My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 n.10 Madrid Oct. 2016
https://dx.doi.org/10.17235/reed.2016.3908/2015
CASE REPORTS
Primary esophageal melanoma: report of a case
Melanoma esofágico primario: descripción de un caso
Laura Granel-Villach1, María Amparo Moya-Sanz1, Vicente Javier Escrig-Sos1, Carlos Fortea-Sanchís2, Carmen Martínez-Lahuerta3, Nuria Tornador-Gaya4 and José Luis Salvador-Sanchís1
1 Department of General and Digestive Surgery. Hospital General de Castellón.
2 Department of General and Digestive Surgery. Hospital Provincial de Castellón.
3 Department of Anatomy, Pathology and Histology. Hospital General de Castellón.
4 Department of Internal Medicine. Consulta de Alta Resolución. Hospital General de Castellón. Castellón, Spain
ABSTRACT
Introduction: Primary malignant melanoma of the esophagus is a rare tumor representing only 0.1-0.2% of esophageal malignancies. The goal of the study was to report on the management of a new case diagnosed and treated in our site.
Case report: A 67-year-old patient presented with dysphagia to solids with no other remarkable history or associated skin lesions. He underwent gastroscopy, which revealed a polypoid mass suggestive of neoplasm in the distal third of the esophagus. Biopsy indicated melanoma with positive immunohistochemical markers S100 and HMB45, and negative cytokeratins and CEA. Computerized tomography (CT) and positron-emission tomography (PET) scans showed no local infiltration or distant metastases. An Ivor-Lewis esophagectomy procedure was performed with regional lymphadenectomy. Postoperative stay lasted for three weeks, and no remarkable postsurgical complications arose. The pathological study of the specimen confirmed the diagnosis of primary esophageal melanoma.
Discussion: Primary malignant melanoma of the esophagus has an unfortunate prognosis as it is an aggressive tumor usually diagnosed at an advanced stage, with local invasion and metastatic disease. Currently, surgery is the treatment of choice, with the remaining adjuvant therapies obtaining limited results.
Key words: Primary melanoma of esophagus. Metastasis. Treatment.
RESUMEN
Introducción: el melanoma esofágico primario es un tumor muy poco frecuente que constituye únicamente el 0,1-0,2% de las enfermedades malignas del esófago. El objetivo del estudio fue presentar el manejo de un nuevo caso clínico diagnosticado y tratado en nuestro centro.
Caso clínico: paciente de 67 años que presentaba clínica de disfagia a sólidos sin otros antecedentes ni lesiones cutáneas asociadas. Se le realizó una gastroscopia, apreciándose una formación polipoide en tercio distal esofágico sugestiva de neoplasia. La biopsia fue positiva para melanoma con marcadores inmunohistoquímicos S100 y HMB45 positivos; citoqueratinas y CEA negativos. La tomografía computarizada (TC) y la tomografía por emisión de positrones (PET) no mostraron infiltración local ni metástasis a distancia. Se practicó una esofaguectomía de Ivor-Lewis con linfadenectomía regional. La estancia postoperatoria fue de tres semanas sin producirse complicaciones postoperatorias reseñables. El estudio anatomopatológico de la pieza confirmó el diagnóstico de melanoma esofágico primario.
Discusión: el pronóstico del melanoma primario de esófago es infausto, debido a que se trata de un tumor agresivo que suele diagnosticarse en fases avanzadas de la enfermedad, con presencia de invasión local y metástasis. El tratamiento de elección actualmente es la cirugía, obteniéndose resultados limitados con el resto de terapias adyuvantes.
Palabras clave: Melanoma primario de esófago. Metástasis. Tratamiento.
Case Report
A 67-year-old patient presents with clinical dysphagia, predominantly to solids, for the past two months, with no associated vomiting or constitutional syndrome. His history is remarkable for psoriasis, smoking, and alcohol abuse. No adenopathies could be palpated in accessible regions, his abdomen was soft, non-tender, and depressible, and no masses or organomegalies could be identified. No malignancy-suggestive skin lesions were seen.
As a part of the study a gastroscopy was performed, which revealed a pigmented, villous, ulcerated, pediculated polypoid lesion in the distal esophagus, which was friable to the touch and did not block the esophageal lumen. Biopsy samples were taken, which were consistent with squamous-cell melanoma positive for immunohistochemical markers S100 and HMB45, and negative for carcinoembryonic antigen (CEA) and cytokeratins.
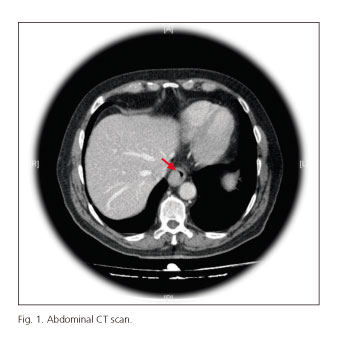
The extension study was completed with a chest-abdominal CT scan, which revealed an endoluminal esophageal growth compatible with neoplasm at the distal third of the esophagus, in the absence of either local infiltration or distant metastases evidence (Fig. 1).
A TEP scan was ordered, which showed hypermetabolism at the distal third of the esophagus and no metastatic uptake suggestive of tumor infiltration. A diagnosis of primary esophageal melanoma was then reached by exclusion.
Surgical management included Ivor-Lewis subtotal esophagogastrectomy with regional, celiac and mediastinal lymphadenectomy, posterior mediastinal gastroplasty, and anastomosis at the azygos arch level, in addition to feeding jejunostomy.
Postoperative stay lasted for three weeks, and the patient had a favorable course with no complications, normal diet being tolerated at discharge.
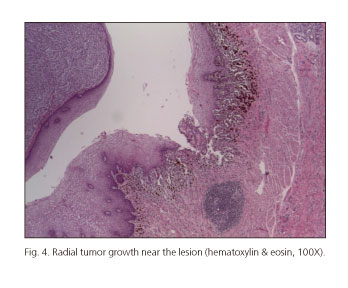
Gross pathology of the surgical specimen showed a pigmented polypoid, focally ulcerated lesion with radial growth, 4.3 x 2.4 x 2 cm in size, at the distal third of the esophagus (Fig. 2). Under the microscope the lesion was made up with squamous and fusiform neoplastic cells, some of them containing melanin pigment, with marked nuclear atypia and mitotic activity (Fig. 3). Radial growth foci were identified near the polypoid lesion (Fig. 4). Tumor infiltration reached the submucosal layer. Proximal, distal and circumferential margins remained tumor-free. Of all 20 dissected nodes, only one had melanoma micrometastasis.
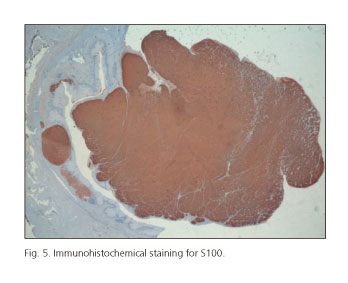
Tumor cells were positive for S100, Melan-A and HMB45, with immunohistochemical staining (Fig. 5). Staining was negative for cytokeratin, AE1/AE3 and CEA.
These pathological findings supported a definitive diagnosis with stage IIA (T2N0M0) primary malignant melanoma of the esophagus.
Discussion
Primary malignant melanoma of the esophagus is a rare condition (1,2). Diagnosis remained uncertain until benign melanocytes were found in the esophageal mucosa in 4 of 100 autopsies by Pava et al. (3). Later, Ohashi (4) and colleagues acknowledged this observation by showing the presence of melanocytes in the esophageal mucosa of 8% of the population.
Risk factors for this disease remain unclear, although it is more common in males between the sixth and seventh decades of life. Our patient meets these requirements without further risk factors, as alcohol and smoking seem to be unrelated, and DiConstanzo found them to be negative in a series of six primary esophageal melanomas recorded through 35 years (5).
Clinical presentation is similar to that of any esophageal malignancy, with dysphagia in 73% of patients, weight loss in 72%, retrosternal pain in 44%, and upper GI bleeding in only 10% (6). Our patient presented for dysphagia to solids of two-month standing with no other associated manifestations.
Upper GI endoscopy reveals an intraluminal polypoid lesion, either non-pigmented or brownish drab in color in 85% of patients, with an occasionally ulcerated or intact mucosa. The most common site (86%) includes the middle and distal thirds of the esophagus (7). Cases with multiple lesions have been described in association with skin melanoma metastases to the esophagus, which must be differentiated from the satellite lesions developing in up to 12% of patients. Our patient had no satellite lesions on endoscopy, only a single polypoid mass.
As with other sites, esophageal melanoma is also highly aggressive because of its tendency to grow vertically within the wall, both at the mucosal and submucosal level, with invasion of both lymph and blood vessels, which results in a high rate of metastatic disease at diagnosis. The first organ to become involved is the liver, followed by the mediastinum, lung, and brain (8). In our patient neither CT nor PET/CT scans demonstrated nodal or distant metastasis at the time of diagnosis.
Management is dependent upon the presence of distant metastasis and patient status. Surgery is the treatment of choice. Specifically for some authors (9) total esophagectomy plus lymphadenectomy should be the initial option since satellite lesions are often overlooked by preoperative diagnosis. As no such lesions were identified in our case, esophagectomy to the upper third was deemed as sufficient, with lesser gastric curvature (from the angular notch) and fundus resection, and extended lymphadenectomy in the mediastinum, paracardial region, lesser gastric curvature, and celiac trunk and its three main branches. Pathology demonstrated infiltration-free margins on the specimen with no satellite lesions and a total of twenty isolated nodes.
Radiotherapy, chemotherapy and immunotherapy have been used with limited results for primary esophageal melanoma (10). None has been shown to improve prognosis. Intraluminal radiotherapy is now showing promising results. A case was recently reported of a patient treated with heavy ion radiation who achieved a complete response. However, lung and liver metastases were identified at month 5 of follow-up, requiring chemotherapy (11).
Prognosis is usually fatal with a 5-year survival rate of 4.2 to 37% according to the various series reported. Survival improves with early diagnosis (12).
The pathological diagnosis of primary malignant melanoma of the esophagus relies on the identification of an in-situ component and/or radial growth in the proximity of the invading melanoma, according to the criteria established by Allen and Spitz in 1952, later implemented for esophageal melanoma by Raven and Dawson (13).
Some authors have described the observed mixed squamous and fusiform growth pattern for primary esophageal melanoma in contrast to metastatic melanoma (14). This criterion may seemingly be useful for the differential diagnosis of primary melanoma. However, given the sparse number of reported cases and the need for thorough lesion sampling in order to identify such mixed pattern, we believe this finding cannot be considered as a valid criterion for the histological diagnosis of primary esophageal melanoma.
Immunohistochemical techniques are useful for the differential diagnosis between melanoma and carcinoma, with antigen HMB-45, protein S-100, and Melan-A being particularly relevant in association with negative cytokeratins and CEA. However, no immunohistochemical marker is available to help differentiate primary from metastatic melanoma. This renders the exclusion of prior or concomitant skin lesions a key factor for initial diagnosis.
Regarding tumor staging, there is no consensus on the system to be used. In our case we followed the 2010 TNM, seventh edition, and categorized the condition as T2N0M0. Presently some authors only classify these tumors as T3-T4. According to this, our patient would be categorized as T3 (15).
To conclude, we may assert that esophageal melanoma is a rare tumor with a poor outcome. Early diagnosis is a key for prognosis, and differential diagnosis from secondary melanoma is required. Surgery is the treatment providing the best outcome as of today.
References
1. Rimsky Álvarez U, Ricardo Funke A, Felipe Solís H, et al. Melanoma primario de esófago. Rev Chilena de Cirugía 2009;61:168-70. [ Links ]
2. Sanchez AA, Wu TT, Prieto VG, et al. Comparison of primary and metastatic malignant melanoma of the esophagus: Clinicpathologic review of 10 cases. Arch Pathol Lab Med 2008;132:1623-9. [ Links ]
3. De la Pava S, Nigogosyan G, Pickren JW, et al. Melanosis of the esophagus. Cancer 1963;16:48-50. DOI: 10.1002/1097-0142(196301)16:1<48::AID-CNCR2820160107>3.0.CO;2-M. [ Links ]
4. Ohashi K, Kato Y, Kanno J, et al. Melanocytes and melanosis of the oesophagus in Japanese subjects - Analysis of factors effecting their increase. Virchows Arch A Pathol Anat Histopathol 1990;417:137-43. DOI: 10.1007/BF02190531. [ Links ]
5. DiCostanzo DP, Urmacher C. Primary malignant melanoma of the esophagus. Am J Surg Pathol 1987;11:46-52. DOI: 10.1097/00000478-198701000-00006. [ Links ]
6. Bisceglia M, Perri F, Tucci A, et al. Primary malignant melanoma of the esophagus: A clinicopathologic study of a case with comprehensive literature review. Adv Anat Pathol 2011;18:235-52. DOI: 10.1097/PAP.0b013e318216b99b. [ Links ]
7. Volpin E, Sauvanet A, Couvelard A, et al. Primary malignant melanoma of the esophagus: A case report and review of the literature. Dis Esophagus 2002;15:244-9. DOI: 10.1046/j.1442-2050.2002.00237.x. [ Links ]
8. Matsutani T, Onda M, Miyashita M, et al. Primary malignant melanoma of the esophagus treated by esophagectomy and systemic chemotherapy. Dis Esophagus 2001;14:241-4. DOI: 10.1046/j.1442-2050.2001.00193.x. [ Links ]
9. De Perrot M, Bründler Ma, Robert J, et al. Primary malignant melanoma of the esophagus. Dis Esophagus 2000;13:172-4. DOI: 10.1046/j.1442-2050.2000.00108.x. [ Links ]
10. Khek H, Jun C, Aileen W, et al. Primary malignant melanoma of the esophagus with multiple esophageal lesions. Nat Clin Pract Gastroenterol Hepatol 2007;4:171-4. DOI: 10.1038/ncpgasthep0761. [ Links ]
11. Naomato Y, Perdomo JA, Kamikawa Y. Primary malignant melanoma of the esophagus: Report of a case successfully treated with pre and postoperative adjuvant hormono-chemotherapy. Jpn J Clin Oncol 1998;28:758-61. DOI: 10.1093/jjco/28.12.758. [ Links ]
12. Lee SA, Hwang JJ, Choi YH, et al. Surgical treatment of primary malignant melanoma of the esophagus: A case report. J Korean Med Sci 2007;22:149-52. DOI: 10.3346/jkms.2007.22.1.149. [ Links ]
13. Boni L, Benevento A, Dionigi G, et al. Primary malignant melanoma of the esophagus: A case report. Surg Endosc 2002;16:359-60. DOI: 10.1007/s00464-001-4223-9. [ Links ]
14. Allen AC, Spitz S. Malignant melanoma. A clinicopathological analysis of the criteria for diagnosis and prognosis. Cancer 1953;6:1-45 DOI: 10.1002/1097-0142(195301)6:1<1::AID-CNCR2820060102>3.0.CO;2-C. [ Links ]
15. Raven RW, Dawson A. Malignant melanoma of the esophagus. Br J Surg 1964;51:551-5. DOI: 10.1002/bjs.1800510723. [ Links ]
![]() Correspondence:
Correspondence:
Laura Granel-Villach.
Department of General and Digestive Surgery.
Hospital General de Castellón.
Avda. Benicássim, s/n.
12004 Castellón, Spain.
e-mail: laura_9487@yahoo.es
Received: 01-07-2016
Accepted: 21-07-2016











 text in
text in