My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 n.12 Madrid Dec. 2016
https://dx.doi.org/10.17235/reed.2016.4060/2015
The role of surgical gastrostomy in the age of endoscopic gastrostomy: a 13 years and 543 patients retrospective study
Gabriel Oliveira1, Carla Adriana Santos2 and Jorge Fonseca2,3
1Department of Surgery. Hospital Garcia de Orta. Almada, Portugal.
2GENE - Enteral Feeding Team. Hospital Garcia de Orta. Almada, Portugal.
3CiiEM - Centro de Investigação Interdisciplinar Egas Moniz. Caparica, Portugal
ABSTRACT
Background: Percutaneous endoscopic gastrostomy (PEG) became the gold standard for enteral feeding. Currently, surgical gastrostomy is seldom used.
Objective: Evaluating the role of surgical gastrostomy in a center with a large experience in PEG.
Methods: A retrospective study ranged 13 years, collecting from clinical records: age, gender, underlying disease, date of procedure, technique, primary surgery, complications, 30-day mortality. Patients were divided according to indication for gastrostomy: a) neurological; b) head and neck cancer; c) other diseases; and d) drainage. PEG, open surgical and laparoscopic gastrostomies were compared concerning evolution of the number of procedures, characteristics of patients, complications and mortality.
Results: We identified 509 PEG, 26 open and 8 laparoscopic surgical gastrostomies. An increasing number of the percutaneous approach over the years was observed, while the number of surgical gastrostomies remains steady (mean: 2.6/year). All percutaneous endoscopic gastrostomies but three were feeding procedures, mostly in neurological patients. All laparoscopic gastrostomies were feeding procedures in head and neck cancer. Most open surgical gastrostomies were secondary procedures, part of more complex surgeries, and frequently for drainage purposes. The open surgical approach displayed more morbidity and mortality, reflecting the severity of underlying diseases.
Conclusions: In our institution, open surgical gastrostomy is seldom used, and mostly as part of complex procedures, frequently for drainage purposes. PEG is the choice to most dysphagic patients needing an enteral feeding access. When not feasible, laparoscopic gastrostomy is a suitable alternative.
Key words: Gastrostomy. Surgical gastrostomy. Laparoscopic gastrostomy. PEG.
Introducción
Enteral nutrition through tube feeding is the recommended nutritional support method for patients whose oral intake is insufficient to match their nutritional needs but whom, in spite of this, still have an efficient digestive tract, able to digest and absorb nutrients. Tube feeding during short periods is suitably achieved using a nasogastric tube. For enteral feeding during periods longer than three to four weeks, gastrostomy is the correct choice and has proven to be a successful procedure in patients unable to swallow (1). Furthermore, gastrostomy may also be used for drainage/decompressive purposes for patients with subocclusive disorders. Since Gauderer, in 1980, described the endoscopic approach to establish a gastrostomy (3), PEG became the gold standard for long enteral feeding (4,5) and surgical gastrostomy (SG) declined, only to be used occasionally. Endoscopic gastrostomy brought several advantages. Not only did it eliminate the need for an operating room, but also yielded a reduction in complications, operative time, and costs (5,6). However, endoscopic gastrostomy is not always feasible, most commonly when endoscopy cannot be performed in advanced head and neck cancer causing obstruction, or if diaphanoscopy of the stomach is not achieved. In those cases, gastrostomy must be accomplished using another method. Radiologically oriented gastrostomy is safe and useful (7,8), but most radiology teams do not have a large experience in this approach. Conversely, surgical teams of most large hospitals have some experience in performing surgical gastrostomies either as a single procedure or as part of a more complex surgical procedure. In the recent years, laparoscopic gastrostomy (LG) became more popular (2,9) as an alternative for open surgical gastrostomy (OSG).
There is a clear awareness that, as endoscopy units perform more and more PEG procedures, the number of SG performed drops. To the best of our knowledge, there is only a recent large study on SG, and it is from a center were the availability of PEG procedure is unreliable (10). In the endoscopic gastrostomy era there are no systematic studies evaluating the role of SG in any center with large experience in endoscopic gastrostomy.
The aim of the present study was the retrospective evaluation of the usefulness of surgical gastrostomy in a tertiary center with a large experience in PEG procedures.
Methods
A retrospective study was performed ranging an interval of 13 years (from January 2000 to December 2012). SGs were identified using the procedure codes ICD-9 (43.19 - Other gastrostomy), and PEG through clinical files from the Enteral Feeding Team. Using digital and paper clinical records, we collected the following data: age, gender, primary diagnosis, underlying disease, date of procedure, technique used, primary surgery (in cases where gastrostomy was an adjuvant procedure), complications and 30-day mortality rate. We excluded patients under 18 years and with incomplete or misclassified files. Patients were distributed in four groups according to the underlying disorder: a) neurological dysphagia; b) head and neck cancer (HNC); c) other diseases requiring feeding gastrostomy; and d) drainage/decompressive gastrostomy.
The three gastrostomy procedures, PEG, OSG and LG, were compared concerning the evolution of the number of procedures over time, demographic and clinical characteristics of patients, complications and 30-day mortality. Statistical analysis was accomplished with PASW Statistics 18. Fisher's exact test was applied to categorical variables, and Student's t-test was used to compare means. Results are considered significant at a 5% significance level.
Results
We identified 543 patients submitted to gastrostomy: 509 PEG and 34 SG. These 34 SG include 26 OSG and 8 LG. The distribution of the procedure over the study period is showed in figure 1. Data show a progressive increase of PEG procedures and a steady number of SG from 0 to 4 every year, with an average of 2.6 per year. Laparoscopic gastrostomy was introduced in 2006 but the regular use of LG did not completely eliminate the use of OSG.
The 509 PEG were performed on 163 females and 346 males, with ages ranging from 18 to 96, mean 63 ± 15.7. Only 3 (0.6%) were drainage procedures; the remaining 506 were feeding gastrostomies. From those, 265 (52%) PEGs were performed on patients with neurological dysphagia, 190 (37.3%) were performed on HNC patients, and 51 (10%) as feeding gastrostomies in other clinical settings.
Among the 34 SG, eight were excluded from further analysis due to incomplete records. The remaining 26 were 21 males and five females, ages ranging from 18 to 96 years, with a mean 59.6 ± 14.8. Neither gender nor ages were statistically different from PEG patients (p values 0.199 and 0.238, respectively).
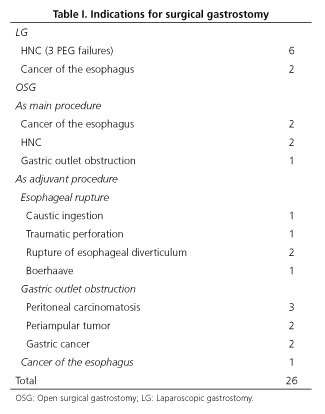
Among the 26 evaluated patients submitted to SG, eight were laparoscopically assisted surgical gastrostomy, while 18 underwent OSG. All of the eight LG were performed for feeding purposes on male patients with HNC. All of them had been previously proposed for PEG with failure of the procedure. The 18 patients that underwent OSG included 13 males and five females. Only in five OSG was the main surgical procedure, including four feeding procedures: two patients with HNC and two patients with esophageal cancer (lower third). These surgical procedures were previous to the introduction of LG. One patient underwent OSG as a drainage procedure for gastric carcinoma. In 13 patients, it was a secondary procedure in which feeding was the gastrostomy aim in only six. In the remaining seven patients, the gastrostomy was a secondary drainage procedure (Table I). In the eight patients with drainage gastrostomies, feeding was achieved through jejunostomy in six and total parenteral nutrition in two.
Analyzing SG distribution according to the four defined groups (underlying disorder or purpose of gastrostomy), surgical approach was predominantly used for feeding purposes in HNC patients and drainage in other more complex situations. No neurological patients needed surgical gastrostomy (Fig. 2).
Complication rate and mortality during the first 30 days after the procedure was different among procedures. No morbidity or 30-day mortality was identified following LG.
Of the patients submitted to PEG, three suffered dislocation of the tube into the peritoneum with peritonitis due to leakage of gastric contents. All of them underwent emergence surgery, and one patient died as a consequence of this complication. The other two patients underwent surgical gastropexy and the tube was successful placed. Seven other patients suffered dislocation of the tube into the abdominal wall creating "buried bumper syndrome", all of which were solved with endoscopic replacement of the PEG tube. Although 30-day mortality for PEG was 13.4% (68 patients), most patients died from the underlying disease and only one died as a consequence of a complication of the PEG technique.
Complications occurred in five patients submitted to OSG (27.8%) consisting of two cases of dehiscence (11.1%) and three with peristomal infection (16.7%). Although 30-day mortality for PEG was 13.4% (68 patients) and 33.3% for OSG (six patients), the difference was not statistically significant (p = 0.154).
Discussion
The introduction of PEG as the preferred method for enteral access to feed a dysphagic patient is well established since the early nineties. Stiegmann et al. (11) demonstrated then that not only PEG was economically superior to SG, but that morbidity and mortality were also equivalent. Later, it has become clear that PEG has, in fact, lower complication rate than SG, as demonstrated in a prospective randomized trial by Ljundhal et al. (6). As experience with the method grew and it became more available, PEG extended the indications for gastrostomy to a greater number of patients, meeting an increasing demand (12,13). In this new clinical paradigm, the role for SG remained up for debate. The authors were able to document the applications of this procedure in a tertiary center, observing in which situations SG is still performed. A progressive increase of PEG procedures was notorious, while the number of SG remained low over the years, and mostly executed within more complex procedures.
Before the introduction of LG, surgical gastrostomies were performed in two different clinical settings: as isolated feeding procedures or as a complementary procedure in other, more complex, surgeries. After 2006, LG became the surgical choice for feeding purposes in patients unsuitable for PEG, and OSG was only performed as an adjuvant procedure part of complex situations.
As expected, HNC represented 50% of the patients submitted to SG (against 38% from PEG). LG was used in HNC dysphagic patients when PEG was impossible, however our data suggest that PEG has been able to solve most of the HNC patients' needs for gastrostomy and feeding LG was used only after PEG attempt failure. Conversely, neurological dysphagia, the most frequent clinical indication for PEG in our hospital, seldom causes any technical problem that precludes the endoscopic approach. In patients with proximal esophageal cancer the endoscopic approach can be challenging, although in the authors' institution PEG was successfully performed in 22 out of 27 patients with this condition, in selected patients unsuitable to esophageal stenting (14). Nevertheless, SG (especially LG) may be the best option for patients without achievable endoscopy.
Although the 27.8% complication rate for OSG seems higher than the 12.1% for PEG, they were not statistically different (p = 0.069). This lack of statistical significance may be due to the small number of OSG. In fact, the larger percentage of complications in OSG seems to uncover the more severe nature of the underlying disorders of OSG patients. Thirty-day mortality was 33.3% after OSG, contrasting with the 13.4% after PEG. This may also reflect the complexity and precarious state of the patients submitted to major surgical procedures that included OSG. The peristomal infection rate for OSG was 16.7%, similar to the previous infection rate reported for our PEG-patients stoma infection (15). No peristomal infections were recorded in any of the eight patients undergoing LG.
In contrast with a recent study from Anselmo et al. (10), which reported that OSG was performed solely with feeding purposes, in our population, OSG was preserved for more complex situations in which gastrostomy was a secondary procedure, frequently for drainage purposes, when nutritional support was provided either by jejunostomy or total parenteral nutrition.
Endoscopic percutaneous is, and should be, first line approach in establishing an enteral feeding access. Nevertheless, there are situations in which safe performance cannot be achieved, either by technical difficulties (lack of diaphanoscopy) or by disease progression (obstruction preventing endoscope passage), which warrant an alternative. Other methods were described, attempting to reduce the shortcomings of PEG. For instance, several studies proposed a combination of PEG with laparoscopy (laparoscopic assisted PEG) to obviate such conundrums (16,17). In our study, we observed that in these situations, the preferred method was LG. In fact, our experience with LG seems to demonstrate that it is a safe and useful option, second only because of costs and longer in-hospital stay.
A recent study by Lucendo and Ruiz (13) reiterates that PEG is the desirable method for feeding patients unable to swallow but who maintain a functioning digestive tract. Concordantly, in our experience, in a large hospital with wide range of neurological and HNC patients needing gastrostomy, most of the patients will have a PEG procedure, which is cheaper and faster and, for the moment, fairly safe. But a small percentage of patients will always be unsuitable for PEG and, although more time consuming and more expensive, laparoscopic gastrostomy proved to be a safe and effective option.
Conclusions
In our institution, SG accounts for only 6% of all gastrostomies. Recently, OSG is used mainly as part of more complex surgical procedures and frequently as a drainage procedure, and not as an isolated feeding procedure. In these cases, feeding is achieved either by jejunostomy or total parenteral nutrition. With over 500 procedures in adults in a 13 year interval, PEG is, in our institution, the preferred method to achieve enteral feeding in patients unable to swallow, even in palliative esophageal cancer patients. When PEG is not feasible, laparoscopic gastrostomy is the main option for feeding purposes. As far as we may anticipate, while the endoscopic approach is available, these clinical indications will carry on unwavering through the era of endoscopic gastrostomy.
References
1. Loser C, Aschl G, Hebuterne EMH, et al. ESPEN guidelines artificial enteral nutrition - Percutaneous endoscopic gastrostomy (PEG). Clin Nutr 2005;24:848-61. DOI: 10.1016/j.clnu.2005.06.013. [ Links ]
2. Paski C, Dominitz JA. Endoscopic solutions to challenging enteral feeding problems. Curr Opin Gastroenterol 2012;28:427-31. DOI 10.1097/MOG.0b013e328355ecc9. [ Links ]
3. Ponsky JL, Gauderer MW. Percutaneous endoscopic gastrostomy: Indications, limitations, techniques, and results. World J Surg 1989;13:165-70. DOI: 10.1007/BF01658394. [ Links ]
4. Moller P, Lindberg G-G, Zilling T. Gastrostomy by various techniques: Evaluation of indications, outcome, and complications. Scand J Gastroentrol 1999;34:1050-4. [ Links ]
5. Rahnemai-Azar AA. Percutaneous endoscopic gastrostomy: Indications, technique, complications and management. World Journal of Gastroenterology 2014;20(24):7739. DOI: 10.3748/wjg.v20.i24.7739. [ Links ]
6. Ljungdahl M, Sundbom M. Complication rate lower after percutaneous endoscopic gastrostomy than after surgical gastrostomy: A prospective, randomized trial. Surg Endosc 2006;20:1248-51. DOI: 10.1007/s00464-005-0757-6. [ Links ]
7. Cosentini EP, Sautner T, Gnant M, et al. Outcomes of surgical, percutaneous endoscopic, and percutaneous radiologic gastrostomies. Arch Surg 1998;133:1076-83. DOI: 10.1001/archsurg.133.10.1076. [ Links ]
8. Covarrubias DA, O'Connor OJ, McDermott S, et al. Radiologic percutaneous gastrostomy: Review of potential complications and approach to managing the unexpected outcome. AJR Am J Roentgenol 2013;200:921-31. DOI: 10.2214/AJR.11.7804. [ Links ]
9. Edelman DS. Laparoendoscopic approaches to enteral access. Semin Laparosc Surg 2001;8:195-201. DOI: 10.1053/slas.2001.25578. [ Links ]
10. Anselmo CB, Tercioti Junior V, Lopes LR, et al. Surgical gastrostomy: Current indications and complications in a university hospital. Revista do Colégio Brasileiro de Cirurgiões 2013;40:458-62. DOI: 10.1590/S0100-69912013000600007. [ Links ]
11. Stiegmann GV, Goff JS, Silas D, et al. Endoscopic versus operative gastrostomy: Final results of a prospective randomized trial. Gastrointest Endosc 1990;36:1-5. DOI: 10.1016/S0016-5107(90)70911-X. [ Links ]
12. Pomerantz MA, Salomon J, Dunn R. Permanent gastrostomy as a solution to some nutritional problems in the elderly. J Am Geriatr Soc 1980;28:104-7. DOI: 10.1111/j.1532-5415.1980.tb00241.x. [ Links ]
13. Lucendo AJ, Friginal-Ruiz AB. Percutaneous endoscopic gastrostomy: An update on its indications, management, complications, and care. Rev Esp Enferm Dig 2014;106(8):529-39. [ Links ]
14. Grilo A, Santos CA, Fonseca J. Percutaneous endoscopic gastrostomy for nutritional palliation of upper esophageal cancer unsuitable for esophageal stenting. Arq Gastroenterol 2012;49:227-31. DOI: 10.1590/S0004-28032012000300012. [ Links ]
15. Duarte H, Santos C, Capelas ML, et al. Peristomal infection after percutaneous endoscopic gastrostomy: A 7-year surveillance of 297 patients. Arq Gastroenterol 2012;49:255-8. DOI: 10.1590/S0004-28032012000400005. [ Links ]
16. Shimizu Y, Okuyama H, Sasaki T, et al. Laparoscopic-assisted percutaneous endoscopic gastrostomy: A simple and efficient technique for disabled elderly patients. JPEN J Parenter Enteral Nutr 2014; 38(4):475-80. DOI: 10.1177/0148607113481476. [ Links ]
17. Hermanowicz A. Laparoscopy-assisted percutaneous endoscopic gastrostomy enables enteral nutrition even in patients with distorted anatomy. World Journal of Gastroenterology 2013;19(43):7696. DOI: 10.3748/wjg.v19.i43.7696. [ Links ]
![]() Correspondence:
Correspondence:
Gabriel Paiva de Oliveira.
Department of Surgery.
Serviço de Cirurgia, piso 4.
Hospital Garcia de Orta.
Av. Torrado da Silva. 2801-951
Almada, Portugal
e-mail: gp.oliveira@outlook.com
Received: 20-10-2015
Accepted: 01-09-2016