Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 no.12 Madrid dic. 2016
https://dx.doi.org/10.17235/reed.2016.4038/2015
Colonic leishmaniasis in a patient with HIV: a case report
Leishmaniasis con afectación colónica en paciente VIH: a propósito de un caso
Estela Soria-López1, Julián Olalla-Sierra2, Alfonso del-Arco-Jiménez2, Teresa Pereda-Salguero3, Cristina Abitei3 and Javier de-la-Torre-Lima2
Servicios de 1Digestivo, 2Medicina Interna y 3Anatomía Patológica. Hospital Costa del Sol, Marbella. Málaga
ABSTRACT
Background: To describe an unusual clinical presentation of visceral leishmaniasis affecting the colon.
Case report: We report the case of an HIV-positive patient with visceral leishmaniasis. We describe the clinical case, the procedures performed, the treatment provided and the patient's evolution. A comparative table of previously reported similar cases is shown.
Discussion: Visceral leishmaniasis with intestinal involvement is an uncommon process. Nevertheless, this possibility should be taken into consideration in the differential diagnosis of immunosuppressed patients with symptoms of diarrhea, as a favorable prognosis depends on early diagnosis and appropriate treatment.
Key words: Visceral leishmaniasis. Colonic involvement. HIV.
RESUMEN
Introducción: describir un cuadro poco habitual como es la leishmaniasis visceral con afectación colónica.
Caso clínico: presentamos el caso de un paciente VIH positivo con leishmaniasis visceral. Se describe el caso clínico, con los procedimientos realizados, el tratamiento y su evolución. Se adjunta tabla comparativa de los casos publicados de leishmaniasis con afectación de colon.
Discusión: la afectación intestinal en la leishmaniasis visceral es un proceso infrecuente, que debe incluirse en el diagnóstico diferencial en todo paciente inmunodeprimido con clínica de diarrea y que requiere un diagnóstico precoz y tratamiento adecuado, del que depende el pronóstico del paciente.
Palabras clave: Leishmaniasis visceral. Afectación colónica. VIH.
Introducción
Leishmaniasis is a disease of the mononuclear phagocyte system. It is caused by a parasite of the species Leishmania and transmitted through the bite of the Phlebotomus fly, which is endemic in several regions of the world, including the Mediterranean area. In Spain, the most common clinical form encountered is visceral leishmaniasis, which is usually associated with the clinical fever, pancytopaenia and hepatosplenomegaly triad (1).
According to previous reports, visceral leishmaniasis is more common in individuals presenting cellular immune deficiency. There is evidence that HIV infection is a risk factor associated with visceral leishmaniasis (2). In addition, HIV-Leishmania coinfection is an emerging disease.
Very few cases of colonic Leishmania have been described (Table I). We present the case of a patient with HIV and colitis due to Leishmania infection.
Case report
A male patient, aged 49 years, was admitted in October 2014 with abdominal pain and diarrhea. He had a clinical history of stage 3 HIV infection diagnosed in 2005, and chronic HCV infection with ultrasound findings of portal hypertension. He was a heavy smoker (continuing to the present) and had been consuming 100 g of alcohol daily until 2013. He was receiving antiretroviral treatment with abacavir-lamivudine-lopinavir-ritonavir (ABC + 3TC + LPV + RTV), but compliance was poor.
In the days prior to admission, the patient had abdominal cramping and 7-8 diarrheal movements per day, without pathological products, together with a recorded fever of up to 38 oC and general malaise.
Physical examination revealed poor general condition, and a large hyperpigmented lesion on the trunk, in the form of confluent plates, together with furuncle-type lesions with a white centre on both hands, hepatomegaly (6 cm), and moderate splenomegaly.
The only notable findings in the blood analysis were Hb 11.4 g/dl, 3,000/µl leukocytes, 92,000/µl platelets, GGT 119 U/l, FA 122 U/l and C-reactive protein 24.2 mg/L. Abdominal ultrasound examination revealed hepatosplenomegaly, hepatic steatosis and hepatic perihilar adenopathy.
In view of this clinical status, the patient was admitted to hospital, and treatment was started with serum, a strict diet and the reinitiation of antiretroviral treatment, with tenofovir-emtricitabine-raltegravir (TDF-FTC-RAL). A second blood test revealed CD4 44 cells/mm3 and HIV viral load 80,000 copies/mL without resistance to antiretrovirals. CMV viral load was negative. Stool culture was negative, and no fecal parasites were observed; the Clostridium difficile toxin test was negative. Blood and urine cultures were both negative. The patient developed acute renal failure by tenofovir, which was substituted by abacavir, with good results.
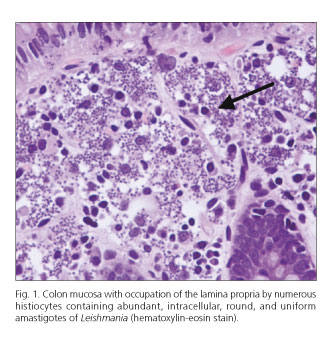
Thoracic-abdominal-pelvic CT revealed a homogeneous hepatosplenomegaly, with an 18 cm spleen, together with small adenopathies in the chest and abdomen. Bronchoscopy revealed diffuse inflammatory signs, mainly in the left bronchial tree; there were no tumor cells in the bronchial aspirate and the AFB (acid fast bacilli) smear was negative. Colonoscopy to the cecum revealed no lesions. Several random biopsies were taken from the ileum, the cecum, and the colon. The pathology analysis indicated ileal mucosa and of the large intestine with numerous intracellular microorganisms in the histiocyte cytoplasm, in the lamina propria, identified as corresponding to Leishmania, although no granulomas were observed (Fig. 1). Further biopsies were performed, of skin from the trunk and the back of the hands, and leishmaniasis was confirmed.
In view of these findings, consistent with visceral and cutaneous leishmaniasis, treatment was initiated with liposomal amphotericin B at a dose of 5 mg/kg/day for 5 days. The diarrheal symptoms and fever disappeared, and oral tolerance was good. During subsequent outpatient treatment to consolidate this recovery, a dose of 200 mg IV was given on days 10, 17, 24, 31 and 38, with good clinical and analytical response to date.
Discussion
Most cases of Leishmania in HIV-positive patients appear in advanced stages of the disease, presenting fewer than 200 CD4 cells/mm3 lymphocytes (3). Organomegaly, which is a common clinical manifestation in immunocompetent patients, is usually absent in HIV-positive persons. Cytopaenias are more common in immunocompromised patients, together with a higher rate of negative serology and increased disease relapse after treatment for Leishmania (3,4).
Atypical locations of visceral disease are more common in HIV patients, especially those with CD4 < 50 cells/mm3 and immunocompromised subjects (5). It can affect any part of the body, including gastrointestinal tract, peritoneum, lungs, pleural space or skin (2).
Leishmania can invade any part of the digestive tract, whether asymptomatically or manifested as esophageal symptoms, epigastric pain, diarrhea or rectal discomfort. It should be noted that these symptoms may also be caused by other coinfections such as CMV or Candida (1). In this respect, the duodenum is the digestive tract location that is most commonly reported (4). The colon is rarely affected; the cases published (most of which include the presence of diarrhea) are summarized in table I.
Intestinal involvement and the consequent malabsorption in visceral leishmaniasis infection are more common in coinfected patients. The precise mechanism by which this malabsorption takes place remains to be established but a multifactorial mechanism is known to be involved (6).
Endoscopic examination of these patients is usually prompted by epigastric pain and diarrhea. Results are irregular but usually nonspecific, with mild inflammatory alterations and atrophic mucosa. However, in over 50% of the cases considered there are no macroscopic alterations. This was the case in the present study, in which the biopsy analysis was necessary to confirm the diagnosis (4).
In conclusion, the possibility of infection by Leishmania should always be considered in immunosuppressed patients, particularly those who are HIV-positive and present symptoms of diarrhea, and especially if, in addition, they develop skin lesions and cytopaenia, as occurred in the case presented here. The pathologist should also take into account the potential presence of this parasite when examining a sample from the colon of an immunocompromised patient.
References
1. Alvar J, Cañabate C, Gutiérrez-Solar B, et al. Leishmania and human immunodeficiency virus coinfection: The first 10 years. Clin Microbiol Rev 1997;10:298-319. [ Links ]
2. Pintado V, Martín-Rabadán, Rivera ML, et al. Visceral leishmaniasis in human immunodeficiency virus (HIV)-infected and non-HIV infected patients. A comparative study. Medicine (Baltimore) 2001;80:54-73. DOI: 10.1097/00005792-200101000-00006. [ Links ]
3. Alvar J, Aparicio P, Aseffa A, et al. The relationship between leishmaniasis and AIDS: The second 10 years. Clin Microbiol Rev 2008;21:334. DOI: 10.1128/CMR.00061-07. [ Links ]
4. Jawhar NM. Visceral leishmaniasis with an unusual presentation in an HIV positive patient. Sultan Qaboos Univ Med J 2011;11:269-72. [ Links ]
5. Rosenthal E, Marty P, Del Giudice P, et al. HIV and Leishmania coinfection: A review of 91 cases with focus on atypical locations of leishmania. Clin Infec Dis 2000;31:1093-5. DOI: 10.1086/318135. [ Links ]
6. Baba CS, Makharia GK, Mathur P, et al. Chronic diarrhea and malabsorption caused by Leishmania donovani. Indian J Gastroenterol 2006;25:309-10. [ Links ]
7. Vargas AM, Belchí E, Martínez A, et al. Diarrhea due to visceral leishmaniasis in a liver transplant recipient. Gastroenterol Hepatol 2013;36:271-3. [ Links ]
8. Jimeno A, Morales E, Peñalver E, et al. Leishmaniasis visceral diagnosticada a partir de una biopsia colónica. Enferm Infecc Microbiol Clin 2012;30:353-54. DOI: 10.1016/j.eimc.2012.01.017. [ Links ]
9. Araujo SA, Nascentes TC, Demas MM. Colonic leishmaniasis followed by liver transplantation. Am J Trop Med Hyg 2010;83:209. DOI: 10.4269/ajtmh.2010.09-0430. [ Links ]
10. Hicks L, Kant P, Tay PH, et al. Visceral leishmaniasis presenting with intestinal failure: A case report and literature review. Eur J Gastroenterol Hepatol 2009;21:117-22. DOI: 10.1097/MEG.0b013e32830e6fdb. [ Links ]
11. Marcas A, Pedrol E, Llargués E, et al. Colon involvement as a form of presentation of visceral leishmaniasis in an AIDS patient. Enferm Infecc Microbiol Clin 1999;17:102-3. [ Links ]
12. Sebastián JJ, García S, Soria MT, et al. Visceral leishmaniasis diagnosed by colonoscopy. J Clin Gastroenterol 1997;25:691-2. DOI: 10.1097/00004836-199712000-00029. [ Links ]
13. Lemaistre AI, Chapel F, Cié P, et al. Unusual vascular lesions in the course of a colonic leishmaniasis in an HIV positive patient. Ann Pathol 1997;17:200-2. [ Links ]
14. Diego J, Omar M, Jiménez-Alonso J, et al. Visceral leishmaniasis with small intestine and colon involvement in a patient with HIV infection. Enferm Infecc Microbiol Clin 1995;13:377-8. [ Links ]
15. Duval JL, Jaubert D, Poizot-Martin I, et al. Colonic leishmaniasis in AIDS. Ann Med Interne (París) 1994;145:198-9. [ Links ]
![]() Correspondence:
Correspondence:
Estela Soria-López.
Department of Gastroenterology.
Hospital Costa del Sol de Marbella.
Autovía A-7, km 187.
29603 Marbella, Málaga. Spain
e-mail: estelasoria89@gmail.com
Received: 13-10-2015
Accepted: 23-11-2015











 texto en
texto en