Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.107 no.8 Madrid ago. 2015
Hilar bile duct tumors: Endoscopic or percutaneous drainage? A prospective analysis
Tumores hiliares biliares: ¿drenaje endoscópico o percutáneo? Análisis prospectivo
Martín Alejandro Guidi, Cecilia Curvale, Juan Viscardi, Hui Jer Hwang, Julio César de-María, Esteban Promenzio, Fernando Ragone and Raúl Fernando Matanó
Department of GI Endoscopy. Hospital de Alta Complejidad en Red El Cruce "Dr. Néstor Carlos Kirchner", Florencio Varela. Buenos Aires, República Argentina
ABSTRACT
Background and objective: Both the endoscopic and the percutaneous approach are widely accepted for the drainage of hilar tumors. Our primary objective was to report on the effectiveness and complications of these procedures.
Methods: Prospective observational analysis of the endoscopic and/or percutaneous management of all hilar tumors treated at a referral hospital from October 2011 until October 2014. Group A included patients treated endoscopically and group B included patients treated with percutaneous drainage. The following variables were assessed: Effective biliary drainage rate, survival time and complications.
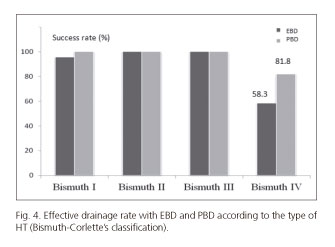
Results: Group A comprised 40 patients and group B, 22 patients. Overall success rate in achieving effective biliary drainage was 85% in group A and 90.9% in group B (p = 0.78). Five patients required a combined approach. In group A, the rate of effective drainage in patients with Bismuth IV-type tumors was 58.3%, while it was 81.8% in patients in group B (p = 0.44). There was no difference in mean survival between both groups. For group A, complication rate was 11.5%, whereas it was 2.94% for group B (p = 0.41).
Conclusions: Endoscopic and percutaneous biliary drainage are both effective methods for the palliative treatment of patients with hilar tumors. However, for Bismuth IV-type strictures, percutaneous drainage proved to be safer and more effective.
Key words: Hilar bile duct tumors. Endoscopic biliary drainage. Percutaneous biliary drainage. Post-ERCP complications. Cholangitis.
RESUMEN
Antecedentes y objetivo: existen dos técnicas válidas para el drenaje de los tumores hiliares: el abordaje endoscópico y el percutáneo. Nuestro objetivo primario fue reportar la efectividad y las complicaciones de estos procedimientos.
Métodos: análisis prospectivo observacional referido al manejo endoscópico y/o percutáneo de todos los tumores hiliares intervenidos en un hospital de tercer nivel desde octubre de 2011 a octubre de 2014. El grupo A representó a los pacientes abordados endoscópicamente, y el grupo B incluyó aquellos con drenaje percutáneo. Se analizaron las siguientes variables: tasa de drenaje biliar efectivo, tiempo de sobrevida y complicaciones.
Resultados: el grupo A tuvo 40 pacientes y el grupo B 22. La tasa de éxito global en lograr un drenaje biliar efectivo fue del 85% en el grupo A y del 90,9% en el grupo B (p = 0,78). En cinco pacientes se requirió un abordaje combinado. La efectividad del grupo A en el drenaje de pacientes con tumores tipo Bismuth IV fue del 58,3%, mientras que el grupo B alcanzó el 81,8% (p = 0,44). La sobrevida media de los pacientes no presentó diferencias estadísticas entre ambos grupos. En el grupo A la tasa de complicaciones alcanzó un 11,5% mientras que en el B fue de 2,94% (p = 0,41).
Conclusiones: el drenaje biliar endoscópico y el percutáneo son métodos efectivos en el tratamiento paliativo de los tumores hiliares. Sin embargo, en estenosis tipo Bismuth IV, el drenaje percutáneo resultó más efectivo y seguro.
Palabras clave: Tumores biliares hiliares. Drenaje biliar endoscópico. Drenaje biliar percutáneo. Complicaciones post-CPRE. Colangitis.
Introduction
Malignant strictures of the hepatic hilum are caused by a heterogeneous group of tumors that includes proximal primary carcinomas (Klatskin tumors), neoplasias extending to the biliary hilar bifurcation (gallbladder cancer) and metastatic tumors or malignant lymph nodes. These lesions are known as hilar tumors (HT) (1). They entail a poor prognosis since many patients die during the first year following diagnosis. Although surgery is the standard of care for curative treatment, in most cases the objective will be palliative treatment, since resectability is estimated to be less than 20% at the time of diagnosis (2). Biliary decompression is useful not only to palliate pruritus or jaundice but also to alleviate other associated symptoms, such as anorexia and vomiting, thus allowing for a better quality of life for these patients (3).
To assess the extent of biliary involvement, CT and MR-cholangiography are needed. In 1975 Bismuth and Corlette established a classification for the management of these patients; according to the subtype of HT one could determine whether patients would benefit from an endoscopic biliary drainage (EBD) or from a percutaneous biliary drainage (PBD) (4).
Both EBD and PBD are minimally invasive techniques validated for the palliative treatment of HT (5), but we do not know for certain which is the procedure of choice. Although success rate is better with PBD, EBD offers better patient comfort and requires a shorter hospital stay (6). However, several studies have shown that EBD may be technically difficult in HT classified as Bismuth III-IV types and entails a higher risk of post-procedure cholangitis due to incomplete drainage of the opacified intrahepatic biliary tree (7,8). In his 1988 study, Deviere cautioned about this problem (9). Costamagna et al. proposed the initial endoscopic approach in Bismuth I type of HT, while in subtypes II, III and IV PBD would be safer and more effective (10).
Current evidence suggests that minimally invasive management of HT should be performed at referral hospitals by a multidisciplinary team, experienced in endoscopic as well as percutaneous and surgical approaches (11).
The objective of this paper is to report on the effectiveness and safety of both EBD and PBD in the minimally invasive palliative treatment of HT.
Methods
We prospectively analyzed a cohort of patients with unresectable hilar tumors who consulted the Endoscopy Department of a large referral hospital from October 2011 to October 2014. According to the therapeutic procedure implemented, patients were assigned to one of two groups, group A: EBD and group B: PBD.
All patients with a diagnosis of unresectable HT were consecutively included. Unresectability criteria were determined by the extent of the disease according to imaging studies and/or the patient's general condition.
The Bismuth-Corlette classification was used to assess the type of hilar involvement (Fig. 1).
All patients were older than 18 years and all signed an informed consent form.
Variables assessed were: Effective biliary drainage, survival time, and complications.
Definition of events
Effective biliary drainage was defined as a 50% decrease in the level of initial total bilirubin after 2 weeks of treatment (6).
Early and late complications were defined as undesired events occurring before and after 30 days of treatment, according to Cotton's criteria (12). Definitions were as follows:
- Cholangitis: Fever (axillary temperature ≥ 38oC) with no other obvious source of infection, persisting more than 24 hours post-procedure, and accompanied by abnormal or worsened liver function tests (6).
- Pancreatitis: Abdominal pain associated to a rise in serum amylase more than threefold the upper limit of normal, within 24 hours of the procedure (12).
- Hemorrhage: Clinically evident bleeding resulting in a drop of at least 2 g/dl in hemoglobin or requiring blood transfusion (13).
Survival was estimated in months, since the moment of diagnosis of the HT until the patient's death.
General technical aspects regarding ERCP (endoscopic retrograde cholangiopancreatography) and PBD
Pre-procedure exams included the usual evaluation for anesthesia with an ECG and hemostasis testing. Wide spectrum prophylactic antibiotics were administered intravenously.
Group A
All ERCP's were performed with the patient in the prone position and a therapeutic duodenoscopy equipment was employed (4.2 mm channel). The contrast medium used for cholangiography was 68% Ioversol, 320 mg/ml, as a 50% dilution. Sphincterotomies were performed using pure cut current. Two experienced endoscopists (performing more than 300 exams per year) were in charge of the procedures. After obtaining access to the biliary tree via cannulation with a sphincterotome and a hydrophilic guidewire, cholangiography was performed and characteristics of hilar strictures were assessed according to Bismuth's classification. After papillotomy, biliary drainage was performed by placing plastic or metal biliary stents (7, 8.5 and 10F) (Fig. 2). Whenever necessary, progressive dilatations were performed using Soehendra dilators and/or 8-10 mm biliary dilating balloons, followed by placement of a stent with the largest possible caliber. Stents' length was determined according to the level of the stricture assessed by cholangiography. The type of stent (metal or plastic) was decided based on the patient's performance status and device availability. Patients with a good performance status (as previously defined by the Departments of Oncology and Palliative Care) were candidates for metal stents. Prior to ERCP, tomographic images of all patients were analyzed and atrophy or hypertrophy (when present) of hepatic lobes was assessed. If one lobe was atrophic, its cannulation and contrast injection were avoided to minimize the risk of cholangitis. The primary goal of the procedure consisted in draining the hypertrophic (functioning) lobe. If there was no atrophy or hypertrophy, and whenever it was technically possible, both hepatic ducts were cannulated and drained (in Bismuth II-III-IV-types of HT).
Group B
All PBD's were performed with patients in the dorsal decubitus, with local anesthesia and neuroleptanalgesia. Biliary access was confirmed using a C-arm digital equipment and/or a portable echo machine. As contrast medium for the cholangiogram, we used 68% Ioversol, 320 mg/ml, as a 50% dilution. After accessing the intrahepatic biliary tree with a Chiva needle and a hydrophilic guidewire, a cholangiogram was performed to assess the stricture's characteristics. Subsequently, biliary drainage was performed using internal-external or external catheters, or self-expandable biliary stents as appropriate (Fig. 3).
- Patients were followed since the intervention and until their death, via regular visits or telephone calls to the patient, his/her relatives and/or the family physician.
- The study was approved by our Hospital's Research and Ethics Committee. All patients included gave their written informed consent. The protocol complies with the ethical guidelines of the 1975 Declaration of Helsinki (1983 revision).
Statistical analysis
Data were analyzed using MedCalc® software, version 11.2.1.0 (MedCalc Software; Broekstraat, Mariakerke, Belgium). Descriptive statistical data were expressed as mean, median, standard deviation and range, as appropriate, and according to data distribution as proportions and rates. The χ2 test was used for between-group comparisons, and the Kaplan-Meier test was used to analyze patient survival. A p value < 0.05 was considered statistically significant.
Results
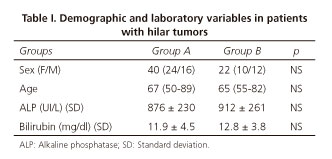
Group A included 40 patients and group B included 22 patients. No difference between both groups was found in demographic variables or laboratory values (Table I).
A total of 52 procedures were performed in group A (1.3 procedures/patient) and 30 procedures were performed in group B (1.36 procedures/patient).
Table II summarizes the number of patients in each group according to Bismuth's classification.
Effective biliary drainage rate was 85% in group A, while it was 90.9% in group B. Five patients in group A required a combined approach with EBD and PBD (one Bismuth I and 4 Bismuth IV tumors), and one patient could not be drained with any of the two methods. The procedure failed in 2 cases of group B (one patient crossed over from group A) and these patients, with no procedure-related complications, died during the course of their disease.
In figure 4 we summarize the effective biliary drainage rate by Bismuth type subgroup in each arm.
In group A, 13 patients (32.5%) received bare metal stents measuring 8, 10 and 12 cm in length x 10 mm in diameter. In one patient with a Bismuth IV tumor, 2 metal stents were placed in parallel, and adequate drainage from both hepatic lobes was achieved.
In 22 patients (55%) plastic stents were placed; of them 17 were 10F, 4 were 8.5F and one was a 7F stent. All patients with Bismuth II, III and IV strictures (except for one) received double plastic stents, thus achieving bilateral drainage (Table III).
Among the 22 patients in group B, 11 received and internal-external biliary drainage (50%), 8 an external biliary drainage (36.34%), and in one case of a Bismuth IV tumor, self-expandable biliary stents were used (4.5%).
In group A, complication rate was 11.5%. Four cholangitis (3 in patients with Bismuth IV type strictures) and 1 liver abscess were reported, which required percutaneous drainage. There was one bleeding episode that required endoscopic treatment. In group B. complication rate was 2.94% (one cholangitis in a patient with a Bismuth IV type stenosis with favorable response to antibiotic treatment). There were no deaths associated with the percutaneous procedure.
In group A mortality was 1.92%. There was one case of septicemia associated to a post-procedure cholangitis. That patient had a Bismuth IV hilar stricture, where only a size 7F plastic stent could be placed in the left hepatic lobe. The patient's poor general condition (due to his underlying disease) together with the rapid progression of the infection, did not allow to attempt a percutaneous drainage.
Mean survival for group A was 7.9 months, compared to 4.8 months for group B.
Combined approach (EBD + PBD)
Five patients required a simultaneous endoscopic and percutaneous approach. Four cases were Bismuth IV strictures and one case was a Bismuth I stricture.
- Effective biliary drainage rate, adding the success achieved with each individual technique plus that obtained with the combined approach, was 95.16% (59/62 patients).
- All patients enrolled in the protocol were followed until their death.
- Overall study results are summarized in table IV and in figure 5.
Discussion
Ideally, a palliative drainage should be simple and effective in alleviating obstructive cholestasis, entail a low morbidity and mortality and maintain biliary permeability for as long as possible (14). Many authors consider EBD as the treatment of choice for neoplastic biliary obstruction (15,16).
However, Fockens et al. (17) explain that in types Bismuth III and IV hilar strictures, EBD may pose technical problems. In these patients, the risk of incomplete drainage after contrast injection in the intrahepatic biliary tree entails a high risk of post-ERCP cholangitis (18,19).
In our report, failed attempts of endoscopic drainage prevailed in the group of patients with Bismuth IV type of strictures, in most cases because the obstruction could not be crossed. In only one case, the biliary tree, after contrast injection, could not be sufficiently drained with a 7F stent. Based on published data and our own results, we believe that with these tumors the minimum stent caliber to ensure biliary drainage is 8.5F, not only to prevent post-ERCP cholangitis, but also because the life span of a plastic stent is determined by its size.
In cases of HT involving the bifurcation and hepatic branches (Bismuth types II-III-IV), the literature is controversial regarding whether the type of drainage should be unilateral (20-22) or bilateral (9,23,24). Several authors claim that a drainage greater than 50% of the functioning liver volume should be achieved, as assessed by axial section images (25). In our study, bilateral drainage was performed in all cases that were technically feasible. Unilateral drainage of the functioning lobe was performed in only 3 cases (all Bismuth IV type strictures). The 2 patients who received a metal stent did well, whereas the patient with a unilateral 7F plastic stent suffered the only lethal complication in the study. We believe it is essential to ensure drainage of the intrahepatic tree after contrast administration, and if the endoscopic method has not been effective enough, a combined approach should be used.
We routinely evaluate the hepatic segments with axial computed tomography (CT) prior to endoscopy. When one lobe is dominant over another due to atrophy of the occluded segments and bilateral cannulation cannot be achieved, drainage of the dominant hepatic lobe is assigned priority.
One prospective controlled study (26) and two retrospective studies (6,15) have compared EBD vs. PBD, including Bismuth II/III, III/IV and II-III-IV types of HT. The authors showed that in HT, PBD is safer and more effective.
In agreement with the literature, we achieved high global rates of effective biliary drainage in both groups (EBD: 85% vs. PBD: 90.9%). However, when we analyzed the subgroup of patients with Bismuth IV type of hilar strictures, the percutaneous technique proved safer and more effective. As to Bismuth II and III types of HT, there seems to be no difference regarding the choice of drainage approach; although the endoscopic approach offers patients a better quality of life. A larger group of patients should be analyzed in order to confirm these conclusions.
In our study, cholangitis was the most frequent complication. There were no cases of post-ERCP pancreatitis, possibly due to the characteristics of our population (elderly patients with high bilirubin levels) and to the use of pure cut current when performing sphincterotomy (27). As in previous publications, our series showed no significant difference in survival among both groups.
The main limitations were our small sample size and the non-randomized protocol, which entails a source of -generally- selection bias or imprecisions. It is worth noting that among the percutaneous group, which included less patients, more patients (Bismuth IV) had a technically difficult approach than among the endoscopic group. At our institution, with an independent Department of Percutaneous Surgery, many Bismuth IV cases are managed directly with PBD, without attempting an endoscopic approach. Hence, this hindered the overall comparison of results.
Finally, the insufficient statistical power for the analysis of results is related to the small sample size, as previously mentioned.
Conclusions
Hilar tumors are associated with a poor prognosis and limited survival of a few months. Both EBD and PBD are safe and effective methods for the palliative treatment of these tumors, mainly in the subgroups of Bismuth I, II and III strictures. The PBD is the treatment of choice for Bismuth IV type of HT. Referral centers for biliary disorders should have both drainage techniques available to manage patients with HT, since some patients will benefit from the combined approach. Randomized multicenter studies are needed to determine which is the palliative technique of choice.
Acknowledgements
We would like to thank the Research Area of the Hospital El Cruce "Dr. Néstor Carlos Kirchner", particularly to the doctors Maximiliano de Abreu and Laura Antonietti for their collaboration in the preparation of this manuscript.
References
1. Larghi A, Tringali A, Lecca PG, et al. Management of hilar biliary strictures. Am J Gastroenterology 2008;103:458-73. DOI: 10.1111/j.1572-0241.2007.01645.x. [ Links ]
2. Cheng JL, Bruno MJ, Bergman JJ, et al. Endoscopic palliation of patients with biliary obstruction caused by nonresectable hilar cholangiocarcinoma: Efficacy of self-expandable metallic Wallstents. Gastrointest Endosc 2005;56:33-9. DOI: 10.1067/mge.2002.125364. [ Links ]
3. Hookey LC, Le Moine O, Deviere J. Use of a temporary plastic stent to facilitate the placement of multiple self-expanding metal stents in malignant biliary hilar strictures. Gastrointest Endosc 2005;62:605-9. DOI: 10.1016/j.gie.2005.04.051. [ Links ]
4. Bismuth H, Corlette MB. Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver. Surg Gynecol Obstet 1975;140:170-8. [ Links ]
5. Born P, Rösch T, Brühl K, et al. Long-term outcome in patients with advanced hilar bile duct tumors undergoing palliative endoscopic or percutaneous drainage. Gastroenterol 2000;38:483-9. DOI: 10.1055/s-2000-14886. [ Links ]
6. Paik WH, Park YS, Hwang JH, et al. Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilar cholangiocarcinoma: A percutaneous versus endoscopic approach. Gastrointest Endosc 2009;69:55-62. DOI: 10.1016/j.gie.2008.04.005. [ Links ]
7. Chang WH, Kortan P, Haber GB. Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic duct drainage. Gastrointest Endosc 1998;47:354-62. DOI: 10.1016/S0016-5107(98)70218-4. [ Links ]
8. De Palma GD, Masone S, Rega M, et al. Endoscopic approach to malignant strictures at the hepatic hilum. World J Gastroenterology 2007;13:4042-5. DOI: 10.3748/wjg.v13.i30.4042. [ Links ]
9. Deviere J, Baize M, De Toeuf J, et al. Long-term follow-up of patients with hilar malignant stricture treated by endoscopic internal biliary drainage. Gastrointest Endosc 1988;34:95-101. DOI: 10.1016/S0016-5107(88)71271-7. [ Links ]
10. Dumonceau JM, Tringali A, Blero D, et al. Biliary stenting: Indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy 2012;44:277-98. DOI: 10.1055/s-0031-1291633. [ Links ]
11. Ho CH, Warkentin AE. Evidence-based decompression in malignant biliary obstruction. Korean J Radiol 2012;13:S56-61. [ Links ]
12. Cotton P, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: An attempt at consensus. Gastrointest Endosc 1991;37:383-93. DOI: 10.1016/S0016-5107(91)70740-2. [ Links ]
13. Freeman ML, Nelson DB, Sherman S, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med 1996;335:909-18. DOI: 10.1056/NEJM199609263351301. [ Links ]
14. Abraham NS, Barkun JS, Barkun AN. Palliation of malignant biliary obstruction: A prospective trial examining impact on quality of life. Gastrointest Endosc 2002;56:835-41. DOI: 10.1016/S0016-5107(02)70356-8. [ Links ]
15. Lee SH, Park JK, Yoon WJ, et al. Optimal biliary drainage for inoperable Klatskin tumors based on Bismuth type. World J Gastroenterology 2007;13:3948-55. [ Links ]
16. Kloek JJ, Van der Gaag NA, Aziz Y, et al. Endoscopic and percutaneous preoperative biliary drainage in patients with suspected hilar cholangiocarcinoma. J Gastrointest Surg 2010;14:119-25. DOI: 10.1007/s11605-009-1009-1. [ Links ]
17. Huibregtes I, Fockens P, Baron T. Plastic biliary stents for malignant biliary disease. Gastrointest Endosc Clin N Am 2011;21:435-43. DOI: 10.1016/j.giec.2011.04.010. [ Links ]
18. Andersen JR, Sorensen SM, Kruse A, et al. Randomized trial of endoscopic endoprostheses versus operative bypass in malignant obstructive jaundice. Gut 1989;30:1132-5. DOI: 10.1136/gut.30.8.1132. [ Links ]
19. Speer AG, Cotton PB, Russell RC, et al. Randomized trial of endoscopic versus percutaneous stent insertion in malignant obstructive jaundice. Lancet 1987;2:57-62. DOI: 10.1016/S0140-6736(87)92733-4. [ Links ]
20. De Palma GD, Galloro G, Siciliano S, et al. Unilateral versus bilateral endoscopic hepatic duct drainage in patients with malignant hilar biliary obstruction: Results of a prospective, randomized, and controlled study. Gastrointest Endosc 2001;53:547-53. DOI: 10.1067/mge.2001.113381. [ Links ]
21. De Palma GD, Pezzullo A, Rega M, et al. Unilateral placement of metallic stents for malignant hilar obstruction: A prospective study. Gastrointest Endosc 2003;58:50-3. DOI: 10.1067/mge.2003.310. [ Links ]
22. Polydorou AA, Cairns SR, Dowsett JF, et al. Palliation of proximal malignant biliary obstruction by endoscopic endoprosthesis insertion. Gut 1991;32:685-9. DOI: 10.1136/gut.32.6.685. [ Links ]
23. Chang WH, Kortan P, Haber GB. Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic duct drainage. Gastrointest Endosc 1998;47:354-62. DOI: 10.1016/S0016-5107(98)70218-4. [ Links ]
24. Witzigmann H, Berr F, Ringel U, et al. Surgical and palliative management and outcome in 184 patients with hilar cholangiocarcinoma: Palliative photodynamic therapy plus stenting is comparable to r1/r2 resection. Ann Surg 2006;244:230-9. DOI: 10.1097/01.sla.0000217639.10331.47. [ Links ]
25. Vienne A, Hobeika E, Gouya H, et al. Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: The role of liver volume assessment. Gastrointestinal Endoscopy 2010;72:728-35. DOI: 10.1016/j.gie.2010.06.040. [ Links ]
26. Saluja SS, Gulati M, Garq PK, et al. Endoscopic or percutaneous biliary drainage for gallbladder cancer: A randomized trial and quality of life assessment. Clin Gastroenterol Hepatol 2008;6:944-50 e943. DOI: 10.1016/j.cgh.2008.03.028. [ Links ]
27. Freeman ML, DiSario JA, Nelson DB, et al. Risk factors for post-ERCP pancreatitis: A prospective, multicenter study. Gastrointest Endosc 2001;54:425-34. DOI: 10.1067/mge.2001.117550. [ Links ]
![]() Correspondence:
Correspondence:
Martín Alejandro Guidi.
Department of GI Endoscopy.
Hospital de Alta Complejidad en Red El Cruce
"Dr. Néstor Carlos Kirchner", Florencio Varela.
Avenida Calchaqui 5401 (1888).
Buenos Aires, República Argentina
e-mail: maguidi71@yahoo.com.ar
Received: 26-01-2015
Accepted: 15-04-2015











 texto en
texto en