My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 n.7 Madrid Jul./Aug. 2014
PICTURES IN DIGESTIVE PATHOLOGY
Pancreatic dysontogenetic cysts
Quistes disontogénicos pancreáticos
Eduardo Rodrigues-Pinto1, Pedro Pereira1, Rui Cunha2 and Guilherme Macedo1
1Gastroenterology Department and 2Radiology Department. Centro Hospitalar São João. Porto, Portugal
Case report
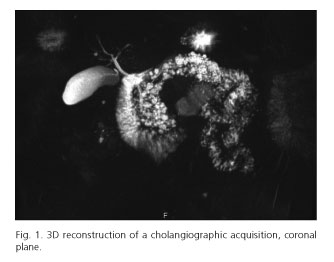
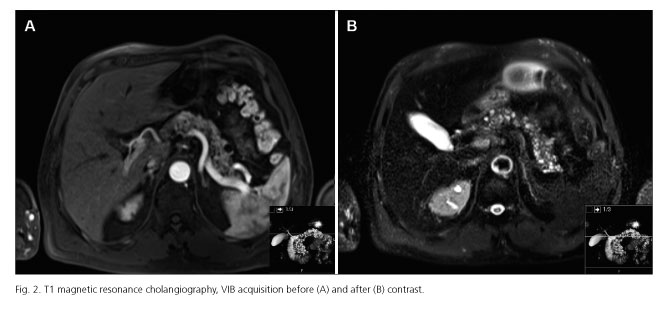
A male patient, 57-years-old, was submitted to abdominal imaging for study of urinary complaints. He had no complaints suggestive of pancreatic disease, no history of smoking, alcohol consumption or family history of pancreatic diseases. Abdominal imaging revealed multiple hypodense lesions mainly on the body and tail of the pancreas, consistent with cystic pancreatic formations (Figs. 1 and 2) with associated parenchymatous calcifications without Wirsung dilatation or solid nodular lesions suggestive of malignancy. He also had multiple renal cysts. Remaining exams revealed no other changes. Pancreatic cysts are present in 2.4-13.5 % of patients without known pancreatic disease (1). Accurate categorization is important since some of them have malignant potential and should be resected. Pancreatic cysts are broadly classified as congenital-developmental cysts, retention cysts, duplication cysts, pseudocysts, neoplastic cysts and parasitic cysts (2). An important differential diagnosis is branch duct intraductal papillary mucinous neoplasm (IPMN). It is accepted that true cysts occur as a result of developmental anomalies related to the sequestration of primitive pancreatic ducts. In the presenting case, there was no previous history of pancreatitis or other pancreatic diseases, the patient was asymptomatic and also had renal involvement by cysts. His pancreatic cysts were multiple, small and diffusely involve the body and tail of pancreas. IPMNs are an important differential diagnosis, due to prognosis implications; however, Wirsung had a normal calibre, with no dilatation. Dysontogenetic pancreatic cysts are a very rare entity that may occur singly or in association with renal cysts, liver, central nervous system or retinal abnormalities (3). Currently there are no well-defined diagnostic criteria for dysontogenetic pancreatic cysts. Therefore it is important to always consider differential diagnosis, namely IPMNs, due to different needs of follow-up.
References
1. de Jong K, Nio CY, Mearadji B, Phoa SS, Engelbrecht MR, Dijkgraaf MG, et al. Disappointing interobserver agreement among radiologists for a classifying diagnosis of pancreatic cysts using magnetic resonance imaging. Pancreas 2012;41:278-82. [ Links ]
2. Rowe MI, O'Neill JA Jr, Grosfeld JL, Fonkalsrud EW, Coran AG, editors. Essentials of pediatric surgery. Disorders of the pancreas. Louis MO: MosbyYear Book; 1995. p. 663-74. [ Links ]
3. Nygaard KK, Walters W. Polycystic disease of the pancreas (Dysontogenetic cysts): Report of a case with partial pancreatectomy. Ann Surg 1937;106:49-53. [ Links ]