Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 no.8 Madrid dic. 2014
LETTERS TO THE EDITOR
Tetany and convulsions: onset symptoms in Crohn's disease
Tetania y convulsiones, síntomas de debut de la enfermedad de Crohn
Key words: Crohn's disease. Malabsorption. Hypocalcemia.
Palabras clave: Enfermedad de Crohn. Malabsorción. Hipocalcemia.
Dear Editor,
The clinical presentation of Crohn's disease is widely variable. Chronic diarrhea, abdominal pain and weight loss are the most common onset symptoms. Rarely, the clinical presentation includes symptoms secondary to global or partial malabsorption of nutrients, including vitamins or trace elements, as in the following case report.
Case report
A 64-years-old male, with no remarkable history in terms of substance abuse or other diseases, was referred to the emergency department after an episode of generalized tonic-clonic movements during several minutes. One week before, he had stiff limbs and occasional muscle cramps. Physical examination showed an altered level of consciousness (stupor), sweaty and hypertonia of upper and lower limbs. Furthermore, Trousseau and Chvostesk signs were assessed and were positive. On the other hand, vital signs were normal, as well as cardiopulmonary and abdominal examination. Laboratory parameters showed leukocytosis (14.6 K/µL, [4.6-10.2 K/µL]) and hypokalemia (2.5 mEq/L [3.5-5 mEq/L]). However, other parameters such as hemoglobin, hematocrit, glucose, urea, creatinine, and sodium were normal. In this context, brain CT scan and electroencephalogram were urgently carried out, showing no abnormalities. During his hospitalization, deepen laboratory tests confirmed mild leukocytosis and hypokalemia, and showed hypoproteinemia (6.3 g/dL [(6.6-8.7 g/dL]), hypocalcemia (calcium 3.9 mg/dL [8.5-10.5 mg/dL], ionized calcium 1.99 mg/dL [4.48-4.92 mg/dL]), and hypomagnesemia (1 mg/dL [1.58-2.55 mg/dL]). Other parameters, including C-reactive protein, and renal and liver profiles were normal. Parathyroid hormone levels were raised (124.5 pg/mL [5-65 pg/mL]) and serum 25-hydroxyvitamin D3 levels were decreased (10.1 nmol/l [75-250 nmol/l]). Otherwise, typical malabsorptive syndromes, such as celiac disease, were ruled out.
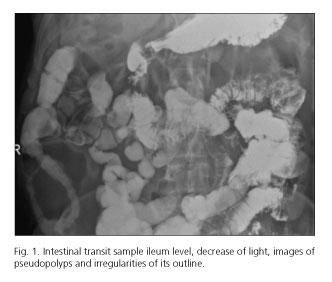
In this scenario, the patient was asked again about gastrointestinal symptoms and, this time, he commented a decrease in fecal consistency in the last 3-4 years with no abdominal pain or other symptoms. Therefore, a colonoscopy was indicated, showing an active Crohn's disease with extensive involvement of ileum. Additionally, small bowel barium radiology and abdominal CT scan were performed (Fig. 1). No alterations were observed in duodenum and jejunum. Thus, clinical and laboratory abnormalities were resolved after appropriate treatment with systemic corticosteroids, together with calcium and magnesium. However, the patient developed a corticodependence over time, introducing azathioprine in the maintenance treatment. Finally, the patient achieved a steroid-free remission and remained asymptomatic with normal levels of magnesium and calcium.
Discussion
Crohn's disease, especially involving the small intestine, is frequently associated with nutrient deficiencies. This latter is usually subclinical but, occasionally, can cause weight loss, growth retardation, fatigue, osteopenia, muscle cramps, anemia, impaired immunity and, even, tetany and seizures. On the other hand, magnesium deficit has been reported in 14-33 % of Crohn's disease patients, calcium deficit in 14 % and vitamin D decreased levels in 75 % (1).
Magnesium is absorbed in the proximal jejunum and ileum. Hypomagnesemia can be caused by decreased intake, malabsorption, and/or increased intestinal losses. The symptoms are usually noted when the magnesium plasma levels are less than 1.2 mg/dL, being muscle cramps, paresthesia, seizures, tetany and cardiac abnormalities the most common symptoms. Furthermore, hypomagnesemia has been linked to severe hypocalcemia (2,3). On the other hand, vitamin D is essential to absorb calcium in small bowel. Similarly to hypomagnesemia, gastrointestinal malabsorption and poor intake are the main causes of the vitamin deficiency. Over time, vitamin D deficit generates hypocalcemia and, consequently, a secondary increase in the parathyroid hormone levels (4-7). There are a few reported cases emphasizing on the clinical consequences of magnesium and calcium deficiency in Crohn's disease, being the surgically short bowel syndrome one of the main causes (8-11).
In our case report, we observed how symptoms like tetany and seizures were related to hypomagnesemia, similar to other reported cases; hypomagnesemia was probably secondary to gastrointestinal malabsorption, and hypocalcemia was consequence of the deficit of magnesium and vitamin D. Other causes of malabsorption, such as celiac disease, were reasonably ruled out. Therefore, our proposal is to focus on the importance of nutritional deficiencies in the clinical management of patients with Crohn's disease and, in particular, on the deficit of magnesium and/or calcium in patients with seizures or tetany.
Marina Millán-Lorenzo, Paula Ferrero-León, Manuel Castro-Fernández,
Javier Ampuero-Herrojo, María Rojas-Feria and Manuel Romero-Gómez
Unit for the Clinical Management of Digestive Diseases & CIBERehd
Hospital Universitario de Valme. Sevilla, Spain
References
1. Dieleman LA, Heizer WD. Nutritional Issues in inflammatory bowel disease. Gastroenterol Clin N Am 1998;27:435-51. [ Links ]
2. Topf JM, Murray PT. Hypomagnesemia and hypermagnesemia. Rev Endocr Metab Disord 2003;4:195-206. [ Links ]
3. Galland L. Magnesium and inflammatory bowel disease. Magnesium 1988;7:78-83. [ Links ]
4. McCarthy D, Duggan P, O'Brien M, Kiely M, McCarthy J, Shanahan F, et al. Seasonality of vitamin D status and bone turnover in patients with Crohn's disease. Aliment Pharmacol Ther 2005; 21:1073-83. [ Links ]
5. Haderslev K, Jeppesen P, Sorensen H, Mortensen PB, Staun M. Vitamin D status and measurement of markers of bone metabolism in patients with small intestinal resection. Gut 2003;52:653-8. [ Links ]
6. Thomas KK, Lloyd-Jones DM, Thadhani RI, Shaw AC, Deraska DJ, Kitch BT, et al. Hypovitaminosis D in medical inpatients. N Engl J Med 1998;338:777-83. [ Links ]
7. Chapuy MC, Preziosi P, Maamer M, Arnaud S, Galan P, Hercberg S, et al. Prevalence of vitamin D insufficiency in an adult normal population. Osteoporos Int 1997;7:439-43. [ Links ]
8. Roitg I, Jamard B, Constantin A, Cantagrel A, Mazières B, Laroche M. Severe refractory hipocalcemia in patients with enteropaty: Consider hypomagnesemia. Joint Bone Spine 2004;71:251-3. [ Links ]
9. Fagan C, Phelan D. Severe convulsant hypomagnesaemia and short bowel syndrome. Anaesth Intensive Care 2001;29:281-3. [ Links ]
10. Fernández R E, Camarero G E. Paciente con enfermedad de Crohn y convulsiones por hipomagnesesia. Nutr Hosp 2007;22:720-2. [ Links ]
11. Kelly AP, Robb BJ, Gearry RB. Hipocalcemia and hypomagnesemia: A complication of Crohn's disease. N Z Med J 2008;121:77-9. [ Links ]











 texto en
texto en