adquiridas. Su asociación a pancreatitis aguda ha sido descrita en muy pocos casos. Se presenta una revisión crítica de este tema, a propósito de un caso, presuntamente diagnosticado de SAMS y pancreatitis aguda.
Palabras clave: Síndrome de la arteria mesentérica superior. Pancreatitis.
Case report
A 28-year-old Caucasian woman, with a medical history of cerebral palsy, spastic quadriplegia and seizures treated with phenobarbital, was admitted to the emergency department with a 24 hour history of abdominal distension, bilious vomiting and fever of 38oC. On admission, the patient's vital signs were stable. Physical examination revealed a cachectic young woman (BMI: 18 kg/m2), with a soft, non-tender but distended abdomen, predominantly in the epigastrium.
Under the suspicion of proximal bowel obstruction, a nasogastric tube was inserted, with abundant bilious fluid output, and additional tests were performed: Abdominal X-ray showed dilatation of the stomach without air-fluid levels; laboratory data showed hemoglobin 18 g/dL with MCV 88 fL, white cell count 17,200 with neutrophilia 87 %, amylase 500 U/L (normal < 53 U/L), lipase 628 U/L (normal < 67 U/L), trypsin 6,990 μg/L (normal < 440 μg/L), and amylasuria 480 U/L (normal < 350 U/L); indicators of renal and liver function and electrolytes were normal. Abdominal X-ray after gastografin administration revealed a grossly dilated stomach and duodenum with late passage of contrast to the small intestine.
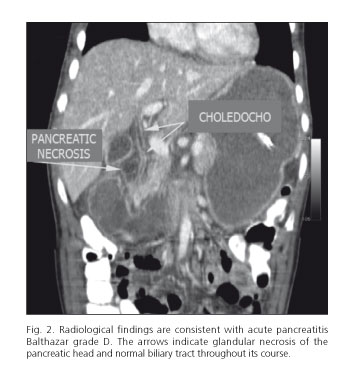
In view of these findings suggestive of partial bowel obstruction at duodenal level, a CT scan performed showed gastric and duodenal distension to the aortomesenteric angle, with a reduced distance between the aorta and SMA (Fig. 1). Glandular necrosis of the head and tail of the pancreas with fat infiltration and free fluid in both paracolic gutters consistent with Balthazar grade D was also observed. The intra- and extra-hepatic biliary tract was normal (Fig. 2).
During admission, the patient was maintained on total parenteral nutrition, and a continuous nasogastric aspiration tube was inserted which yielded a high debit (around 2,000 mL/day) of bilious liquid. Blood cultures were negative and the fever self-limited. Serial determinations of amylasuria oscillated between 1,000 and 4,500 U/L for around 10 days and the condition resolved gradually after 3 weeks.
An abdominal CT scan performed prior to discharge showed resolution of the pancreatitis and dilatation of the stomach and duodenum. To rule out other possible causes of pancreatitis, abdominal US was performed, which was normal, and serology for some viruses (CMV, EBV, herpes virus, measles, rubella and varicella zoster) which were all normal. The patient was discharged and was followed for 1 year with favourable outcome.
Discussion
The superior mesenteric artery syndrome (SMAS) was first described by Von Rokitansky in 1861 as an obstruction of the third portion of the duodenum between the superior mesenteric artery (SMA) and the aorta. In 1921, Wilkie published the first series of 75 cases of high intestinal obstruction due to narrowing of the angle between the SMA and aorta (1). Since then, only isolated cases or small series have been published; thus, the exact prevalence of this syndrome remains unknown. A review of 1,280 barium studies showed only 10 (0.78 %) to be suggestive of SMAS (2).
In normal conditions, the SMA and aorta form a 45-60o angle, which permits the normal passage of the third part of the duodenum. This angle remains open due to the presence of retroperitoneal fat (3,4). When this retroperitoneal fat is reduced, mainly secondary to clinical conditions that generate severe weight loss, compression of the duodenum could result. It has been proposed that an angle below 15 to 20o usually marks the beginning of the obstructive symptoms, which may be acute or chronic (4).
Multiple risk factors associated with SMAS have been reported: Severe weight loss (consumptive syndromes, polytrauma, large extensive burns, anorexia nervosa), diseases of the spine, including orthopaedic correction surgeries and use of corrective corsets ("cast syndrome") and congenital (short Treitz ligament) or acquired (after surgical correction of aneurysms) anatomical abnormalities (5). The BMI of our patient was 18 kg/m2; she presented a deformity of the thoracolumbar spine with marked kyphosis associated with cerebral palsy and spastic quadriplegia.
However, the diagnosis of superior mesenteric artery syndrome must be viewed with caution. The differential diagnosis must be made with motility disorders, particularly of myopathic type of which a megaduodenum could be the only symptom. The most common diseases related to this kind of motility disorder are collagen diseases, especially systemic sclerosis and usually family-type chronic intestinal pseudo-obstruction. Clinical manifestations may range from trivial or dyspeptic symptoms to severe occlusive syndrome and are indistinguishable from those attributed to SMAS. Moreover, disorders considered risk factors for SMAS are known causes of secondary motility disorders (anorexia nervosa, orthopaedic surgery, etc.). In these cases, small bowel motility must be studied to differentiate these two entities (6,7). In our case, given the resolution of the symptoms and the patient's general status, intestinal manometry was not performed.
The association of SMAS and acute pancreatitis is rare. Very few cases have been reported (8-12) in the MEDLINE database; of these only in one, owing to the clinical outcome, was SAMS suggested as a possible aetiology of pancreatitis (9). This was the case of a 16-year-old man with cerebral palsy and multiple episodes of mild pancreatitis initially attributed to "biliary sludge", however after image review, SMAS was suspected and the patient improved progressively, first after an initial weight gain of 4 kg with enteral and parenteral nutrition and, 3 years later, after surgical correction (9). Although the other cases had in common that patients had one or more risk factors for SMAS, the cause of pancreatitis was not established and in all of them, as in our case, abdominal US was performed, and even ERCP in some cases to rule out the main causes of pancreatitis. On occasions, the diagnosis of pancreatitis was doubtful since it was based solely on raised amylase levels, a relatively non-specific finding, which may also occur in duodenal occlusion (13). The mechanism of SMAS pancreatitis is poorly understood; the secondary occlusive postpapillary syndrome due to SMAS may produce a retrograde reflux of bile into the pancreatic duct, which would activate the inflammatory phenomena responsible for pancreatitis. Moreover, pancreatitis could also cause partial paralytic ileus or peripancreatic edema that could produce conflict in the aorto mesenteric space with involvement of the distal duodenum.
In conclusion, the relationship between narrowing of the angle between the SMA and aorta, dilatation of the proximal gastrointestinal tract and acute pancreatitis may have different interpretations, and conservative treatment such as gastroduodenal decompression, correction of electrolyte abnormalities and adequate nutritional support is recommended. Most patients recover satisfactorily, with surgical correction being required only in some cases (14,15).
References
1. Wilkie BP. Chronic duodenal ileus. Am J Med Sci 1927;173:643-50. [ Links ]
2. Jiménez F, Rodríguez F, Puente J, Muñoz R, Adarraga M, Zambrana L. Compresión duodenal por la arteria mesentérica superior: análisis de 10 pacientes. Rev Esp Enferm Dig 2003;95:480-4. [ Links ]
3. Raman SP, Neyman EG, Horton KM, Eckhauser FE, Fishman EK. Superior mesenteric artery syndrome: Spectrum of CT findings with multiplanar reconstructions and 3-D imaging. Abdom Imaging 2012;37:1079-88. [ Links ]
4. Lippl F, Hannig C, Weiss W, Allescher HD, Classen M, Kurjak M. Superior mesenteric artery syndrome: Diagnosis and treatment from the gastroenterologist's view. J Gastroenterol 2002;37:640-3. [ Links ]
5. Merrett ND, Wilson RB, Cosman P, Biankin AV. Superior mesenteric artery syndrome: Diagnosis and treatment strategies. J Gastrointest Surg 2009;13:287-92. [ Links ]
6. Mungan Z, Akyüz F, Bugra Z, Yönall O, Oztürk S, Acar A, et al. Familial visceral myopathy with pseudo-obstruction, megaduodenum, Barrett's esophagus, and cardiac abnormalities. Am J Gastroenterol 2003;98:2556-60. [ Links ]
7. Boeckxstaens GE, Rumessen JJ, de Wit L, Tytgat GN, Vanderwinden JM. Abnormal distribution of the interstitial cells of cajal in an adult patient with pseudo-obstruction and megaduodenum. Am J Gastroenterol 2002;97:2120-6. [ Links ]
8. Gwee K, Teh A, Huang Ch. Acute superior mesenteric artery syndrome and pancreatitis in anorexia nervosa. Australas Psychiatry 2010;18: 523-6. [ Links ]
9. Arbell D, Gross E, Koplewitz B, Vromen A, Bar-Ziv J, Udassin R. Superior mesenteric artery syndrome masquerading as recurrent biliary pancreatitis. Isr Med Assoc J 2006;8:441-2. [ Links ]
10. Cremonte LG, Mantellini E. Associazone di pancreatite acuta ed infarto intestinale da oclussione dell' arteria mesenterica superiore. Minerva Med 1989;80:505-6. [ Links ]
11. Petrosyan M, Estrada JJ, Giuliani S, Williams M, Rosen H, Mason RJ. Gastric perforation and pancreatitis manifesting after an inadvertent nissen fundoplication in a patient with superior mesenteric artery syndrome. Case Rep Med 2009;2009:426162. [ Links ]
12. Ammaturo C, Giardello C, Piscitelli L. The superior mesenteric artery syndrome: A rare cause of acute pancreatitis. Panminerva Med 1988;30:114-7. [ Links ]
13. Feiss JS, Goldenberg AL, Plevy DJ, Luckman GS. Superior mesenteric artery syndrome simulating acute pancreatitis: A case report. Am J Gastroenterol 1976;66:476-9. [ Links ]
14. Richardson W, Surowiec W. Laparoscopic repair of superior mesenteric artery syndrome. Am J Surgery 2001;18:377-8. [ Links ]
15. Alnabulsi BK, Miro JT, Faidah OH, Hamo MA. Laparoscopic duodenojejunostomy omega loop with braun anastomosis as a treatment for superior mesenteric artery syndrome. Saudi Med J 2011;32:188-91. [ Links ]
![]() Correspondence:
Correspondence:
Denisse Joan Sihuay Diburga.
Department of Gastroenterology.
Hospital Universitario Vall d'Hebron.
Passeig de la Vall d'Hebrón, 119-129.
08035 Barcelona, Spain
e-mail: desidi31@hotmail.com
Received: 05-09-2012
Accepted: 10-07-2013











 texto en
texto en