Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 no.2 Madrid feb. 2014
https://dx.doi.org/10.4321/S1130-01082014000200015
Ectopic hepatocellular carcinoma in the gallbladder
Hepatocarcinoma ectópico en vesícula biliar
Key words: Hepatocellular carcinoma. Gallbladder. Ectopic tissue.
Palabras clave: Carcinoma hepatocelular. Vesícula biliar. Tejido ectópico.
Dear Editor,
We report on a 49-year-old female patient with an uneventful clinical history except for subclinical hypothyroidism. She visited our hospital for right hypochondrium pain with mass sensation and mild jaundice. From a biochemical standpoint normal carcinoembryonic antigen levels (0.50ng/l) and highly elevated alpha-fetoprotein levels (13,785ng/ml) stand out. HBV and HCV serology was negative.
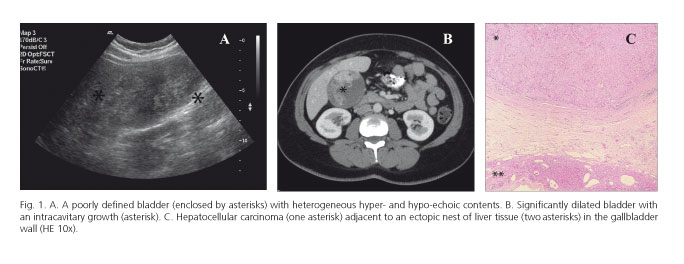
An abdominal ultrasonogram and a computerized axial scan are performed, which reveal a dilated, huge (15x5x4 cm) gallbladder with a 12-cm polypoid mass inside (Fig. 1 A and B). In view of these findings, and suspecting a gallbladder carcinoma, a cholecystectomy and hepatectomy for segments IVB and V is carried out through extended midline laparotomy.
Histologically, the mass was a well-differentiated hepatocellular carcinoma growing like a polyp within the gallbladder. Next to this neoplasm healthy ectopic liver (EL) nests may be seen on the gallbladder wall (Fig. 1C). Resected liver fragments show no neoplastic or preneoplastic findings. From all the above a diagnosis of well-differentiated liver cell carcinoma on EL attached to the gallbladder is made.
The postoperative course is favorable and uneventful, and the patient remains -over 3 years after surgery- asymptomatic with no evidence of local or distant relapse.
Discussion
EL is defined as the presence of normal liver tissue detached from the liver (1). It has been seen in numerous sites, both near the liver -gallbladder and hepatic ligament- and far from it -peritoneum, retroperitoneum and even the chest (2,3). From a pathogenic point of view, the cause of EL seems to be an aberrant migration of liver cells during embryonic development; EL has the same risk factors as the liver for hepatocellular carcinoma (1,4-6). However, risk factors such as hepatitis B or C and cirrhosis seem more uncommon -in fact, only 32% of ectopic liver cell carcinomas had a cirrhotic background (7), and two of 21 cases reported by Arakawa et al. had positive viral serology (5), which suggests EL is of itself apt to undergo malignant transformation (6). The reasons for this greater degenerative ability remain unknown; however, deficient blood flow through the hepatic artery and an absent connection with the portal and biliary systems are thought to be triggering factors, possibly as a result of long-term exposure to carcinogenic substances (1,5,7).
From a prognostic perspective these patients usually have a significantly better clinical outcome as compared to individuals with hepatocellular carcinoma of the liver, and tumor excision is often curative (1,8). Thus, of the three patents reported by Leone et al. two were still living four years after surgery (1).
To conclude, the presence of EL in laparoscopies performed for other reasons, or more rarely its clinical suspicion from imaging techniques, makes excision mandatory given its greater carcinogenic potential versus the liver.
Juan Segura-Sánchez1, Yolanda Torres-Domínguez2 and Esther Ruiz-García3
1Laboratory. Section of Pathology
2Internal Medicine. Section of Digestive Diseases, and
3Department of Radiodiagnosis
Hospital San Juan de Dios del Aljarafe. Bormujos, Sevilla. Spain
References
1. Leone N, De Paolis P, Carrera M, Carucci P, Musso A, David E, et al. Ectopic liver and hepatocarcinogenesis: Report of three cases with four years' follow-up. Eur J Gastroenterol Hepatol 2004;16:731-5. [ Links ]
2. Lundy J, Johnson E, Edwards K, Rivera D. Laparoscopic management of gallbladder-associated ectopic liver. JSLS 2005;9:485-7. [ Links ]
3. Martinez CA, de Resende HC Jr, Rodrigues MR, Sato DT, Brunialti CV, Palma RT. Gallbladder-associated ectopic liver: A rare finding during a laparoscopic cholecystectomy. Int J Surg Case Rep 2013;4:312-5. [ Links ]
4. Fraser CG. Accessory lobes of the liver. Ann Surg 1952;135:127-9. [ Links ]
5. Arakawa M, Kimura Y, Sakata K, Kubo Y, Fukushima T, Okuda K, et al. Propensity of ectopic liver to hepatocarcinogenesis: Case reports and a review of the literature. Hepatology 1999;29:57-61. [ Links ]
6. Christine P, Caygill, Piers A. Ectopic liver and hepatocarcinogenesis. Eur J Gastroenterol Hepatol 2004;16:727-9. [ Links ]
7. Miyake T, Hoshino S, Yoshida Y, Aisu N, Tanimura S, Hisano S, et al. Multiple ectopic hepatocellular carcinomas arising in the abdominal cavity. Case Rep Gastroenterol 2012;6:629-34. [ Links ]
8. Asselah T, Condat B, Cazals-Hatem D, Hassani Z, Bernuau J, Groussard O, et al. Ectopic hepatocellular carcinoma arising in the left chest wall: A long-term follow-up. Eur J Gastroenterol Hepatol 2001;13:873-5. [ Links ]











 texto en
texto en