My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 n.11 Madrid Nov. 2016
PICTURES IN DIGESTIVE PATHOLOGY
Ulcerated submucosal gastric tumor. Could it be a benign condition?
Tumoración gástrica submucosa ulcerada. ¿Puede ser algo benigno?
Enrique Rodríguez-de-Santiago1, Celia Zaera-de-la-Fuente1, Beatriz Peñas-García1,3, Ana María Gutiérrez-Pecharromán2, José Luis Cuño-Roldán1, Carlos Arocena-Aranguren1, Víctor Defarges-Pons1, Lara Aguilera-Castro1, Daniel Boixeda-de-Miquel1,3 and Agustín Albillos-Martínez1,3
Departments of 1Gastroenterology and Hepatology, and 2Pathology. Hospital Universitario Ramón y Cajal. Madrid, Spain.
3Universidad de Alcalá. IRICYS. Madrid, Spain
Case Report
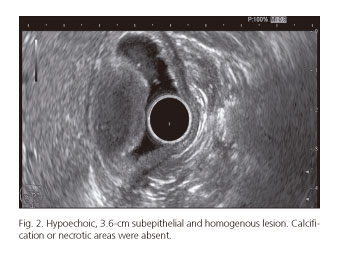
A 68-year-old female patient with an unremarkable past medical history presented to our Gastroenterology Department with a one month history of symptomatic anemia (hemoglobin: 4.5 g/dL) and intermittent episodes of melena without hemodynamic compromise. Esophagogastroduodenoscopy found an ulcerated mass of probable submucosal origin located in the prepiloric region (Fig. 1). Biopsies were compatible with granulation tissue. A subsequent endoscopic ultrasound (EUS) identified a 3.6-cm subepithelial, hypoechoic and homogenous lesion; calcification or necrotic areas were absent (Fig. 2). A CT scan revealed no distant disease (Fig. 3). The suspected diagnosis was a gastrointestinal stromal tumor (GIST); antrectomy with Roux-en-Y reconstruction was performed. Pathologic examination revealed an antral submucosal highly vascularized tumor constituted by a solid proliferation of spindle cells without atypia and eosinophil-predominant inflammation (Fig. 4A). Immunohistochemical staining exhibited strong positivity for vimentin and CD34, mild for actin and patchy for CD-117 and bcl-2, consistent with the diagnosis of an inflammatory fibroid polyp (IFP) (Fig. 4B). The postoperative period was uneventful and the patient is currently asymptomatic.
Discussion
First described in 1949 (1), IFP has also been named eosinophilic granuloma, inflammatory pseudotumor or Vanek's polyp. It is a rare benign submucosal tumor that can appear anywhere in the digestive tract, including the cecal appendix (2). It may be asymptomatic or present with gastrointestinal bleeding, iron deficiency anemia, dyspepsia or intussusception (3). The differential diagnosis includes carcinoids, GISTs, lipomas, leiomyomas, gastric adenocarcinomas, adenomas, neurofibromas, schwannomas and eosinophilic gastroenteritis. They are usually semi-pedunculated and covered with normal mucosa, but when the size exceeds one centimeter they can ulcerate and become indistinguishable from malignant tumors (4). EUS commonly shows an ill-defined, hypoechoic, homogeneous lesion which originates from the 2nd or 3rd layer of the gastric wall (5). Histopathological examination with immunohistochemistry is required for a definitive diagnosis. The classical treatment is surgery; however, endoscopic resection may be curative. Prognosis is excellent.
References
1. Vanek J. Gastric submucosal granuloma with eosinophilic infiltration. Am J Pathol 1949;25:397-411. [ Links ]
2. Liu TC, Lin MT, Montgomery EA, et al. Inflammatory fibroid polyps of the gastrointestinal tract: Spectrum of clinical, morphologic, and immunohistochemistry features. Am J Surg Pathol 2013;37:586-92. DOI: 10.1097/PAS.0b013e31827ae11e. [ Links ]
3. Matsushita M, Hajiro K, Okazaki K, et al. Endoscopic features of gastric inflammatory fibroid polyps. Am J Gastroenterol 1996;91:1595-8. [ Links ]
4. Matsushita M, Hajiro K, Okazaki K, et al. Gastric inflammatory fibroid polyps: Endoscopic ultrasonographic analysis in comparison with the histology. Gastrointest Endosc 1997;46:53-7. DOI: 10.1016/S0016-5107(97)70210-4. [ Links ]
5. Tada S, Iida M, Yao T, et al. Endoscopic removal of inflammatory fibroid polyps of the stomach. Am J Gastroenterol 1991;86:1247-50. [ Links ]











 text in
text in