Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Española de Enfermedades Digestivas
versão impressa ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 no.11 Madrid Nov. 2016
PICTURES IN DIGESTIVE PATHOLOGY
Endoscopic management of late complication of blunt traumatic total pancreatic transection
João Santos-Antunes, Pedro Moutinho-Ribeiro and Guilherme Macedo
Department of Gastroenterology. Faculty of Medicine. Centro Hospitalar S. João. Porto, Portugal
Case Report
An 11-year-old girl was admitted elsewhere due to severe abdominal pain after a fall with abdominal blunt trauma. CT-scan showed total pancreatic transection of the distal body with suspected injury of main pancreatic duct (Fig. 1). Conservative approach with antibiotics and total parenteral nutrition was decided due to her clinical stability. On day 12, she deteriorated clinically; ultrasound showed an 8 cm pseudocyst that was percutaneously drained. Initially she improved, but on day 37 she developed alimentary intolerance, and on day 55 she was referred to us with septic shock, to perform endoscopic drainage, under piperacillin/tazobactam.
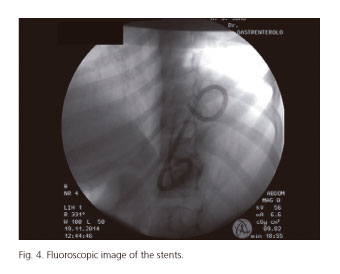
During endoscopic ultrasound, a 5 cm anechoic lesion (Fig. 2) was found in the distal pancreatic body. Transgastric puncture was performed and, over a guide-wire, the fistula was created with a cystotome, followed by balloon dilation (Fig. 3). Two 7 Fr double pigtail stents were placed (Fig. 4). Fluid and blood cultures were positive for Pseudomonas aeruginosa, and amikacin was added.
She had a favourable evolution, starting oral feeding 5 days later, and was discharged asymptomatic after two weeks. Six months later, MRI showed no signs of pancreatic lesion.
Discussion
Immediate management of blunt traumatic pancreatic transection is controversial, since the literature is based on case reports or series. Previous reports showed good outcomes with endoscopic, surgical treatment and even with conservative management in clinically stable patients (1,2).
Management of late complications are even rarely described (3). Clinical deterioration with septic shock demanded undoubtedly an aggressive treatment, with cystogastrostomy, percutaneous drainage or laparotomy. In our case, a minimally invasive approach was decided, with an excellent outcome.
References
1. Iqbal CW, St Peter SD, Tsao K, et al. Operative vs nonoperative management for blunt pancreatic transection in children: Multi-institutional outcomes. J Am Coll Surg 2014;218:157-62. DOI: 10.1016/j.jamcollsurg.2013.10.012. [ Links ]
2. Hamidian Jahromi A, D'Agostino HR, Zibari GB, et al. Surgical versus nonsurgical management of traumatic major pancreatic duct transection: Institutional experience and review of the literature. Pancreas 2013;42:76-87. DOI: 10.1097/MPA.0b013e3182575cf9. [ Links ]
3. Wales PW, Shuckett B, Kim PC. Long-term outcome after nonoperative management of complete traumatic pancreatic transection in children. J Pediatr Surg 2001;36:823-7. DOI: 10.1053/jpsu.2001.22970. [ Links ]