Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Española de Enfermedades Digestivas
versão impressa ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 no.4 Madrid Abr. 2016
LETTERS TO THE EDITOR
Hiatal herniation following total gastrectomy
Key words: Diafragmatic hernia. Gastrectomy. Esophagectomy.
Dear Editor,
The authors present a case of early hiatal hernia (HH) that recurred a week after. Our purpose in this case report is to discuss briefly the potential cause and to enhance the importance of computed tomography (CT).
Case report
The patient was a 69-year-old male with advanced gastric cancer of the cardias who underwent total gastrectomy, lower esophagectomy, with antecolic Roux-en-Y reconstruction.
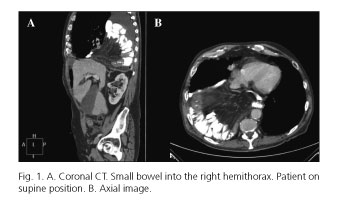
Thirty days after surgery, he presented to the emergency department with orthopnea. A CT scan reported that both small and large bowel were herniated into the right hemithorax (Fig. 1). Patient was admitted for urgent laparotomy with intraoperatory findings of a transdiaphragmatic evisceration into the thorax. After hernia reduction, the hiatal defect was closed with polypropilen interrupted sutures.
On the 7th day, our patient started with dyspnoea again. We repeated the CT; images showed a relapse of abdominal content herniated into the thorax. Our patient was operated on again and, this time, a mesh of BioA© was fixed with interrupted sutures.
He was discharged 28 days after admission; a previous CT was done, with no findings.
Discussion
Incidence of HH after esophagectomy ranges from 0.05% (1) to 19.4% (2) in some series.
The enlargement of the hiatus after esophagectomy makes patients prone to HH, with higher incidence after transhiatal esophagectomy (3), as it was our case. Patients with high body mass index (BMI) are less prone to have a HH postesophagectomy; our patient's BMI was 25. Another predisposing factor is the pressure gradient between thoracic and abdominal cavities.
Incarceration may appear sooner or later, with a wide range of clinical symptoms. Clinical suspicion based on patients background and early CT scan is very important in the detection of this pathology (3).
Primary repair may be done by reapproximating diaphragmatic crura. In the recurrence, the repair may require the use of meshes (3,4). Despite mesh repair, HH can recur (5).
María Azucena Gonzalo, Helen Almeida and Antonio Güemes
Department of General Surgery, Esophagogastric Unit.
Hospital Universitario Lozano Blesa. Zaragoza, Spain
References
1. Yang Y, Yan W, Xiong H, et al. Analysis of 19 cases undergoing reoperation for complications following esophagectomy. Zhonghua Wei Chang Wai Ke Za Zhi 2014;17:492-4. [ Links ]
2. Sutherland J, Banerji N, Morphew J, et al. Postoperative incidence of incarcerated hiatal hernia and its prevention after robotic transhiatal esophagectomy. Surg Endosc 2011;25:1526-30. DOI: 10.1007/s00464-010-1429-8. [ Links ]
3. Ganeshan DM, Correa AM, Bhosale P, et al. Diaphragmatic hernia after esophagectomy in 440 patients with long-term follow-up. Ann Thorac Surg 2013;96:1138-45. DOI: 10.1016/j.athoracsur.2013.04.076. [ Links ]
4. Jeng KS, Huang CC, Lin CK, et al. Early incarcerated diaphragmatic hernia following right donor hepatectomy: A case report. Transplant Proc 2015;47:815-6. DOI: 10.1016/j.transproceed.2015.02.001. [ Links ]
5. Kent MS, Luketich JD, Tsai W, et al. Revisional surgery after esophagectomy: An analysis of 43 patients. Ann Thorac Surg 2008;86:975-83; discussion 967-74. DOI: 10.1016/j.athoracsur.2008.04.098. [ Links ]