Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 no.10 Madrid oct. 2016
https://dx.doi.org/10.17235/reed.2016.4410/2016
ORIGINAL PAPERS
How is inflammatory bowel disease managed in Spanish gastroenterology departments? The results of the GESTIONA-EII survey
¿Cómo se maneja la enfermedad inflamatoria intestinal en los servicios de digestivo en España? Resultados de la Encuesta GESTIONA-EII
Manuel Barreiro-de-Acosta1, Federico Argüelles-Arias2, Joaquín Hinojosa3, Javier Júdez-Gutiérrez4 and José María Tenías5
1Hospital Universitario de Santiago de Compostela. A Coruña, Spain.
2Hospital Universitario Virgen Macarena. Sevilla, Spain.
3Hospital de Manises. Valencia, Spain.
4Departamento de Gestión del Conocimiento. SEPD. Spain.
5Department of Preemptive Medicine. Hospital Pare Jofré. Valencia, Spain.
ABSTRACT
Introduction: Not all national health centers include specialized units or clinicians devoted to inflammatory bowel disease. The goal of the survey was to gain an insight into the management of this disease within Spanish gastroenterology departments via a survey among their members.
Material and methods: An online survey was conducted in February and March 2015, among SEPD members (2017 clinician members), who were split into three categories: heads of department, general gastroenterologists, and experts in this disease. The results of the last two surveys are reported, including demography-related questions and specific questions on the strategies and resources available for the care of these patients.
Results: A total of 166 responses were received (response rate 8.19%), excluding those from heads of department (previously published). Sixty gastroenterologists considered themselves experts in inflammatory bowel disease, and 106 non-experts in it, the latter being either general gastroenterologists or specialists in other areas, mainly endoscopy. Twenty-eight percent of non-expert gastroenterologists said their hospitals had specific units, with a monographic clinic in 46%. However, 26% reported that they were treating affected patients themselves. Experts in inflammatory bowel disease reported that their institute had resources to support their work, but there was a lack of surgeons with expertise in this condition, particularly in county hospitals.
Conclusions: At least, within SEPD members, 2 out of 3 experts in inflammatory bowel disease seem to have the resources available for their work (nurses, day unit, telephone line, database, referrals, joint sessions). Although there is room for improvement (email to contact patients, devoted surgeon, absence of referral protocols), and 2 out of 3 are concerned about pharmacy costs. Since a substantial number of patients remain treated by general practitioners, rapid referral programs might be helpful in this setting.
Key words: Inflammatory bowel disease. Resources.
RESUMEN
Introducción: no en todos los centros nacionales existen unidades ni especialistas dedicados a la EII. El objetivo de la SEPD fue conocer, a través de una encuesta a sus socios, datos sobre el manejo de la EII en los servicios de digestivo de España.
Material y métodos: encuesta en línea (telemática) realizada entre el 2 de febrero y el 9 de marzo de 2015, a socios de la SEPD (remitida a 2.017 socios numerarios con actividad clínica) divididos en tres categorías: jefes de servicio, digestivos generales y digestivos especializados en EII. Se muestran los resultados de las últimas dos incluyendo preguntas demográficas y otras más específicas sobre el modo y recursos con los que se cuenta para atender a estos pacientes.
Resultados: se recibieron 166 encuestas completas (tasa de respuesta del 8,19%, con distribución entre todas las CC. AA. menos La Rioja), excluyendo las de los jefes de servicio. Sesenta digestivos se consideraban expertos en EII y 106 se consideraban no expertos en EII, bien generales o especializados en otros ámbitos, siendo el principal el área de endoscopias. Un 28% de los digestivos no expertos afirmaron que sus hospitales tienen unidades de EII y en un 46% existe una consulta monográfica. Pero un 26% refería que ellos mismos son los que ven y tratan los pacientes de EII. Los digestivos expertos en EII refieren disponer de una estructura con recursos para desarrollar su tarea aunque existe carencia de cirujanos expertos en EII sobre todo en centros comarcales.
Conclusiones: al menos 2 de cada 3 expertos en EII, socios de la SEPD parecen disponer de recursos para desarrollar su tarea (enfermería, unidad de día, línea telefónica, base de datos, derivación, sesiones conjuntas). Existe ámbito de mejora (correo-e para contacto con pacientes, cirujano con dedicación específica, ausencia de protocolos de derivación) y 2 de cada 3 están preocupados por el control del gasto farmacéutico. Dado que un número de pacientes considerable sigue siendo tratado por médicos generalistas, programas para favorecer una rápida derivación podrían ayudar.
Palabras clave: Enfermedad inflamatoria intestinal. Gestión clínica.
Introduction
Inflammatory bowel disease (IBD) is doubtlessly an increasingly common condition with ever increasing incidence and prevalence over the last few years, particularly in Western countries (1,2). Currently, the highest incidence in Europe is 24.3 cases per 100,000 people/year for ulcerative colitis (UC), and 12.7 cases per 100,000 people/year for Crohn's disease (CD). The annual prevalence of CD is 322 per 100,000 people in Europe, and 319 per 100,000 in North America.
Furthermore, given this strong increase, IBD units are clearly necessary to provide IBD patients with optimum care, as they often require a personalized strategy with therapies requiring more stringent control measures than usual (3,4). Also, multidisciplinary teams are needed to provide appropriate care of the wide range of symptoms of this disease (5).
However, despite the aforementioned prevalence, not all Spanish centers have IBD units; many do not even have expert IBD specialists. Based on this, the "Sociedad Española de Patología Digestiva" (SEPD), a scientific society of all Spanish gastroenterologists (GEs) which includes not only specialists in a specific area as seen in other other societies (6-8), attempted to gain insight into the management of IBD within Spanish GE departments via a survey of its members. As information on the management of this condition in many units is scarce; the survey also explored the relevance of the condition in GE units, and their available resources for patient care.
Objetives
The study aimed at gaining insight into the management of IBD within Spanish GE departments, and into IBD-related managerial aspects as per the different categories identified (head of department, expert IBD gastroenterologists, general gastroenterologists).
Material and methods
An online survey was submitted by SEPD to its practicing full members (2027 as of February, 2015). Members were asked whether they were heads of department, or considered themselves experts in IBD, or had no specific area of expertise. Thus, they were redirected to a category-specific survey. Each survey had a general portion, dealing with general and demographic data as pertaining to the responder and his or her department. A second, more specific portion followed.
Surveys were submitted from February 2 to March 9, 2015, as follows:
1. The first one was sent to heads of department to inquire about the significance bestowed upon IBD and on therapy costs. This first section was recently reported as a letter to the editor (9).
2. The second survey was sent to general GEs and focused on obtaining information regarding the way they care for patients with IBD or refer them to specialist units,. This survey included 10 items to address issues such as when and how newly diagnosed patients are managed, the presence of referral circuits, etc. (Annex 1).
3. The third survey was sent to expert IBD doctors in order to obtain information on the managerial and structural issues entailed by the management of these patients. This survey included 32 items inquiring about the number of patients cared for and on the availability of telephone lines, e-mail, day units, nurses, etc. (Annex 2).
A descriptive statistical analysis was carried out using the IBM SPSS Statistics®, version 23.0, software. Results are expressed as percentages. When comparing unit structures according to hospital size the chi-square statistic was used, assuming statistically significant differences for p < 0.05.
Results
A total of 166 completed surveys were received, aside from those received from heads of departments. Sixty GEs considered themselves IBD experts, and 106 thought otherwise, such as general GEs or GEs specialists of other disciplines, mainly endoscopy.
After analyzing both sets of surveys the following results were obtained:
Results obtained from non-IBD experts
Regarding the demographic distribution of the 106 GEs who did not declare specific expertise in IBD, covering 16 autonomous communities (all except La Rioja), 55% were males, and the commonest age range was 31-40 years. Regarding hospital type, 25% worked at county hospitals, 20% at general hospitals, and 55% at university or tertiary hospitals; 38% were mainly endoscopists, 35% worked mainly at the general outpatient clinic, and 20% worked mainly at the hospital ward.
A total of 28% of respondents reported IBD units in their hospitals, with a monographic IBD clinic in 46% of cases. However, 26% reported that they themselves saw and treated patients with IBD. When asked about the number of visits, 50% saw fewer than 10 patients/year and only 6% followed up over 100 patients/year.
Regarding specific scenarios, most significant results include the following: when IBD is suspected, only 11% of patients are referred; when IBD was recently diagnosed, 46% are referred to a specialist. Referral to IBD units varies according to patient treatment. Thus, 16% of patients on mesalazine alone are referred, 46% of those requiring an immunomodulator are referred, and 62% of cases requiring a biologic are referred.
Appointment delays is no doubt a significant factor for a GE department; figure 1 shows the time taken for a patient to be seen in a reference unit following his or her referral from a non-IBD specialist. It takes longer than 1 month for 34% of cases.
A stratified sub-analysis was performed according to GE age (> or < 40 years) and hospital type. No statistically significant differences were seen in attitude, either clinical or therapeutically, between both groups in any of the suggested scenarios. As per hospital type, no significant changes in referral time or referral behavior for suspected IBD cases were seen; however, changes were seen and proven significant for newly diagnosed IBD cases. In a county, second-tier hospital, 75% of patients are followed up by the same GE, whereas 65% are referred to an IBD unit in a university ortertiary hospital. Differences between treatment scenarios were also seen (Annex 1). Patients on mesalazineare were referred to IBD units in 25% of cases in a tertiary hospital, versus 0% in a county site; percentages are 50% vs. 8% for patients on immunosuppressants, and 77% vs. 38% for patients on biologics.
Results obtained from expert IBD gastroenterologists
Regarding the demography of the 60 GEs from 15 autonomous communities (all except La Rioja and Extremadura) who claimed to be experts in IBD, 70% were males, with the commonest age range between 41 and 50 years. With regard to hospital type, 44% worked at county hospitals, 26% at general hospitals, and 30% at university or tertiary hospitals. Regarding the numbers of patients seen at the various sites included in the survey, 8% had a clinic with 100 to 200 patients, 22% had 200 to 500 patients, 26% saw 501 to 750 patients, 12% had 750 to 1000, and 32% saw over 1,000 patients. According to these data, the number of patients seen oscillates between 28,000 and 38,000. A total of 88.9% of respondents reported working at an IBD clinic or monographic practice, but the number of physicians in these units and the number of visits per week varied significantly according to hospital type, with higher figures reported for tertiary sites (Fig. 2).
Particularly interesting data include the fact that 74.1% had supporting nurses and 100% had access to a day hospital for the administration of intravenous medication, albeit only 9% had their own specialty-related day hospital, and 91% shared this resource with other units.
With regards to other specific questions, 94.4% of respondents reported seeing urgent cases in their clinic without an appointment. A telephone line for patient concerns was available to 78%, and an e-mail service was only available for 38% of respondents. A total of 68% had an IBD patient database, and 46% had access to the GETECCU (Grupo Español de Trabajo en Enfermedad de Crohn y Colitis Ulcerosa) ENEIDA program.
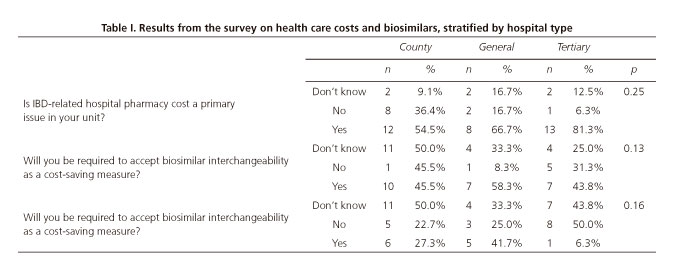
With regard to healthcare costs, 66% of respondents reported that hospital pharmacy costs were a major issue for their department; with regard to biosimilars, 48% thought their initial use would be mandated by the authorities, and 24% believed interchangeability would be mandatory. When all three questions are analyzed per hospital type, while no significant differences are seen (Table I), higher cost concerns were identified in tertiary hospitals and lack of awareness about biosimilars is greater in smaller hospitals.
Overall, 84% of respondents reported joint sessions with other units, and 62% had a reference surgeon for patients with IBD, with significant differences between hospital types (p < 0.01), while only 13% of tertiary hospitals have a surgeon, 93% of tertiary centers have one for referral. As for the presence of protocols for the referral of patients to the IBD clinic or unit, 55% of hospital did not have one.
Discussion
The results of the Project GESTIONA-EII, undertaken using online surveys with SEPD members, allowed an overall assessment of IBD status in our country. These surveys provided information beyond the views of GEs who consider themselves IBD experts - other scientific associations such as ECCO (European Crohn's and Colitis Organization) and GETECCU have already performed surveys (10,11), and drawn interesting conclusions on topics ranging from biosimilar awareness to satisfaction with care. The value of the present survey is likely related to the fact that SEPD includes a large number of gastroenterologists, many of them unrelated to IBD, which will allow "external" but close data on IBD that cannot be obtained from studies by societies devoted to more specific areas of gastroenterology.
The results of the GESTIONA-EII survey of non-IBD expert GE specialists provided interesting information on the ways referrals occur to specialist units. Interestingly, a high percentage of centers do not refer patients. It should be highlighted that 1 in 4 gastroenterologists with no expertise in IBD, follow up patients with this condition, although most do so with fewer than 10 patients per year; this does not seem a positive factor for patients. Two studies in Spain and Portugal comparing care between sites mainly with IBD units (Spain) and sites mainly with general GEs (Portugal), immunosuppressants and biologics were most widely used in specialist units both for CD and UC, which was reflected by fewer surgical procedures for IBD patients (12,13). Over 50% of patients with IBD are still cared for by general GEs, but referral to specialists units increases with IBD severity, thus patients on mesalazine are are hardly ever referred whereas those on biologics are more often referred, likely due to a more complex management and the fact that these doctors have better access to clinical recommendations and guidelines (14). However, nearly 40% keep their patients on biologics, but less so at university hospitals (change doctors within same site) as compared to county centers. Staying within the same site likely favors higher referral rates. Time to care is an issue reported by non-IBD experts, which may have a significant impact on severe cases, hence the need to implement easy-flowing referral methods in sites for the near future.
The high participation of IBD experts, and the fact that 60 SEPD members "define themselves" as such, is to be highlighted, and also corroborates the relevance gained by IBD in our specialty over the past few years, with significant increases in both communications at meetings and papers in scientific journals. Many factors may influence this fact, including the well-known increased incidence in our setting, now similar to that of other countries across Europe (15). The number of participating experts in IBD is even more relevant given the number of patients they include, which oscillates between 28,000 and 38,000, considerable figures when discussing the results obtained.
Some of the data obtained warrant particular comment. Some aspects are highly positive: most centers provide emergency care, have telephone visits available, and have nurses in their units, all of which is highly beneficial for patient-doctor interactions (16,17). However, other aspects are negative, including the fact that nearly 40% have no surgeon specialist in IBD, which is clearly non-beneficial for patients as, the higher the number of annual surgeries for IBD, the lower the number of complications (18). This illustrates the fact that the parameters required to consider a GEs a specialist in IBD still remain to be defined. Where advances have recently taken place, also pioneered in Spain by GETECCU, is in the definition of the standards a unit must meet to be considered an IBD unit. Thus, a paper was recently reported by different care providers (GEs, surgeons, nurses) that was based on the Delphi method, which selected 56 items to be considered when assessing a unit (19). Similar initiatives have taken place in other countries such as the USA (20). Thus, in the near future, these tools will be used in clinical practice to assess which professionals may form part of a specialist unit.
A major concern among IBD experts is healthcare costs. In other countries with public health systems such as Canada, drug costs have been shown to burden IBD costs (21). While various studies and reviews considering indirect costs have shown the cost-effectiveness of biologic therapy (22), cost concerns remain a priority not only for governments but also for IBD experts, as revealed by our survey. The advent of biosimilars, especially infliximab's, is no doubt a key aspect in a novel paradigm to keep costs down in an attempt to reduce drug costs (23). However, concerns about their use persist, with highly different opinions amongst GEs. Specialists in county centers seem to be less familiar with biosimilars, hence the need for initiatives such as SEPD's to provide members with information on these new drugs (24). Similarly, the notion of mandatory interchangeability is more predominant in smaller hospitals.
The main strengths of the study include a high number of specialists and wide geographical outreach, as well as an in-depth exploration of aspects such as healthcare costs and resource management, including the direct views of respondents. However, the present study has a number of limitations such as the fact that it is a voluntary survey aimed at society members where opinion accuracy cannot be validated. It also exhibits a participation bias, since practitioners minimally interested in IBD may choose not to respond. Thus, some results must be assessed in greater depth before their extrapolation to all practitioners may be envisaged.
To conclude, the results of the GESTIONA-EII survey allow us to conclude that at least 2 of every 3 SEPD experts in IBD seemingly have enough resources available for their work (nurses, day unit, telephone line, database, referral, joint sessions). There is room for improvement (e-mail for patient contact, devoted surgeon, absence of referral protocols), and 2 out of every 3 respondents are concerned with drug costs control (proportion increases with hospital level), feeling uncertain about the impact biosimilars may have on their practice. Also, a considerable number of patients are still managed by general practitioners, and programs favoring fast, easy-flowing referrals will likely help in correcting or improving this situation.
Conflict of interest
This survey has been promoted and executed by SEPD. Both this organization and the authors of the paper have worked with full scientific independence and they declare no conflict of interest related with this work. Nonetheless, several of the authors (MB, FA, JH) and SEPD have received, on several occasions sponsorships or grants from companies with interest in IBD.
References
1. M'Koma AE. Inflammatory bowel disease: an expanding global health problem. Clin Med Insights Gastroenterol 2013;6:33-47. DOI: 10.4137/CGast.S12731. [ Links ]
2. Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology 2012;142(1):46-54.e42; quiz e30. DOI: 10.1053/j.gastro.2011.10.001. [ Links ]
3. Barreiro-de-Acosta M. The importance of the interaction between doctor and patient with inflammatory bowel disease. Rev Esp Enferm Dig 2014;106(6):369-71. [ Links ]
4. Mawdsley JE, Irving PM, Makins RJ, et al. Optimizing quality of outpatient care for patients with inflammatory bowel disease: the importance of specialist clinics. Eur J Gastroenterol Hepatol 2006;18(3):249-53. DOI: 10.1097/00042737-200603000-00004. [ Links ]
5. Mikocka-Walus AA, Andrews JM, Bernstein CN, et al. Integrated models of care in managing inflammatory bowel disease: a discussion. Inflamm Bowel Dis 2012;18(8):1582-7. DOI: 10.1002/ibd.22877. [ Links ]
6. Argüelles-Arias F, Rodríguez Ledo P, Tenías JM, et al. The management of lactose intolerance among primary care physicians and its correlation with management by gastroenterologists: the SEPD-SEMG national survey. Rev Esp Enferm Dig 2015;107(9):554-8. DOI: 10.17235/reed.2015.3771/2015. [ Links ]
7. Argüelles-Arias F, Tenías JM, Casellas-Jordá F, et al. Results of a nation-wide survey on hypolactasia--how is this condition diagnosed and managed in our setting? Rev Esp Enferm Dig 2015;107(1):55-6. [ Links ]
8. Lucendo AJ, González-Huix F, Tenias JM, et al. Gastrointestinal endoscopy sedation and monitoring practices in Spain: a nationwide survey in the year 2014. Endoscopy 2015;47(4):383-90. DOI: 10.1055/s-0034-1391672. [ Links ]
9. Argüelles Arias F, Barreiro-de Acosta M, Hinojosa J. Pharmaceutical costs for inflammatory bowel disease units - An issue for department heads? The GESTIONA EII survey. Rev Esp Enferm Dig 2016;108(6):380-1. DOI: 10.17235/reed.2016.4192/2016. [ Links ]
10. Casellas F, Vera I, Ginard D, et al. Inflammatory bowel disease patient's satisfaction with healthcare services received. Physicians' and nurses' perceptions. Rev Esp Enferm Dig 2013;105(7):385-91 DOI: 10.4321/S1130-01082013000700003. [ Links ]
11. Danese S, Fiorino G, Michetti P. Viewpoint: knowledge and viewpoints on biosimilar monoclonal antibodies among members of the European Crohn's and Colitis Organization. J Crohns Colitis 2014;8(11):1548-50. DOI: 10.1016/j.crohns.2014.06.007. [ Links ]
12. Barreiro-de Acosta M, Magro F, Carpio D, et al. Ulcerative colitis in northern Portugal and Galicia in Spain. Inflamm Bowel Dis 2010;16(7):1227-38. DOI: 10.1002/ibd.21170. [ Links ]
13. Magro F, Barreiro-de Acosta M, Lago P, et al. Clinical practice in Crohn's disease in bordering regions of two countries: different medical options, distinct surgical events. J Crohns Colitis 2010;4(3):301-11. DOI: 10.1016/j.crohns.2009.12.004. [ Links ]
14. Cabriada JL, Vera I, Domènech E, et al. Recommendations of the Spanish Working Group on Crohn's Disease and Ulcerative Colitis on the use of anti-tumor necrosis factor drugs in inflammatory bowel disease. Gastroenterol Hepatol 2013;36(3):127-46. DOI: 10.1016/j.gastrohep.2013.01.002. [ Links ]
15. Burisch J, Pedersen N, Čuković-Čavka S, et al. East-West gradient in the incidence of inflammatory bowel disease in Europe: the ECCO-EpiCom inception cohort. Gut 2014;63(4):588-97. DOI: 10.1136/gutjnl-2013-304636. [ Links ]
16. Hernández-Sampelayo P, Seoane M, Oltra L, et al. Contribution of nurses to the quality of care in management of inflammatory bowel disease: a synthesis of the evidence. J Crohns Colitis 2010;4(6):611-22. DOI: 10.1016/j.crohns.2010.08.009. [ Links ]
17. Ramos-Rivers C, Regueiro M, Vargas EJ, et al. Association between telephone activity and features of patients with inflammatory bowel disease. Clin Gastroenterol Hepatol 2014;12(6):986-94.e1. DOI: 10.1016/j.cgh.2013.11.015. [ Links ]
18. Nguyen GC, Steinhart AH. The impact of surgeon volume on postoperative outcomes after surgery for Crohn's disease. Inflamm Bowel Dis 2014;20(2):301-6. DOI: 10.1097/01.MIB.0000438247.06595.b9. [ Links ]
19. Calvet X, Panés J, Alfaro N, et al. Delphi consensus statement: Quality Indicators for Inflammatory Bowel Disease Comprehensive Care Units. J Crohns Colitis 2014;8(3):240-51. DOI: 10.1016/j.crohns.2013.10.010. [ Links ]
20. Melmed GY, Siegel CA, Spiegel BM, et al. Quality indicators for inflammatory bowel disease: development of process and outcome measures. Inflamm Bowel Dis 2013;19(3):662-8. DOI: 10.1097/mib.0b013e31828278a2. [ Links ]
21. Bernstein CN, Longobardi T, Finlayson G, et al. Direct medical cost of managing IBD patients: a Canadian population-based study. Inflamm Bowel Dis 2012;18(8):1498-508. DOI: 10.1002/ibd.21878. [ Links ]
22. Tang DH, Harrington AR, Lee JK, et al. A systematic review of economic studies on biological agents used to treat Crohn's disease. Inflamm Bowel Dis 2013;19(12):2673-94. DOI: 10.1097/MIB.0b013e3182916046. [ Links ]
23. Fiorino G, Danese S. The biosimilar road in inflammatory bowel disease: the right way? Best Pract Res Clin Gastroenterol 2014;28(3):465-71. DOI: 10.1016/j.bpg.2014.04.006. [ Links ]
24. Argüelles-Arias F, Barreiro-de-Acosta M, Carballo F, et al. Joint position statement by "Sociedad Española de Patología Digestiva" (Spanish Society of Gastroenterology) and "Sociedad Española de Farmacología" (Spanish Society of Pharmacology) on biosimilar therapy for inflammatory bowel disease. Rev Esp Enferm Dig 2013;105(1):37-43. DOI: 10.4321/S1130-01082013000100006. [ Links ]
![]() Correspondence:
Correspondence:
Correspondence:
Manuel Barreiro-de Acosta.
Inflammatory Bowel Disease Unit. Department of Digestive Diseases.
Hospital Clínico Universitario de Santiago.
Travesía de Choupana, s/n.
15706 Santiago de Compostela, A Coruña. Spain
e-mail: manubarreiro@hotmail.com
Received: 29-04-2016
Accepted: 22-05-2016











 texto en
texto en