Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.107 no.7 Madrid jul. 2015
PICTURES IN DIGESTIVE PATHOLOGY
Usefulness of magnifying endoscopy with narrow-band imaging for identification of early gastric cancer around an ulcer scar
Tae Matsunaga, Hideki Kobara, Hirohito Mori, Shintaro Fujihara and Tsutomu Masaki
Department of Gastroenterology and Neurology. Kagawa University. Faculty of Medicine. Kagawa University. Kagawa, Japan
A 60-year-old man with familial colonic polyposis presented for screening upper GI endoscopy; he had previously undergone pancreato-duodenectomy because of Vater's papilla cancer and total colectomy. Conventional white light endoscopy (C-WLE) revealed an ulcer scar with converting folds located in the upper remnant stomach; a gastric tumor was not detected (Fig. 1). Subsequently, magnifying endoscopy with narrow-band imaging (NBI-ME) was performed for detailed assessment of the ulcer scar, including the surrounding mucosa, and demonstrated a carcinoma with a demarcation line (DL) (Fig. 2) and an irregular micro-vascular pattern (Fig. 3) based on the VS (vessel plus surface) classification system (1) on the anal side of the ulcer scar. C-WLE shows a concordant line demarcated by NBI-ME (Fig. 4). The determination of DL by C-WLE appeared to be difficult. Informed consent for endoscopic submucosal dissection (ESD) treatment was received from the patient.
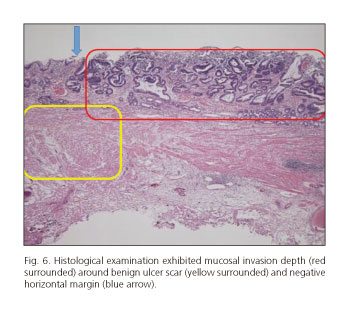
After the lesion was circumferentially marked using NBI-ME, standard ESD was completed without complications. Histology revealed curative resection of a well-differentiated adenocarcinoma in adenoma corresponding to the demarcation line drawn preoperatively using NBI-ME (Fig. 5); the lesion exhibited mucosal invasion depth around benign ulcer scar (Fig. 6).
Discussion
Recently, the development of NBI-ME has enabled us to differentiate between benign and malignant tumors and to determine the horizontal extent of gastric cancers (1,2). Moreover, some authors have described NBI-ME is more accurate than C-WLE in the diagnosis of gastric mucosal cancer (3). With C-WLE, the identification of early gastric cancer around an ulcer scar can be difficult because of morphological mucosal changes, severe gastritis in the background, and the lack of a color change (4).
Although the utility of NBI-ME in the detection of early gastric cancer around an ulcer scar remains unclear, this case suggests that NBI-ME may be more useful than C-WLE in this clinical scenario.
Acknowledgments
The authors wish to thank the Diagnostic Pathology Departments of the Kagawa University Hospital for their contribution to this study.
References
1. Yao K, Nagahama T, Matsui T, et al. Detection and characterization of early gastric cancer for curative endoscopic submucosal dissection. Dig Endosc 2013;25:44-54. [ Links ]
2. Kato M, Kaise M, Yonezawa J, et al. Magnifying endoscopy with narrow-band imaging achieves superior accuracy in the differential diagnosis of superficial gastric lesions identified with white-light endoscopy: A prospective study. Gastrointest Endosc 2010;72:523-9. [ Links ]
3. Ezoe Y, Muto M, Uedo N, et al. Magnifying narrowband imaging is more accurate than conventional white-light imaging in diagnosis of gastric mucosal cancer. Gastroenterology 2011;141:2017-25. [ Links ]
4. Graham DY, Schwartz JT, Cain GD, Gyorkey F. Prospective evaluation of biopsy number in the diagnosis of esophageal and gastric carcinoma. Gastroenterology 1982;82:228-31. [ Links ]