Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.107 no.4 Madrid abr. 2015
LETTERS TO THE EDITOR
Intrahepatic pancreatic pseudocyst: A case report
Pseudoquiste pancreático de localización intrahepática
Key words: Pseudocyst. Pancreatic.
Palabras clave: Pseudoquiste. Intrahepático.
Dear Editor,
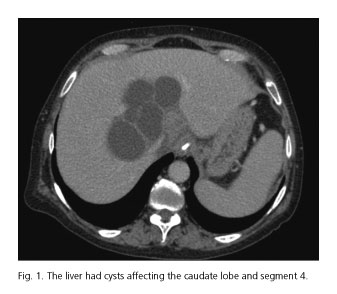
We report a 46-years-old woman diagnosed in 2010 as having pseudocysts after alcoholic chronic pancreatitis (CP) and followed with endoscopic ultrasound (EUS). At this consultation, she complained of epigastric pain radiating into belt, intensified in the last two weeks. Laboratory tests showed amylase of 794 UI/L and amylasuria of 16.900 UI/L; and CT reported uncomplicated hepatic (Fig. 1) and pancreatic (Fig. 2) cysts. With a diagnosis of acute exacerbation of chronic pancreatitis, conservative treatment with inhibitors of proton pump, meperidine and metamizol and nasojejunal feeding tube was introduced. Pancreatic secretion inhibitory drugs were not administered. A 10 cm pseudocyst was drained to relieve pain, checking the simultaneous decrease of liver lesions. The analysis of the amylase showed 114.000 UI/L.
The sonographic control after 6 weeks revealed a decrease of intrahepatic cystic images, but the larger pancreatic pseudocyst persisted, causing pain due to gastric compression. After therapeutic EUS-guided transgastric drainage, the patient progressed satisfactorily. Twelve months later, she remained asymptomatic, with almost complete resolution of the lesions.
Discussion
A significant number of patients with chronic pancreatitis remain asymptomatic until the appearance of complications (1,2), which will determine the clinical course of the disease: Pseudocysts (25-30%), common bile duct stenosis (40-50%) and even pancreatic cancer (3%) (3). Pancreatic pseudocysts are described in multiple extra-pancreatic locations (20%) (1). The intrahepatic location is exceptional, usually asymptomatic and more common in the left lobe (1). As pathophysiological mechanism, the effect of pancreatic proteolytic enzymes, which allows the formation of pseudocysts in so many different areas as the liver, pleura, mediastinum, and retroperitoneum (1,4), is proposed. Some authors suggest the hepatoduodenal ligament as a way of dissemination (5). It is suspected by imaging techniques, in the presence of liver cystic lesion in the course of acute pancreatitis or exacerbations; diagnostic confirmation is established by elevated amylase in the intracystic liquid (6). The treatment of pancreatic pseudocysts located in the liver is conservative because most resolve spontaneously, reserving percutaneous drainage or surgery for symptomatic or complicated cases (1,5), although there is no consensus. In our case, probably the largest pseudocyst was in continuity with liver lesions; hence, EUS+ cystogastrostomy was therapeutic.
Nuria Martínez-Sanz1, F. Miguel González-Valverde2,
María Vicente-Ruiz1, Patricia Pastor-Pérez1,
Miguel Ruiz-Marín1 and Antonio Albarracín-Marín-Blázquez1
1Department of General Surgery and Digestive Diseases.
Hospital General Universitario Reina Sofía. Murcia, Spain.
2Department of Surgery. Universidad de Murcia. Murcia, Spain
References
1. Les I, Córdoba J, Vargas V, et al. Pseudoquiste pancreático de localización hepática. Rev Esp Enferm Dig 2006;98:616-20. [ Links ]
2. Vaquero Raya EC, Molero Richard X. Pancreatitis crónica. En: Ponce J, Castells Garangou A, Gomollón García F, editores. Tratamiento sobre las enfermedades gastroenterológicas. 3a ed. Madrid: Asociación Española de Gastroenterología; 2011. p. 439-53. [ Links ]
3. Jimeno Ayllón C, Pérez García J, Gómez Ruiz CJ, et al. Criterios estándar versus clasificación de Rosemont para el diagnóstico ecoendoscópico de pancreatitis crónica. Rev Esp Enferm Dig 2011;103:626-31. [ Links ]
4. Baranyai Z, Jakab F. Pancreatic pseudocyst propagating into retroperitoneum and mediastinum. Acta Chir Hung 1997;36(1-4):16-7. [ Links ]
5. Goyal S, Raju R, Yadav S. Pancreatic pseudocyst of gastrohepatic ligament: A case report and review of management. JOP 2012;13(4):439-42. [ Links ]
6. Iglesias García J, Domínguez Muñoz JE. Curso de actualización de la SEED. Papel de la endoscopia en el diagnóstico y el tratamiento del pseudoquiste pancreático. Diagnóstico diferencial de las lesiones quísticas del páncreas. Rev Esp Enferm Dig 2009;101(Supl. I):219-32. [ Links ]











 texto en
texto en