Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 no.2 Madrid feb. 2014
https://dx.doi.org/10.4321/S1130-01082014000200014
Acute necrotizing pancreatitis after transarterial chemoembolization of hepatocellular carcinoma: An usual complication
Pancreatitis aguda necrotizante posterior a quimioembolización transarterial de hepatocarcinoma: una complicación infrecuente
Key words: Key words: Pancreatitis. Hepatocellular carcinoma. Liver cirrhosis.
Palabras clave: Pancreatitis. Hepatocarcinoma. Cirrosis hepática.
Dear Editor,
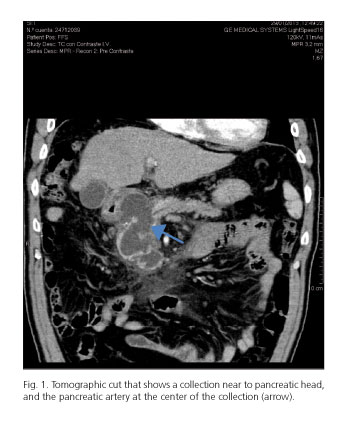
Acute necrotizing pancreatitis following transarterial chemoembolization is an uncommon complication, its incidence being estimated in around 1.7-2% according to various studies. We report the case of a 60-year-old male patient with a diagnosis of both HBV- and alcohol-related cirrhosis. He underwent a second chemoembolization procedure for a relapsing hepatocellular carcinoma, 12.5mm in diameter, in segment VIII (he was not eligible for transplantation because of prostate adenocarcinoma). Forty-eighthours after the procedure he presented with epigastric pain radiating to the back and right hypochondrium in association with febricula at 37.8 oC, with lab tests showing serum amylase of 896mU/ml, C-reactive protein of 122.7mg/l, total bilirubin of 1.64mg/dl (direct bilirubin was 0.83mg/dl), GGT of 147IU/L, alkaline phosphatase of 154U/L, and mildly impaired coagulation (PT, 16.5 seconds; INR, 1.47), with normal CBC and transaminases. Abdominal, IV contrast-enhanced tomography revealed several collections: an extrapancreatic one surrounding the head of the pancreas, 50mm in size, and another one in the uncinate process, 43mm in size, associated with a complication of acute necrotizing pancreatitis (Fig. 1). Following intestinal rest, hydration, intravenous analgesia, and empiric antibiotic therapy with meropenem 1g every 8hours for 7days, the disease had a favorable evolution, and both amylase and C-reactive protein levels returned to normal. Tomographic follow-up at 3months showed that collections had shrunk by 50% in size. Similarly, no uptake was identified by the chemoembolized hepatocellular carcinoma.
Discussion
Transarterial chemoembolization is a first-line therapy for hepatocellular carcinoma. Its mechanism of action consists of compromising the tumor's arterial inflow and instilling a chemotherapy agent (usually doxorubicin) in order to bring about tumor necrosis (1). Following the procedure post-chemoembolization syndrome is commonly experienced, which is characterized by fever, abdominal pain, nausea/vomiting, and occasionally impaired liver function. Unusual complications may develop, such as noted by Xia Jinglin et al. in their study of 1,348patients, with an incidence of rare complications of 2.68% that ranged from spontaneous carcinoma rupture to hepatic artery occlusion (0.15% and 1.99%); the fact stands out that no acute necrotizing pancreatitis cases was identified in this large series (2). This is an uncommon condition, and studies estimate an incidence of 1.7-2% (clinical pancreatitis) as compared to 40% for biological pancreatitis, defined as hyperamylasemia with no clinical impact (3-5). This complication results from a retrograde injection of the chemotherapeutic, embolizing agent into pancreatic arteries, giving rise to ischemic pancreatitis (6). Amylasemia testing after chemoembolization is controversial -some authors do not recommend its routine use but in patients experiencing severe abdominal pain unrelated to post-chemoembolization syndrome (7,8).
Management in such situation is similar to that of any acute pancreatitis; prophylactic antibiotic use is indicated when severe necrosis or superinfection is present (9). In our case we used meropenem because of the presence of necrotic collections, febricula, and markedly elevated C-reactive protein levels, in addition to cirrhosis-related immune deficiency. Up to 57% of patients may have such collections progressing to pseudocysts; those located at the neck and head should be assessed for drainage or surgical resection when symptomatic (10). In our case all collections evolved satisfactorily with a significant decrease in size, and the patients remained asymptomatic after 3months of follow-up.
Juan Manuel Alcívar-Vásquez,Guillermo Ontanilla-Clavijo,
María Teresa Ferrer-Ríos and Juan Manuel Pascasio-Acevedo
Department of Digestive Diseases. Hospital Universitario Virgen del Rocío.
Sevilla, Spain
References
1. Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: Chemoembolization inproves survival. Hepatology 2003;37:429-42. [ Links ]
2. Xia J, Ren Z, Ye S, Sharma D,Lin Z,Gan Y, et al. Study of severe and rare complicacations of transarterial chemoembolization (TACE) for liver cancer. Eur J Radiol 2006;59:407-12. [ Links ]
3. Stefanini GF, Amoratu P, Biselli M, Mucci F, Celi A, Arienti V, et al. Efficacy of transarterial targeted treatments on survival of patients with hepatocellular carcinoma. An italian experience. Cancer 1995;75:2427-34. [ Links ]
4. Marchiari L, Mansueto GC, Nifosi F, Bortolosi L, Dal Dosso I, Facci E, et al. The treatment of hepatocellular carcinoma by chemoembolization. Chir Ital 1994;46:17-22. [ Links ]
5. Khan KN, Nakata K, Shima M, Kusumoto Y, Nobuko I, Koji T, et al. Pancreatic tissue damage by transarterial embolization for hematoma. Dig Dis Sci 1993;38:65-70. [ Links ]
6. Ozçinar B, Güven K, Poyanli A, Ozden I. Necrotizing pancreatitis alter transcatheter arterial chemoembolization for hepatocellular carcinoma. Diagn Interv Radiol 2009;15:36-8. [ Links ]
7. Chey V, Chopin-laly X, Micol C, Lepiliez V, Forestier J, Lombard-bohas C, et al. Acute pancreatitis alter transcatheter arterial chemoembolization for liver metastases of carcinoid tumors. Clin Res Hepatol Gastroenterol 2011;35:583-5. [ Links ]
8. López-Benítez R, Radeleff BA, Barragán-Campos HM, Noeldge G, Grenacher L, Richter GM, et al. Acute pancreatitis alter embolization of liver tumors: Frequency and associated risk factors. Pancreatology 2007;7:53-62. [ Links ]
9. Baker S. Diagnosis and management of acute pancreatitis. Crit Care Resusc 2004;6:17-24. [ Links ]
10. Working Party of the British Society of Gastroenterology, Association of Surgeons of Great Britain and Ireland, Pancreatic Society of Great Britain and Ireland, Association of Upper GI Surgeons of Great Britain and Ireland. UK guidelines for the management of acute pancreatitis. Gut 2005;54(Supl. 3):iii1-9. [ Links ]











 texto en
texto en