My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 n.3 Madrid Mar. 2016
CASE REPORT
Atypical diagnosis by endoscopic capsule: Whipple's disease
Diagnóstico atípico mediante cápsula endoscópica: enfermedad de Whipple
Alba Martínez-Sánchez1, Francisco L. Sánchez-Ceballos1, Servando Fernández-Díez1, María Luisa Suárez-Solís2, Matilde Asteinza-Daganzo1, Walid Baki1, José Miguel Esteban1 and Enrique Rey-Díaz-Rubio1
Departments of 1Digestive Diseases and 2Pathology. Hospital Clínico San Carlos. Madrid, Spain
ABSTRACT
Whipple's disease is a chronic systemic infection produced by the actinomycete Tropheryma whipplei. Endoscopic tests are key in the diagnosis as they allow biopsy and histopathological examination for definitive diagnosis of this entity. We present a case of Whipple's disease where capsule endoscopy, uncommon for the diagnosis of this condition, was essential for it and its performance before and after antibiotic treatment allows to describe the macroscopic evolution of the findings in the small bowel. This case illustrates the usefulness of capsule endoscopy to allow complete examination of the small bowel disease in which up to 30% of patients may present with normal endoscopy.
Key words: Whipple's disease. Capsule endoscopy.
RESUMEN
La enfermedad de Whipple es una infección sistémica crónica producida por el actinomiceto Tropheryma whipplei. Las pruebas endoscópicas son claves en el diagnóstico ya que permiten la toma de biopsia y su estudio anatomopatológico para el diagnóstico definitivo de esta entidad. Presentamos un caso de enfermedad de Whipple en el que la cápsula endoscópica, poco común para el diagnóstico de esta afección, fue clave para el mismo y su realización antes y después del tratamiento antibiótico permite describir la evolución macroscópica de los hallazgos en intestino delgado. Este caso ilustra la utilidad de la cápsula endoscópica al permitir un estudio completo del intestino delgado en esta enfermedad en la que hasta el 30% de los pacientes puede cursar con gastroscopia normal.
Palabras clave: Enfermedad de Whipple. Cápsula endoscópica.
Introduction
Produced by Tropheryma whipplei, Whipple's disease is a rare chronic infectious process that mostly affects the small intestine and may present extraintestinal locations including joints, lungs, central nervous system, heart and eyes, so its clinical presentation may be very heterogeneous with diarrhea, weight loss, asthenia, fever, arthralgia, ataxia and ocular involvement with a subacute course often makes it diagnosis delayed. To achieve the diagnosis it is necessary to identify the presence of foamy, PAS-positive macrophages, which can also be observed using electron microscopy. The diagnosis is confirmed by PCR in the intestinal biopsy, lymph tissue, synovial fluid, blood or cerebrospinal, among others.
It is a fatal disease without treatment which should include antibiotics that cross the blood-brain barrier and keep it for long periods, as despite an initial clinical response is very frequent the recurrence. Endoscopy with biopsy of the second duodenal portion is the diagnostic test of choice, however up to 30% of cases present with a normal endoscopy. In this context, capsule endoscopy shows great use to complete the study of the small intestine.
Case report
A 58-year-old Spaniard man with a past medical history of backache and hyperuricemia and a two-year course of bilateral idiopathic panuveitis. Over the last 6 months complaints of epigastric pain, diarrhea with up to 6-7 stools/day occasionally bloody and constitutional symptoms with loss of 10 kg in weight. The patient denied drinking alcohol or smoking, and did not have any significant familial medical history. Intake of methylprednisolone and omeprazole as regular medication, without consumption of NSAIDs.
Physical examination only highlights underweight. At the beginning, the laboratory tests found hemoglobin 9.2 g/dL, hematocrit 25.8%, VCM 69,8 mm3, serum iron 8 μg/dL, ferritin 94 ng/ml, transferrin 194 (requiring blood transfusions), albumin 2.7 g/dL, prealbumin 8.8 mg/dL, total cholesterol 93 mg/dL, folic acid 3.4 ng/ml and CRP 7.7 mg/dL. Blood test were performed to rule out thyroid or autoimmune diseases (ANA, anticentromere, anti-smooth muscle, antimitochondrial, antiLKM, antireticulin and antitransglutaminase antibodies were negative) as the cause of the clinic, as well as negative stool cultures for parasites, Shigella, Salmonella, Campylobacter, Giardia and Clostridium difficile toxin.
A gastroscopy was performed reaching over the second duodenal portion with diffuse whitish stippling suggestive of lymphoid hyperplasia; tissue simple were obtained resulting duodenal xanthoma under histopathological examination. Colonoscopy findings were inconclusive regarding patient's symptoms. Abdominal CT showed generalized lymphadenopathy: retrocural, hepatic hilum, adjacent to the superior mesenteric vein and in mesenteric fat up to 3 cm, with loops of small intestine without alterations. Laparoscopic biopsy of lymph nodes was being informed as nonspecific reactive changes.
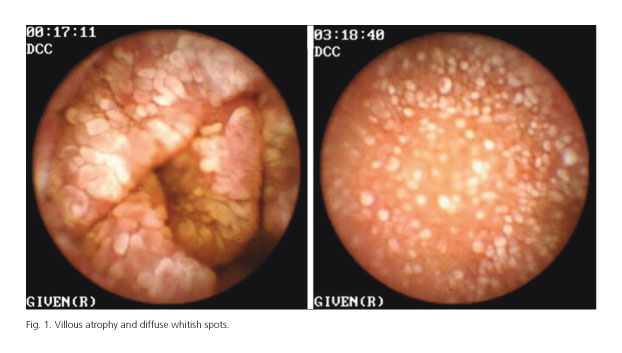
Two months later a Pillcam®SB capsule endoscopy (Given Imaging Ltd., Yoqneam, Israel) was performed according to the chronic diarrhea workup, revealing a diffuse pattern or mucosal involvement in terms of breaks and villous atrophy and disarrangement mucosa. The most prominent finding was a whitish spots on the surface of the mucosa around its all circumference (Fig. 1). Areas of erosions and images of mucosal haemorrhages were also observed. This features involved the intestinal mucosa from distal duodenum to the ileum, recommending endoscopy sample. Push enteroscopy confirmed CE findings and samples taken for histological examination showed PAS-positive macrophages, negative Ziehl, suggestive of Whipple's disease (Figs. 2 and 3).
Given the findings in complementary tests, antibiotic treatment was started initially with intravenous ceftriaxone for 14 days followed by oral cefixime for 1 year. The patient improved clinically with significant weight gain and normalization of his bowel habits. It was decided to test the mucosal evolution performing follow-up endoscopic control capsules. At 8 months of starting antibiotic therapy, mucosal improvement was observed with persistent areas of cracked hyperemic mucosa and isolated erosions seen in all segments of the small intestine as the capsule moved distally (Figs. 4 and 5).
At 15 months normal mucosa was observed in the region which seemed to correspond to distal duodenum and ileum, with persisting cracked mucosa in the rest of the small intestine (Figs. 6 and 7). Finally, at 30 months morphology of small bowel folds has nearly normalized with minimal tiny of villi (Fig. 8).
Discussion
Whipple's disease, also called intestinal lipodystrophy, is an infectious multisystem rare condition (30 cases/year) caused by Tropheryma whipplei. Whipple first described in 1907 this systemic disease caused by a gram positive bacillus. However, it was not until 2000 when the first culture was obtained. Although T. whipplei commonly infects humans, classic Whipple's disease is rare. It seems that could be an opportunistic bacterium that causes chronic infections in genetically susceptible patients. Its incidence has been increased in the Caucasian, median age (40-50 years), farmers, and exposure to sewage. The prevalence in the adult population could reach 50-70% depending on the geographic area (1), being endemic in certain areas of Senegal. The bacterium is most likely transmitted among humans via the oro-oral and the feco-oral routes.
The infection can lead to an asymptomatic carrier state, classic or disseminated Whipple's disease that usually is preceded by arthralgia and localized infections such as endocarditis or encephalitis (2). It has recently been associated with acute infections such as gastroenteritis, pneumonia or bacteremia (2).
The classic disease typically affects middle-aged men. It has been described four late cardinal clinical manifestations of the disease: arthralgias (migratory, large joints that may precede other symptoms in years), weight loss, diarrhea and abdominal pain (3,4).
Although mainly affects the intestine, its clinical spectrum is very heterogeneous and can affect the heart, lungs, CNS, eyes, hematopoietic system, endothelium, lymph nodes (5) or skin. Neurological symptoms are present in up to 25% of patients including cognitive impairment, psychiatric symptoms, supranuclear ophthalmoplegia and oculomasticatoria miorritmia (considered pathognomonic sign), among others.
Due to it being a rare disease along with the absence of specific clinical data, diagnosis and usually has been delayed years between the onset of symptoms and diagnosis.
Diagnostic confirmation is obtained in the presence of PAS-positive macrophages and villous atrophy in mucosal biopsies, identification of T. whipplei by electron microscopy or by identification of bacterial RNA by PCR techniques. All these tests show a similar sensitivity (10). Through optical microscopy, the whitish-yellowish plaques reflect lipid deposits or linfagiectasia while villous distension is due to macrophage infiltration of the lamina propria. Swollen cytoplasm of macrophages becomes foamy when stained with hematoxylin and eosin, but numerous granular particles become visible when the PAS is used. These particles correspond to the phagosome filled with numerous T. whipplei and positive reaction with PAS reflects the glycoproteins content of the bacterial cell wall.
Before the antibiotic era, Whipple's disease was always fatal, most frequently due to severe malabsorption. Antibiotics crossing the blood brain barrier are preferably used during treatment and should be continued at least 1 year with subsequent follow up. It is suggested starting antibiotics with ceftriaxone (2 g i.v., day) or penicillin (2 MU i.v. every 4 hours) for 2 weeks followed by trimethoprim-sulfamethoxazole (160 mg TMP/SMX 800 mg every 12 hours) for a year. For classic Whipple's disease, Fenollar et al. suggest a combination of doxycycline (200 mg/day) and hydroxychloroquine (200 mg, 3 times daily) for 1 year (2). Because of relapses, narrow control and follow-up of these patients should be performed. It should not be forgotten that Whipple's disease is a disease that can present with recurrence by up to 20% of cases, even affecting organs other than the previously described and given the lethal potential of cardiac or neurological relapses could be considered treatment with doxycycline for lifetime. At present there are no specific treatment recommendations for asymptomatic carriers and acute infections.
The resolution is generally complete and there may be irreversible neurological sequelae. The checking of the cure is based on the clinical improvement (typically diarrhea and malabsorption improve in weeks), with PCR techniques (turned negative quickly with efficient therapy) and repeated endoscopic biopsies (histological changes can persist for years) (10).
Capsule endoscopy is a noninvasive diagnostic tool that allows an appropriate study of the small intestine and which in our case had a key role to achieve the diagnosis, since the initial duodenal biopsies were nondiagnostic and of the intra-abdominal lymph nodes were nonspecific.
In the literature there are few cases that describe the findings of the CE in this disease, but they are coincident in the existence of villous atrophy, erosions, lymphatic dilation, areas of denuded mucosa and especially diffuse whitish stippling (6,8,11-13), described also when associated with Giardia coinfection (14).
These findings do not usually affect the small intestine in a continuous manner, but they are often subtle or discontinuous (8) injuries that hinder and delay the diagnosis in many cases.
Fritscher-Ravens (8) postulates that intestinal malabsorption could be associated with accelerated intestinal transit in these patients based on a case of Whipple's disease with a CE transit time by small bowel of 163 minutes. Beyond the difficulty of relating the transit time of the CE by small bowel with intestinal motility, Gay et al. (11) publish their experience with a patient in whom is performed a CE at the diagnosis and 10 weeks after the initiation of antibiotic treatment with a transit time of 425 and 274 minutes, respectively, so Whipple's disease may delay intestinal transit. In our case transit time of the small bowel CE was 260 minutes at diagnosis, 215 minutes at 8 months, 230 minutes at 15 months and 227 minutes at 30 months. Although transit times by small intestine does not differ greatly in the different explorations, in the first CE is superior to other controls, so the local inflammatory bowel wall may decrease small bowel motility and malabsorption in this context would be secondary to the morphological changes consequences of the disease.
After the establishment of the antibiotic, Dzirlo et al. (12) describes an improvement and resolution of macroscopic findings described in the CE that seem to start in the more distal parts of the small bowel and progress proximally. However, in our case, this improvement does not follow this macroscopic distribution and in the capsules done in an evolutionary form a trend to decrease in injuries in a patched form is observed. Dzirlo describes the findings in two cases in which the CE is performed on an evolutionary basis, one at 9 months after initiation of treatment in which there are still mucosal alterations and the other at 29 months after initiation of treatment with normal mucosa. The resolution times of macroscopic findings agree with those observed in our case where the mucosal lesions persist at 8 months, and at 30 months the mucosa has an almost normal appearance, which shows that the macroscopic restitution may take years to achieve.
In conclusion, Whipple's disease is a rare multisystem disorder whose main involvement is located in the small bowel. Usually the endoscopy with biopsy of the second duodenal portion allows the diagnosis, but up to 30% present with a normal gastroscopy (9). Capsule endoscopy, noninvasive exploration and whose ultimate goal is the study of all the small bowel can be useful if suspecting this disease since it identifies the spread of the lesions and check its evolution.
References
1. Fenollar F, Keita AK, Buffet S, et al. Intrafamilial circulation of Tropheryma Whipple, France. Energ Infect Dis 2012;18:949-55. [ Links ]
2. Fenollar F, Lagier JC, Raoult D. Tropheryma whipplei and Whipple's disease. Journal of Infection 2014;69:103-12. DOI: 10.1016/j.jinf. 2014.05.008. [ Links ]
3. Marth T, Raoult D. Whipple's disease. The Lancet 2003;361:239-46. DOI: 10.1016/S0140-6736(03)12274-X. [ Links ]
4. Durand DV, Lecomte C, Cathébras P, et al. Whipple disease. Clinical review of 52 cases. The SNFMI Research Group on Whipple Disease. Société Nationale Française de Médecine Interne. Medicine (Baltimore) 1997;76:170-84. DOI: 10.1097/00005792-199705000-00003. [ Links ]
5. Coli MV, Chebli JMF, Gaburri PD. Gastrointestinal: Whipple's disease. J Gastroentero Hepatol 2007;22:136. DOI: 10.1111/j.1440-1746.2006.04816.x. [ Links ]
6. Keane MG, Shariff M, Stocks J, et al. Imaging of the small bowel by capsule endoscopy in Whipple's disease. Endoscopy 2009;41(Supl. 2):E139. DOI: 10.1055/s-0028-1119729. [ Links ]
7. Monkemuller K, Fry LC, Von Arnim U, et al. Whipple's disease: An endoscopic and histologic study. Digestion 2008;77:161-5. DOI: 10.1159/000140978. [ Links ]
8. Fritscher-Ravens A, Swain CP, von Hervia A. Refractory Whipple's disease with anaemia: First lessons from capsule endoscopy. Endoscopy 2004;36:659-62. DOI: 10.1055/s-2004-814537. [ Links ]
9. Ratnaike RN. Whipple's disease. Postgrad Med J 2000;76:760-6. DOI: 10.1136/pmj.76.902.760. [ Links ]
10. Radu B, Bengus A, Marinescu M, et al. First Pillcam Colon 2 capsule images of Whipple's disease: Case report and review of the literature. World J 11. Gastrointest Endosc 2012;4:575-8. DOI: 10.4253/wjge.v4.i12.575. [ Links ]
11. Gay G, Roche F, Delvaux M. Capsule endoscopy, transist times and Whipple's disease. Endoscopy 2005;37:272-4. DOI: 10.1055/s-2005-861012. [ Links ]
12. Dzirlo L, Blaha B, Müller C, et al. Capsule endoscopy of the small intestine in Whipple's disease and the changes that occur during antibiotic therapy. Endoscopy 2007;39(Supl. 1):E207-8. DOI: 10.1055/s-2006-944990. [ Links ]
13. Roulet J. Capsule endoscopy in Whipple's disease. Clin Gastroenterol Hepatol 2013;11:26 DOI: 10.1016/j.cgh.2013.01.018. [ Links ]
14. Urién-Fernández I, Carretero C, Sola J, et al. Refractory Whipple's disease. Gastrointest Endosc 2007;65:521 DOI: 10.1016/j.gie.2006.06.073. [ Links ]
![]() Correspondence:
Correspondence:
Alba Martínez Sánchez.
Department of Digestive Diseases.
Hospital Clínico San Carlos.
C/ Doctor Martín Lagos, s/n.
28040 Madrid, Spain
e-mail: almartinezsanchez@gmail.com
Received: 04-02-2015
Accepted: 09-03-2015











 text in
text in