Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 no.2 Madrid feb. 2016
LETTERS TO THE EDITOR
A propos of a case: Abdominal compartment syndrome caused by massive hydatid disease
A propósito de un caso: síndrome compartimental abdominal provocado por hidatidosis masiva
Key words: Hydatid disease. Albendazol. Pericystectomy. Emergency.
Palabras clave: Quistes hidatídicos. Albendazol. Quistoperiquistectomía. Urgencia.
Dear Editor,
For hydatid disease surgery remains the treatment of choice. The surgical technique and approach will depend on location, cyst status and size, and surgical team experience (1). The goal of this letter is to report the clinical case of a patient with a compartment syndrome, suffering from all its pathophysiological consequences, caused by hepatic and abdominal hydatid disease, as well as its two-stage resolution.
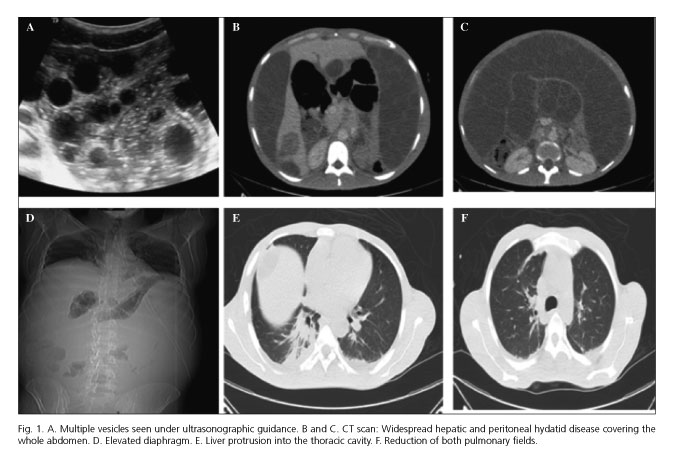
We report the case of a 31-year-old male Moroccan patient from a rural area, with no outstanding medical history, who presented at the emergency room for fever, breathlessness and abdominal pain of one-week duration. Laboratory tests reveal elevated acute-phase reagents, hypoxemia and hypercapnia. Abdominal sonography and a chest-abdominal CT scan revealed an elevated diaphragm, bilateral atelectasis, three large hydatid cysts in the liver -the largest one in segment VI- and massive peritoneal spread (Fig. 1). He was admitted to surgery and developed overall health impairment, somnolence, respiratory distress, oliguria, generalized edema, and evidence of congestive heart failure. An emergency decompressive mini-laparotomy was performed, which removed 13 liters of ascetic fluid and hydatids. Following a favorable recovery a surgical procedure was scheduled after 15 days. It included cholecystectomy, bile tree exam, closed cystectomy for a large mesenteric cyst, open pericystectomy for cysts in segments II-III and VI, and omentectomy with removal of multiple peritoneal cysts. The patient had a satisfactory outcome and was discharged on albendazole.
The relevant literature on this topic is sparse and no therapeutic algorithm is available, hence the modality of choice is selected on a case by case basis (4). Regarding surgery, patients were usually operated upon using non-radical techniques, which have drawbacks such as longer hospital stays, higher relapse risk, and chronic biliary fistulas. It is because of this that total cystectomy/pericystectomy is increasingly considered to be the most appropriate closed technique (5). For massive hepatic hydatid disease (6) radical surgery is a must, and it usually involves significant liver resections because of scarce healthy liver tissue remnants.
Fewer than 10 cases requiring emergency surgery to solve complications have been reported. No study has ever reported a patient with massive hydatid disease requiring two-stage surgery: an initial urgent procedure to reduce abdominal pressure and a second procedure by a team with expertise in hepatobiliary surgery for a definitive management.
Few institutions use a laparoscopic approach for hydatid disease as it is a demanding technique, particularly in poorly accessible sites and given the risk of hydatid spread after accidental cyst rupture. Most papers (7,8) claim that such an approach should only be used in centers specializing in advanced laparoscopy and in highly experienced hepatobiliary units, after proper patient selection, in order to conclude that laparoscopy is safe and comparable to open surgery in terms of radicalness criteria.
Almudena Moreno-Serrano1, Juan José García-Díaz2, Manuel Ferrer-Márquez2,
Pablo Moreno-Marín2 and Paolo Fabiano1
1 Hospital La Inmaculada Huércal-Overa. AGSN. Almería, Spain.
2 Hospital Torrecárdenas. AGSN. Almería, Spain
References
1. Bildik N, Cevik A, Canberk M, et al. Efficacy of preoperative albendazole use according to months in hydatid cyst of the liver. J Clin Gastroenterol 2007;41:312-16. DOI: 10.1097/01.mcg.0000225572.50514.e6. [ Links ]
2. Gupta N, Javed A, Puri S, et al. Hepatic hydatid: PAIR, drain or resect? J Gastrointest Surg 2011;15:1829-36. DOI: 10.1007/s11605-011-1649-9. [ Links ]
3. Ruiz-Tovar J, López-Buenadicha A, Paramo J, et al. Massive recurrence of cyst hydatid disease in the proximal thigh: Unsuccessful conservative treatment with percutaneous, aspiration, ethanol injection y reaspiration. Am Surg 2009;75:439-41. [ Links ]
4. Priego P, Nuño J, López A, et al. Hidatidosis hepática. Cirugía radical vs. no radical: 22 años de experiencia. Rev Esp Enf Dig 2008;100:82-5. [ Links ]
5. El Malki H, Souadka A, Benkabbou A. Radical versus conservative surgical treatment of liver hidatid cyst. Br J Surg 2014:101:669-75. DOI: 10.1002/bjs.9408. [ Links ]
6. Bonfrate L, Giuliante F, Palasciano G, et al. Unexpected discovery of massive liver echinococcosis. A clinical, morphologial and functional diagnosis. Ann Hepatol 2013:12:634-41. [ Links ]
7. Baltar Boileve J, Baamonde de la Torre I, Concheiro Coello P, et al. Laparoscopic treatment of hepatic hydatid cysts: Techniques and post operative complication. Cir Esp 2009;86:33-7. DOI: 10.1016/S2173-5077(09)70069-9. [ Links ]
8. Tuxun T, Aji T, Tai Qw. Conventional versus laparoscopic surgery for hepatic hydatidosis: A 6 year single center experience. J Gastrointestinal Surg 2014;18:1155-60. DOI: 10.1007/s11605-014-2494-4. [ Links ]











 texto en
texto en