Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 no.2 Madrid feb. 2016
LETTERS TO THE EDITOR
Gastric neuroendocrine tumor presenting with gastrointestinal bleeding
Key words: Endoscopic submucosal dissection. Gastric neuroendocrine tumor. Gastrointestinal bleeding.
Dear Editor,
The most reported manifestations of gastric neuroendocrine tumor (GNETs) are non-specific symptoms such as epigastric pain, nausea, dyspepsia, etc. Gastrointestinal bleeding is an uncommon manifestation in GNETs patients and only few cases have been reported (1-4). This letter to editor describes a gastric polypoid lesion presenting with melena which was ultimately diagnosed with GNETs.
Case report
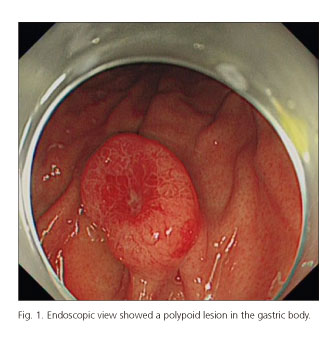
A 49-year-old woman came to our hospital with a week history of melena. There was no family history of gastrointestinal cancer. Upon presentation, her physical examination was not remarkable. Laboratory studies showed mild anemia (hemoglobin 9.7 g/dL, normal values: 11.5 ~ 15.0 g/dL) and an elevated blood gastrin level (84.96 × 10-3 ng/mL, normal values: 2.1 ~ 31.5 × 10-3 ng/mL). Esophagogastroduodenoscopy (EGD) revealed a 15 mm polypoid lesion in gastric body with erythematous depression and central ulcer (Fig. 1). Endoscopic ultrasonography (EUS) showed a thick mucosal layer without regional lymph node swelling (Fig. 2). Computerized tomography revealed no metastasis.
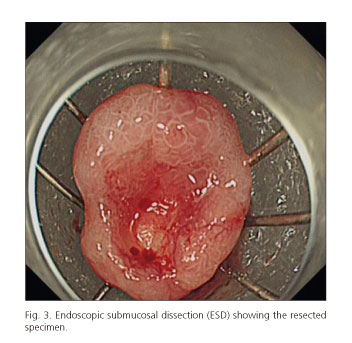
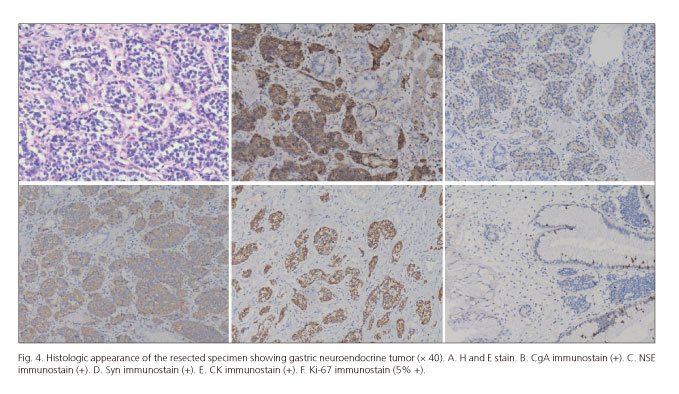
The patient received endoscopic submucosal dissection (ESD) (Fig. 3) and histopathologic examination revealed GNETs with neoplasia-free vertical and radial margins, and the GNET was classified as type I (Fig. 4). He was discharged 5 days after ESD and no melena or recurrence was noted within a follow-up of a month.
Discussion
GNETs arise from enterochromaffin-like cells of the stomach. They represent 8.7% of all gastrointestinal neuroendocrine tumors, and account for 0.6-2% of all gastric polyps identified (5,6). GNETs are classified into four types, based on pathogenesis and histomorphologic characteristics; these types differ in biological behavior and prognosis, ranging from benign to highly malignant biological behavior and extremely poor prognosis (7). Preoperative diagnosis of GNETs remains difficult because of their rarity of occurrence, protean clinical manifestations, and wide variety of radiological and endoscopic presentation. Primary treatment of GNETs includes endoscopic or surgical removal, and endoscopic removal is recommended for GNETs < 20 mm that have not invaded beyond submucosa or otherwise metastasized (6,7). In the present case, the primary symptom was gastrointestinal bleeding and we successfully managed the tumor by endoscopic submucosal dissection. Periodical follow-up is recommended as recurrence may be encountered.
Tan Yuyong1, Dai Yinghuan2, Liu Deliang1 and Huo Jirong1
(huojirong1953@sina.com)
Departments of 1Gastroenterology and 2Pathology. The Second Xiangya
Hospital of Central South University. Changsha, Hunan. China
References
1. Dallal HJ, Ravindran R, King PM, et al. Gastric carcinoid tumour as a cause of severe upper gastrointestinal haemorrhage. Endoscopy 2003;35:716. DOI: 10.1055/s-2003-41506. [ Links ]
2. Schoenfeld R, Cahan J, Dyer R. Gastric carcinoid tumor. An unusual cause of hematemesis. Arch Intern Med 1959;104:649-52. DOI: 10.1001/archinte.1959.00270100135024. [ Links ]
3. Devarbhavi H, Alvares JF. Polypoid gastric carcinoid tumor presenting as hematemesis with prolapse into the duodenum. Gastrointest Endosc 2003;57:618-201. DOI: 10.1067/mge.2003.151. [ Links ]
4. Aguirre A, Cosme A, Bujanda L, et al. Diagnosis, treatment and follow-up of gastric carcinoid tumors. Analysis of 14 cases. Rev Esp Enferm Dig 2011;103:493-4. DOI: 10.4321/S1130-01082011000900011. [ Links ]
5. Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer 2003;97:934-59. DOI: 10.1002/cncr.11105. [ Links ]
6. Delle FG, Kwekkeboom DJ, Van Cutsem E, et al. ENETS Consensus Guidelines for the management of patients with gastroduodenal neoplasms. Neuroendocrinology 2012;95:74-87. DOI: 10.1159/ 000335595. [ Links ]
7. Kulke MH, Shah MH, Benson AB 3rd, et al. Neuroendocrine tumors, version 1.2015. J Natl Compr Canc Netw 2015;13:78-108. [ Links ]