Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.107 no.3 Madrid mar. 2015
Quality standards in 480 pancreatic resections: a prospective observational study
Estándares de calidad en 480 resecciones pancreáticas: estudio prospectivo observacional
Francisco Javier Herrera-Cabezón, Pablo Sánchez-Acedo, Cruz Zazpe-Ripa, Antonio Tarifa-Castilla and José Miguel Lera-Tricas
Unit of Hepato-bilio-pancreatic Surgery. Complejo Hospitalario de Navarra. Pamplona, Navarra. Spain
ABSTRACT
Pancreatic resection is a standard procedure for the treatment of periampullary tumors. Morbidity and mortality are high, and quality standards are scarce in our setting. International classifications of complications (Clavien-Dindo) and those specific for pancreatectomies (ISGPS) allow adequate case comparisons. The goals of our work are to describe the morbidity and mortality of 480 pancreatectomies using the international classifications ISGPS and Clavien-Dindo to help establish a quality standard in our setting and to compare the results of CPD with reconstruction by pancreaticogastrostomy (1,55) versus 177 pancreaticojejunostomy). We report 480 resections including 337 duodenopancreatectomies, 116 distal pancreatectomies, 11 total pancreatectomies, 10 central pancreatectomies, and 6 enucleations. Results for duodenopancreatectomy include: 62 % morbidity (Clavien ≥ III 25.9 %), 12.3 % reinterventions, and 3.3 % overall mortality. For reconstruction by pancreaticojejunostomy: 71.2 % morbidity (Clavien ≥ III 34.4 %), 17.5 % reinterventions, and 3.3 % mortality. For reconstruction by pancreaticogastrostomy: 51 % morbidity (Clavien ≥ III 15.4%), 6.4 % reinterventions, and 3.2 % mortality. Differences are significant except for mortality. We conclude that our series meets quality criteria as compared to other groups. Reconstruction with pancreaticogastrostomy significantly reduces complication number and severity, as well as pancreatic fistula and reintervention rates.
Key words: Pancreaticoduodenectomy. Pancreatectomy. Morbidity. Mortality. Quality Indicators. Health Care.
RESUMEN
Introducción: la resección pancreática es un procedimiento estándar para el tratamiento de los tumores periampulares. La morbimortalidad es elevada y los estándares de calidad en nuestro medio son escasos. Las clasificaciones internacionales de las complicaciones Clavien-Dindo y las específicas de las pancreatectomías (ISGPS) permiten una adecuada comparación de casuísticas.
Objetivos: los objetivos de nuestro trabajo son describir la morbimortalidad de 480 pancreatectomías utilizando las clasificaciones internacionales ISGPS y Clavien-Dindo para contribuir al establecimiento de un estándar de calidad en nuestro medio, y comparar los resultados de la DPC con reconstrucción mediante pancreaticogastrostomía (1.55) frente a la pancreaticoyeyunostomía (177).
Métodos: presentamos 480 resecciones que incluyen 337 duodenopancreatectomías, 116 pancreatectomías distales, 11 pancreatectomías totales, 10 pancreatectomías centrales y 6 enucleaciones.
Resultados: los resultados en la duodenopancreatectomía son: 62 % de morbilidad (Clavien ≥ III 25,9 %), 12,3 % de reintervenciones y 3,3 % de mortalidad global. En las reconstrucción con pancreaticoyeyunostomía: 71,2 % de morbilidad (Clavien ≥ III 34,4 %), 17,5 % de reintervenciones y 3,3 % de mortalidad. En la reconstrucción con pancreaticogastrostomía: 51 % de morbilidad (Clavien ≥ III 15,4 %), 6,4 % de reintervenciones y 3,2 % de mortalidad, las diferencias son significativas, excepto en la mortalidad.
Conclusiones: concluimos que nuestra serie cumple criterios de calidad en comparación con la experiencia de otros grupos. La reconstrucción con pancreaticogastrostomía disminuye significativamente el número de complicaciones, su gravedad, la tasa de fístula pancreática y las reintervenciones.
Palabras clave: Pancreaticoduodenectomía. Pancreatectomía. Morbilidad. Mortalidad. Indicadores de calidad. Sistema sanitario.
Abbreviation list:
ISGPS: International Study Group of Pancreatic Surgery;
CDP: Cephalic duodenopancreatectomy;
DP: Distal pancreatectomy;
ASA: American Society of Anesthesiologists;
BMI: Body mass index;
PF: Pancreatic fistula;
DGE: Delayed gastric emptying;
PJ: Pancreaticojejunostomy;
PG: Pancreaticogastrostomy;
TP: Total duodenopancreatectomy;
ERAS: Enhanced recovery after surgery;
CP: Central pancreatectomy;
GIST: Gastrointestinal stromal tumors;
ICU: Intensive care unit.
Introduction
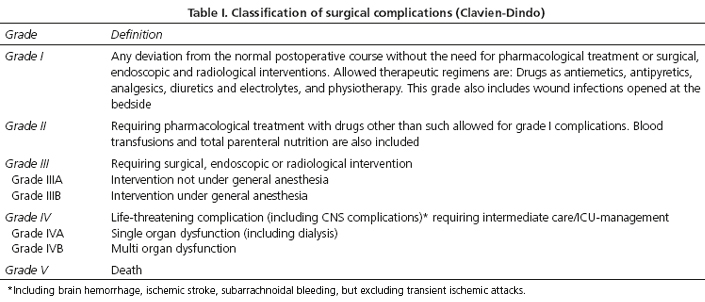
The increased number of pancreatic resections in specialized units has led to improved morbidity and mortality rates. Despite this, in our health care system, we have no postoperative quality standards specific for the two procedures most commonly used: Cephalic duodenopancreatectomy (CDP) and distal pancreatectomy (DP). Duodenopancreatectomy-related morbidity and mortality has been shown to decrease as the number of procedures per surgeon and hospital increases, even if limits are rather vague (1-4). Furthermore, quality references available mostly derive from series in health care environments where high-volume centers predominate (5). The description of complications as recently standardized by the ISGPS (6-8) and Clavien-Dindo (9,10) classifications (Table I) has been scarcely used in Spanish publications (5,11-14). This fact precludes case comparisons and hinders the establishment of quality standards adapted to our health care setting.
The goals of our work are to describe the morbidity and mortality of 480 pancreatectomies using the international classifications ISGPS and Clavien-Dindo in order to help establish a quality standard in our setting, and to compare the results of CDP with reconstruction by pancreaticogastrostomy versus pancreaticojejunostomy.
Patients and methods
All patients undergoing pancreatic resection between June 1994 and June 2014 were included. Data were prospectively entered into a proprietary FileMaker Pro 3.0 database on patient discharge, also including readmissions within 30 days of discharge. Seventeen variables were studied: Demography, ASA classification, body mass index (BMI), diagnosis, surgical procedures, surgery date, surgical complications according to the ISGPS classification, pancreatic fistula (PF), delayed gastric emptying (DGE), bleeding and Clavien-Dindo, reintervention, infection, admission to ICU, need for radiological/endoscopic or transfusion procedures, mortality and its cause at 30 days or at any time point for inpatients, and hospital stay. Complications during readmission were added to overall results. Data before 2008 were adjusted to international classifications on a case-by-case basis, and reviewed by the primary author. Complications were deemed to be minor if Clavien I-II, and major if Clavien ≥ III-A, including mortality. All patients signed an informed consent according to the ethical guidelines provided by the Declaration of Helsinki as revised in 1975.
According to pancreatic resection type patients were included in the following groups: CDP in two periods - from June 1994 to April 2008, where pancreatic reconstruction was performed by duct-to-mucosa pancreaticojejunostomy using a silicone drain (PJ) (15); and from April 2008 to June 2014, where the reconstruction of choice was by two-plane invaginated pancreaticogastrostomy as described by Delcore (PG) (16). Both cohorts were used to compare morbidity, mortality, and postoperative stay.
Total duodenopancreatectomy (TP), where the whole pancreas is excised together with the duodenum and spleen, hence no suture or section border is present.
Distal, body-tail or subtotal pancreatectomy, grouped together as distal pancreatectomies (DP) and categorized into two subgroups: Urgent (pancreatitis and trauma) or elective.
Central pancreatectomy (CP), where a section of the proximal pancreas is performed and a portion of the pancreatic body is excised, with an anastomosis of the distal pancreas to the jejunum or stomach.
Pancreatic enucleation, meaning the excision of a small pancreatic fragment around the lesion. Data will be presented according to pancreatic resection technique and comparing PJ versus PG.
Preoperative study, technique, and postoperative care were standardized, and from 2008 on a clinical path based on a postoperative multimodal rehabilitation protocol (17) for CDP was implemented.
Statistical study
Mean and standard deviation, and median plus range were used for the descriptive analysis. A cohort comparison study was carried out for PJ versus PG. Qualitative variables were analyzed using the chi-squared and Fisher tests, whereas Student's t test or the Mann Whitney U test was used for quantitative variables. Data were analyzed with the SPSS 22.0 statistical package, and a p value of 0.05 was considered statistically significant for all comparisons.
Results
In all, 480 patients were included, and 5,893 data for all 17 variables under study were obtained; missing data amounted to 207 (3.2 %) (128 BMI and 53 DGE extent). Surgical technique was: 337 CDP (177 PJ, 155 PG, 5 excluded), 116 DP (11 urgent, 105 elective), 11 TP, 10 CP, and 6 enucleations (Fig. 1).
CDP
Of all 337 CDPs 5 were excluded from the study because of associated major surgery (2 total gastrectomies, 2 major hepatectomies, and 1 gunshot injury) (Table II).
Diagnoses included: 119 pancreatic adenocarcinomas, 60 papillary adenocarcinomas, 34 cholangiocarcinomas, 34 chronic pancreatitis, 19 mucinous intraductal papillary neoplasms, 17 papillary adenomas, 15 neuroendocrine tumors, 8 duodenal adenocarcinomas, 5 serous cystadenomas, 3 metastases (2 from renal carcinoma, 1 from hemangiopericytoma), 2 mucinous cystadenomas, 2 cystadenocarcinomas, 14 others (3 ampullary stenoses, 3 colonic cancers, 2 biliary stenoses, 1 Castleman's disease, 1 gallbladder cancer, 1 gastric cancer, 1 lymphoma, 1 hamartoma, 1 duodenal GIST).
Of all CDPs, 289 (87 %) were performed for tumors: 251 (75.6 %) malignancies, 33 (10 %) premalignant lesions, and 5 (1.5 %) benign growths; the remaining 43 were for inflammatory conditions (13 %).
Complications
A total of 206 patients (62 %) had at least one complication. Minor complications amounted to 121 (36.4 %) and major ones to 85 (25.5 %). Of patients with major complications, 25 (7.5 %) were III-A (22 percutaneous drains, 3 visceral artery aneurysm embolizations); 19 (5.7 %) were III-B (17 cases from reintervention and 2 radiographic procedures under general anesthesia); 18 (5.4 %) patients were IV-A (11 bleeding events with hemodynamic failure -5 GI, 5 visceral arteries, 1 hemoperitoneum- 7 reinterventions that required admission in an ICU); 12 (3.6 %) were IV-B (12 reoperated patients with organ failure).
Mortality (Clavien V) was 11 patients (3.3 %), and causes included: 5 abdominal sepsis, 3 visceral artery bleeding, 1 hemoperitoneum, 1 bronchial aspiration, and 1 cardiac arrest from ventricular fibrillation. Of those who died, 4 were reoperated and 4 had pancreatic fistula.
Pancreatic fistula
PFs are described using two classifications: ISGFP and Clavien's. In 76 patients (22.9 %) PF was identified as per the ISGPF: A 18 (5.4 %), B 27 (8.1 %), C 31 (9.4 %). According to Clavien's classification: Grade I-II 28 (8.4 %), III 25 (7.5 %), and IV-V 25 (6.9 %). Of all 76 patients with PF, 27 (35.5 %) were re-intervened versus 14 (5.7 %) of those with no PF (p < 0.001); 4 patients died with PF (5.2 %) versus 7 (2.7 %) without PF (p = 0.27); 7 patients with PF (9.2 %) developed visceral artery bleeding versus 4 (1.5 %) without PF (p < 0.001).
Delayed gastric emptying
Our data from before the publication of the ISGPS classification were adapted to said system. In this process DGE was estimated to have an incidence of 100 %, but extent could only be obtained for 53 patients (15.9 %). The overall incidence of DGE was 114 (34.3 %), this being the most common complication. Its association with other abdominal complications was: 47 (64 %) PFs with DGE and 67 (35.4 %) PFs without DGE (p < 0.001); 41 (36 %) intra-abdominal abscesses with DGE and 27 (12.3 %) without DGE (p < 0.001); 27 (23.6 %) reinterventions with DGE and 14 (12.2%) without DGE (p < 0.001).
Reintervention
There were 41 reoperated patients (12.3 %), including readmissions within 30 days, which required 59 reinterventions (28 one, 8 two, 5 three). Causes, multiple at times, included: 26 grade-C pancreatic fistulas, 25 bleeding events, 22 intra-abdominal infections, and 1 evisceration. Reintervention-related mortality was 4 patients (9.7 %).
Readmission
The causes for all 30 (9 %) readmissions included: 10 digestive intolerance, 9 bleeding, 8 fever, and 3 abscesses that required percutaneous drainage.
Stay
Mean stay was 20 (17.14) days, with a median of (6-144) days. For patients with no complications mean stay was 10 (3.84) days; for Clavien < III 19.7 (9.03) days (p < 0.001); for Clavien ≥ III 36 (24.68) days (p < 0.001). For patients with PF it was 33.6 (23.51) days versus 16.2 (12.3) days without PF (p < 0.001).
Comparison between PJ and PG
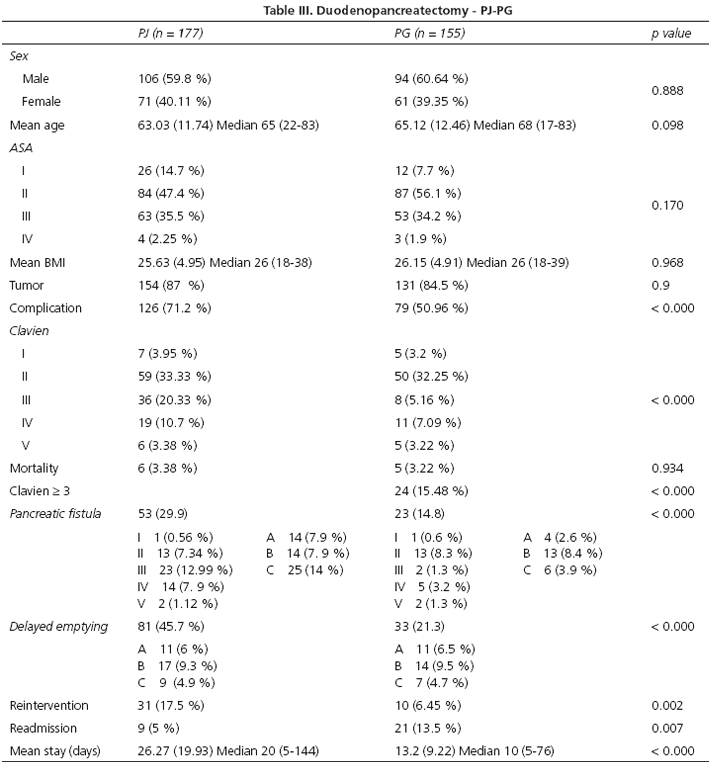
The two cohorts show no significant differences in demography, operative risk or diagnosis. The procedures were performed by the same surgeons and two differences existed as regards the technique, namely the type of pancreatic anastomosis (PG vs. PJ); also, 87 (49.1 %) patients with PJ benefited from pyloric preservation. All PGs included antrectomy (Table III).
The overall incidence of complications was significantly higher for PJ (71.2 %) versus PG (50.9 %) (p < 0.000). Differences were not significant for mild cases -37.2 % for PJ and 35.5 % for PG. In contrast, differences were significant for severe events -34.4 % for PJ and 15.5 % for PG (p < 0.000). This decrease in severe complications parallels the incidence of PF -29.9 % for PJ and 14.8 % for PG (p < 0.000). Differences are not only global but also regarding PF severity (Clavien ≥ III) -22 % for PJ and 5.8 % for PG. Regarding DGE, numbers are 45.7 % for PJ and 21.3 for PG (p < 0.000), which reflects the association between abdominal complications and DGE.
Mortality was similar in both groups -3.3 % for PJ and 3.2 % for PG. The only variable where PG obtained poorer results was readmission rate within 30 days -13.5 % versus 5 % for PJ (p < 0.007).
Distal pancreatectomy
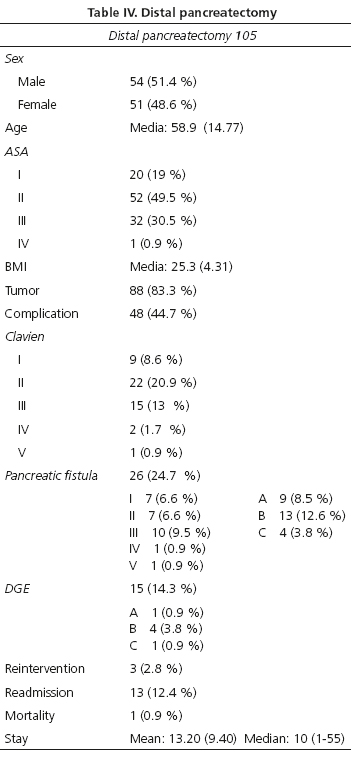
A total of 116 DPs were performed -105 scheduled vs. 11 urgent procedures (Table IV).
Diagnoses included: 25 cystic tumors, 22 neuroendocrine tumors, 20 pancreatic adenocarcinomas, 17 complicated chronic pancreatitides (11 associated with total gastrectomy, 4 associated with colectomy), 3 renal carcinoma metastases, 2 solid papillary tumors, and 1 paraganglioma.
Complications
Only complications deriving from DP were included; 48 patients (44.7 %) had at least one complication, 31 (29.5 %) were mild and 17 (14.7 %) were severe. Of these, 11 (10.4 %) involved percutaneous draining of fistulas or intra-abdominal abscesses. Reintervention was necessary for 3 patients (1 early hemoperitoneum, 1 abscess, 1 ischemic cecal perforation). One patient died from myocardial infarction.
Pancreatic fistula
PF (ISGPF classification) developed in 26 patients (24.8 %) -grade A or B in 22 (21 %) and grade C in 4 (3.8 %). According to Clavien's classification 14 subjects (13.2 %) developed mild complications and 12 (11.3 %) developed severe complications. Seven (6.6 %) required percutaneous drainage, 3 (2.8 %) were reoperated upon. Pancreatic fistula accounted for half of complications.
There were 13 (12.4 %) readmissions: 9 for intra-abdominal collections, 1 for visceral artery bleeding, 1 for splenic infarction, 1 for GI bleeding, and 1 for pancreatitis.
A total of 11 (10.4 %) laparoscopies with conversion were carried out; 10 laparoscopic DPs were performed -3 with splenic preservation and 1 with vessel preservation. Two complications occurred- 1 PF and 1 wound infection.
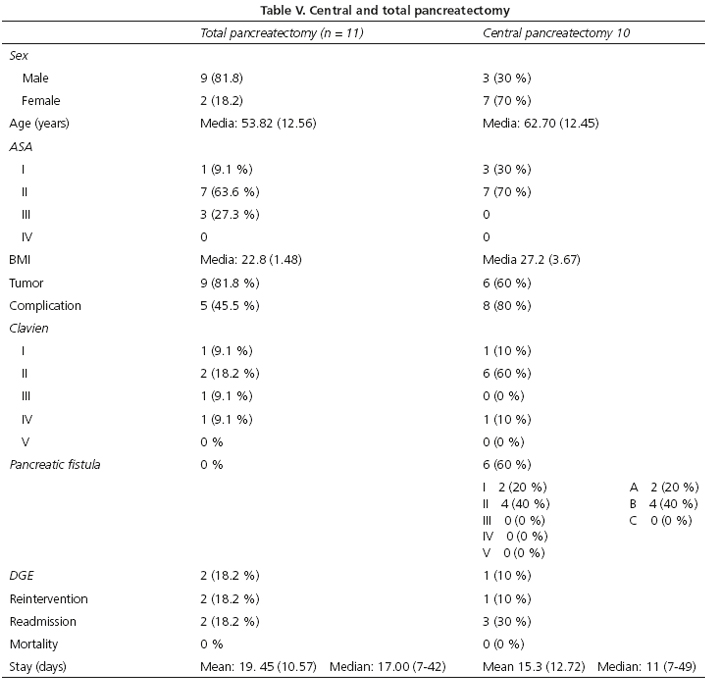
Total pancreatectomy
Eleven TPs were performed -8 for adenocarcinoma, 2 for chronic pancreatitis, and 1 for a neuroendocrine tumor. Morbidity was lower as compared with CDP, and no deaths occurred (Table V).
Central pancreatectomy
Ten CPs were performed -3 type-II mucinous intraductal papillary tumors, 4 cystic tumors, and 3 neuroendocrine tumors. The distal pancreas was anastomosed to the jejunum on 5 occasions, and PG was used for the remaining cases. Complications amounted to 80 % -70 % were mild (Clavien I-II), all of them pancreatic fistulas of intra-abdominal infections solved with antibiotic therapy. One visceral artery bleeding event required reintervention to complete a distal pancreatectomy. No deaths occurred. Readmission for fever and intra-abdominal collections was required for 30 % of patients (Table V).
Discussion
This review of 480 pancreatectomies is to our knowledge the most extensive series reported in the literature by Spanish groups, both in total numbers and CDPs.
Overall mortality in our series was 12 patients (2.5 %), with 11 (3.3 %) in 332 CDPs, which is comparable to other Spanish (12,13,18,19) as well as foreign (2,20,21) series.
Hospital de Bellvitge (19) published a series of 204 CDPs for pancreatic adenocarcinoma. They used the IGSPF classification for PF, but not Clavien's classification for the other complications, which renders comparisons with our series difficult. PF rate was 10 % with PJ, better than in our series, but the fact that ductal pancreatic adenocarcinoma is usually associated with a hard pancreas and dilated Wirsung duct is to be considered, which entails a lower risk for PF. Reintervention and mortality rates were 13 % and 7 % versus 9.2 % and 1.5 % in our series.
As regards CDP, the series by Figueras et al. (11)compared the results of 58 PJs and 65 PGs in a prospective, randomized study using the same technique for both types of pancreatic reconstruction as in our series. They conclude that PG significantly reduces PF incidence and severity. Severe complications for both techniques were 38.9 % versus 25.6 % in our series. If we consider only PGs, it was 63 % versus 50.9 % of our cases. The overall incidence of PF was 24.4 % [34 % for PJ and 15 % for PG (p = 0.014)]. In our series it was 22.9 % [29.9 % for PJ and 14.8 % for PG (p < 0.000)]. Regarding PF severity, their results were: 33 % grade B-C for PJ and 11 % for PG (p = 0.006). In our series we found 22 % for PJ and 12.3 % for PG (p = 0.000). Both series agree that PF incidence and severity are lower for PG.
In the aforementioned paper DGE was 27.6 %, similar between PJ and PG, in contrast to our series, with an overall value of 34.3 % but with 45.7% for PJ and 21.3 % for PG (p < 0.000). Such difference may be accounted for by the association between abdominal complications and DGE, previously demonstrated by other authors (22).
The second study that may compare to our series is a Belgian prospective, randomized, multicenter clinical trial on 329 CDPs (23), half PJs and half PGs, with stratification by Wirsung duct diameter (≥ 3 mm). Mean complications were 62 %, similar to our series, with no differences between the two reconstruction techniques. Nor were any differences in reintervention and mortality rates. Mean hospital stay was 18.5 days, with no differences between groups; in our experience, this was 26.7 days (19.93) for PJ and 13.2 days (9.22) for PG (p < 0.000).
The conclusion reached by the Belgian study is that PG is more efficient than PJ for pancreatic fistula prevention and complication severity, but not for overall incidence. Differences in PJ outcome with our series may result from the different technique used duct-to-mucosa in our series, invaginated in the Belgian study. A randomized study showed that invaginated PJ was superior to duct-to-mucosa PJ (24), which may explain such differences with the results seen in the series by Figueras et al. (11) and in our series.
PF holds a relationship with pancreatic texture and Wirsung duct diameter, and represents the primary cause of postoperative morbidity and mortality. In the Belgian series (26) PF increases death risk four-fold, and in the study by Figueras et al. (11) there is a HR of 7.29 for severe complications. In our experience PF is significantly associated with severe complications but not with mortality.
In the prospective, randomized study by Fernández Cruz et al. (25) outcomes are better than above, but their comparison may be biased due to differences in PG technique. A meta-analysis in 2014 (26) summarizes the 7 prospective, randomized studies comparing PJ versus PG, 4 of them using the ISGPF classification. Conclusions are consistent with our findings: PG results in fewer PFs when compared to PJ (p < 0.001).
Regarding quality standards, Sabater et al. (5) performed an elegant review of 6,336 CDPs for periampullary neoplasms during 2000-2010 using the ISGPS classification, and concluded that the acceptable quality limits are: < 55 % for morbidity (no specific classification is quoted), < 31 % for PF (as per the ISGPF classification; the authors also point out that 12 definitions of PF are presently used), and < 5 % for mortality.
The four series mentioned above (11,19,23,25), as well as ours, meet the required quality criteria, but it should be noted that overall morbidity was not obtained using Clavien's classification. Spanish groups have reported their own standards -the first one was published in 2002 by Figueras et al. (27), who suggest that limits should be 10 % for mortality and 50 % for morbidity regarding CDP. In 2011, Fernández Cruz et al. (28) reviewed CDP complications. In 2013, Domínguez-Comesaña (12) reported on 117 pancreatectomies (61 CDPs -58 PJs-, 15 TPs and 40 DPs) with a morbidity of 59 % for CDP (PF 9.83 %, DGE 9.8 %, bleeding 16.4 %, reintervention 23 %, mortality 6.5 %). Two additional Spanish teams have reported series with similar results -Sabater et al. in 2009 (18) and Montiel et al. in 2010 (29).
As for DP our series meets the quality criteria published by Sabater et al. (5), who reviewed 11 series with over 100 patients and acceptable quality limits at < 53 % for morbidity, < 31 % for PF, and < 1 % for mortality.
A comparable series was reported by Goh (21), who discusses 232 open DPs during 21 years with a morbidity of 47 %, a mortality of 3 %, and a PF rate of 31 % (18 % A, 6 % B, 8 % C), similar to our results.
CP is a procedure with the primary goal of pancreas preservation in benign or borderline lesions. It associates the morbidity of DP with that of pancreaticoenteric anastomosis; this explains our high morbidity rate of 80 % (Clavien ≥ III, 10 %), albeit with no deaths. In a French multicenter study (30) of 100 CPs with reconstruction by PG morbidity was 72 % (Clavien ≥ III, 18 %), with 6 % reinterventions and 3 % mortality.
The limitations of our study have to do with a historical series where some mild complications may have been not counted in, since recorded complications had to be translated using international classifications. Furthermore, when comparing PJ versus PG sample volume was not estimated, although we deem the series adequate for our purposes.
Conclusions
The described CDP and PG series represents the most numerous reports by Spanish sites ever. Our findings meet the required morbidity- and mortality-related quality criteria as compared to current series and reported standards. We coincide with reported meta-analyses in that pancreatic reconstruction by PG offers better outcomes as compared with PJ (duct-to-mucosa) in terms of PF (frequency and severity), abdominal complications, severe morbidity, and hospital stay, even though mortality is not improved. For DP our findings are consistent with the reported standards, although a laparoscopic approach will likely improve them. Regarding CP, we agree with other teams that, being a conservative procedure to preserve pancreatic function, its mortality is high and the technique should reserve for younger patients with a low surgical risk.
References
1. Eppsteiner RW, Csikesz NG, McPhee JT, Tseng JF, Shah SA. Surgeon volume impacts hospital mortality for pancreatic resection. Ann Surg. 2009;249:635-40. [ Links ]
2. Orr RK. Outcomes in pancreatic cancer surgery. Surg Clin North Am. 2010;90:219-34. [ Links ]
3. Hartwig W, Werner J, Jäger D, Debus J, Büchler MW. Improvement of surgical results for pancreatic cancer. Lancet Oncol. 2013;14:e476-85. [ Links ]
4. Yoshioka R, Yasunaga H, Hasegawa K, Horiguchi H, Fushimi K, Aoki T, et al. Impact of hospital volume on hospital mortality, length of stay and total costs after pancreaticoduodenectomy. Br J Surg. 2014;101:523-9. [ Links ]
5. Sabater L, García-Granero A, Escrig-Sos J, Gómez-Mateo MDC, Sastre J, Ferrández A, et al. Outcome quality standards in pancreatic oncologic surgery. Ann Surg Oncol. 2014;21:1138-46. [ Links ]
6. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8-13. [ Links ]
7. Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761-8. [ Links ]
8. Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142:20-5. [ Links ]
9. Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-13. [ Links ]
10. Strasberg SM, Linehan DC, Clavien P-A, Barkun JS. Proposal for definition and severity grading of pancreatic anastomosis failure and pancreatic occlusion failure. Surgery. 2007;141:420-6. [ Links ]
11. Figueras J, Sabater L, Planellas P, Muñoz-Forner E, Lopez-Ben S, Falgueras L, et al. Randomized clinical trial of pancreaticogastrostomy versus pancreaticojejunostomy on the rate and severity of pancreatic fistula after pancreaticoduodenectomy. Br J Surg. 2013;100:1597-605. [ Links ]
12. Dominguez-Comesaña E, Gonzalez-Rodriguez FJ, Ulla-Rocha JL, Lede-Fernandez A, Portela-Serra JL, Piñon-Cimadevila MÁ. Morbimortalidad de la reseccion pancreatica.. Cir Esp. 2013;91:651-8. [ Links ]
13. Fernández-Cruz L, Sabater L, Fabregat J, Boggi U. Complicaciones despues de una pancreaticoduodenectomia. Cir Esp. 2012;90:222-32. [ Links ]
14. Fabregat J, Busquets J, Peláez N, Jorba R, García-Borobia F, Masuet C, et al. Tratamiento quirúrgico del adenocarcinoma pancreático mediante duodenopancreatectomía cefálica (parte 2). Seguimiento a largo plazo tras 204 casos. Cir Esp. 2010;88:374-82. [ Links ]
15. Kimura W. Pancreaticojejunal anastomosis, using a stent tube, in pancreaticoduodenectomy. J Hepatobiliary Pancreat Surg. 2009;16:305-9. [ Links ]
16. Delcore R, Thomas JH, Pierce GE, Hermreck AS. Pancreatogastrostomy: a safe drainage procedure after pancreatoduodenectomy. Surgery. 1990;108:641-5; discussion 645-7. [ Links ]
17. Lassen K, Coolsen MME, Slim K, Carli F, de Aguilar-Nascimento JE, Schäfer M, et al. Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS®) Society recommendations. World J Surg. 2013;37:240-58. [ Links ]
18. Sabater L, Calvete J, Aparisi L, Cánovas R, Muñoz E, Añón R, et al. Neoplasias de pancreas y periampulares: morbimortalidad, resultados funcionales y supervivencia a largo plazo. Cir Esp. 2009; 86:159-66. [ Links ]
19. Busquets J, Fabregat J, Jorba R, Peláez N, García-Borobia F, Masuet C, et al. Tratamiento quirurgico del adenocarcinoma pancreatico mediante duodenopancreatectomia cefalica (Parte 1). Complicaciones postoperatorias en 204 casos en un centro de referencia. Cir Esp. 2010;88:299-307. [ Links ]
20. Van Buren G 2nd, Bloomston M, Hughes SJ, Winter J, Behrman SW, Zyromski NJ, et al. A randomized prospective multicenter trial of pancreaticoduodenectomy with and without routine intraperitoneal drainage. Ann Surg. 2014;259:605-12. [ Links ]
21. Goh BKP, Tan Y-M, Chung Y-FA, Cheow P-C, Ong H-S, Chan W-H, et al. Critical appraisal of 232 consecutive distal pancreatectomies with emphasis on risk factors, outcome, and management of the postoperative pancreatic fistula: a 21-year experience at a single institution. Arch Surg Chic Ill 1960. 2008;143:956-65. [ Links ]
22. Park JS, Hwang HK, Kim JK, Cho SI, Yoon D-S, Lee WJ, et al. Clinical validation and risk factors for delayed gastric emptying based on the International Study Group of Pancreatic Surgery (ISGPS) Classification. Surgery. 2009;146:882-7. [ Links ]
23. Topal B, Fieuws S, Aerts R, Weerts J, Feryn T, Roeyen G, et al. Pancreaticojejunostomy versus pancreaticogastrostomy reconstruction after pancreaticoduodenectomy for pancreatic or periampullary tumours: a multicentre randomised trial. Lancet Oncol. 2013;14:655-62. [ Links ]
24. Berger AC, Howard TJ, Kennedy EP, Sauter PK, Bower-Cherry M, Dutkevitch S, et al. Does type of pancreaticojejunostomy after pancreaticoduodenectomy decrease rate of pancreatic fistula? A randomized, prospective, dual-institution trial. J Am Coll Surg. 2009;208:738-47. [ Links ]
25. Fernández-Cruz L, Cosa R, Blanco L, López-Boado MA, Astudillo E. Pancreatogastrostomy with gastric partition after pylorus-preserving pancreatoduodenectomy versus conventional pancreatojejunostomy: a prospective randomized study. Ann Surg. 2008;248:930-8. [ Links ]
26. Chen Z, Song X, Yang D, Li Y, Xu K, He Y. Pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy: A meta-analysis of randomized control trials. Eur J Surg Oncol 2014;40:1177-85. [ Links ]
27. Figueras Joan J, Valls C, Fabregat J, Serrano T, Jaurrieta E. Equipamiento, experiencia mínima y estándares en la cirugía hepatobiliopancreática (HBP). Cir Esp. 2002;71:201-6. [ Links ]
28. Fernández-Cruz L. Pancreaticojejunostomy versus pancreaticogastrostomy. J Hepato-Biliary-Pancreat Sci. 2011; 18: 762-8. [ Links ]
29. Montiel Casado MC, Pardo Sánchez F, Rotellar Sastre F, Martí Cruchaga P, Alvarez Cienfuegos FJ. Experiencia de un programa de fast-track en la duodenopancreatectomia cefalica. Cir Esp. 2010;87:378-84. [ Links ]
30. Goudard Y, Gaujoux S, Dokmak S, Cros J, Couvelard A, Palazzo M, et al. Reappraisal of central pancreatectomy a 12-year single-center experience. JAMA Surg. 2014;149:356-63. [ Links ]
![]() Correspondence:
Correspondence:
Francisco Javier Herrera-Cabezón
Department of General Surgery (Pabellón H-3o)
Complejo Hospitalario de Navarra-A
Irunlarrea, s/n
31008 Pamplona, Navarra. Spain
e-mail: javierherrera2004@gmail.com
Received: 07-10-2014
Accepted: 23-12-2014











 texto en
texto en