My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 n.1 Madrid Jan. 2017
https://dx.doi.org/10.17235/reed.2016.4202/2016
Mesenteric schwannoma: an unusual cause of abdominal mass
Alejandra Tepox-Padrón1, Marcos Rafael Ramírez-Márquez2, Juan Carlos Córdova-Ramón3, Juan Cosme-Labarthe4 and Diego Luis Carrillo-Pérez2
Departments of 1Gastroenterology, 2Internal Medicine, 3Pathology and 4Radiology. Instituto Nacional de Ciencias Médicas y Nutrición "Salvador Zubirán". Mexico City, Mexico
ABSTRACT
Schwannomas (or neurilemmomas) are slow-growing mesenchymal neoplasms of the peripheral nerve sheath that may arise at almost any anatomical site. Mesentery schwannoma is extremely rare, with less than ten previously described cases. We present the case of a 38-year-old woman with arterial hypertension and chronic kidney disease with an abdominal painless mass of two years duration and an inconclusive pre-operative clinical diagnosis; she was successfully treated by complete surgical resection of the mass. The aim of this report is to recognize the possibility of schwannomas in the differential diagnosis of abdominal slowly growing tumors.
Key words: Schwannoma. Neurilemmoma. Mesentery. Nerve sheath neoplasms. Magnetic resonance imaging.
Introduction
Schwannoma (or neurilemmoma) is usually a benign neurogenic tumor arising from the sheath of cranial, peripheral and autonomic nerves. Clinically, these tumors may present as a cranial neuropathy, an abdominal or soft tissue mass, an intracranial lesion, or as spinal cord compression (1).
They rarely develop in the mesentery but should nevertheless be considered in the differential diagnosis of slow-growing abdominal masses. The growth of these masses causes displacement and compression of the nerve of origin, resulting in clinical symptoms. Surgical excision is the treatment of choice (2,3).
We report a patient with a schwannoma arising in the mesenteric root, and in whom the pre-operative diagnosis was inconclusive; the final diagnosis was established by histopathological examination.
Case report
Clinical summary
A 38-year-old female with arterial hypertension and chronic kidney disease of uncertain etiology (KDIGO stage G3a A1) was admitted to our hospital due to an abdominal mass that had been noticeable for 2 years but with no associated clinical symptoms; she had no history of Von Recklinghausen's disease. Physical examination revealed a painless mass, approximately 10 cm in diameter in the upper middle abdomen. Magnetic resonance imaging (MRI) showed a well-encapsulated, heterogeneous, cystic, right flank mass measuring 7.5 x 9.2 cm on T2-weighted images. It showed septal formations and marginal solid portion enhancement on T1-weighted images. There was no evidence of invasion of adjacent organs (Fig. 1). The results of tumor markers and metanephrines were all normal. The patient underwent surgery to excise the tumor and a large encapsulated heterogeneous mass located in the root of mesentery was resected.
Pathological findings
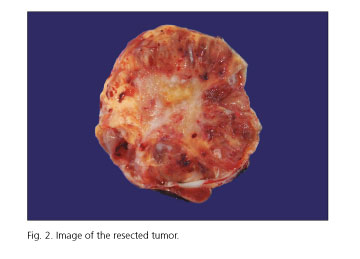
A well-encapsulated mass was completely removed. The tumor measured 11.3 x 8.4 x 4.1 cm, weighted 315 g and, on section, it had well-defined edges, an irregular surface with central fibrous and hemorrhagic areas and cystic portions containing brown liquid (Fig. 2).
Histological examination revealed a spindle cell tumor with abundant hyalinized vessels with a short beam pattern, sharp edges and cells with nuclei arranged en palisade (Verocay bodies) (Fig. 3A) as well as a biphasic pattern with hypercellular and hypocellular myxoid areas corresponding to Antoni A and Antoni B regions (Fig. 3B). On immunohistochemical examination, neoplastic cells were strongly positive for S-100 protein. The histopathological diagnosis of schwannoma was established. The patient was followed for two years and no disease recurrence was identified.
Discussion
Simon GC described the first case of mesenteric schwannoma in 1969 (3). As of 2015, less than ten cases have been reported in the English literature (2,5,6). It usually develops in young and middle-aged adults (median age 52 years) (2). Schwannomas are generally asymptomatic and discovered incidentally, although they may cause acute abdominal problems such as mechanical bowel obstruction as they progressively grow (7). In this case, the only clinical manifestation was a palpable abdominal mass.
On computed tomography (CT) scanning, schwannomas appear as well circumscribed, round-oval, homogeneous masses with CT densities ranging from near that of water to that of muscle. On contrast-enhanced CT scans, they appear as a heterogeneous mass. MRI findings reveal low-intensity images on T1-weighted imaging and high-intensity images on T2-weighted imaging, due to Antoni A and Antoni B areas and secondary degenerative changes. CT and MRI are useful to determine the size, location and extension of the tumor, but imaging features are nonspecific and lead to a difficult preoperative diagnosis (8,9).
The diagnostic gold standard is histopathological examination. The tumor consists of a compact cellular region (Antoni type-A tissue) and a hypocellular, myxoid region with a microcystic space (Antoni type-B tissue). En palisade nuclei (Verocay bodies) may be present in the Antoni-A area. Immunohistochemically, the tumor cells are positive for S100 protein. Enucleation is usually adequate surgical therapy for schwannoma and carries a good long-term prognosis; malignant transformation is exceedingly rare (10).
In summary, the clinical signs and symptoms of mesenteric schwannoma tend to be non-specific or even absent; they are difficult to diagnose with cross-sectional imaging and histopathological examination is required to reach a final diagnosis. This entity should be considered in the differential diagnosis of slow-growing abdominal masses.
References
1. Rosai J. Tumors and tumor like conditions of peripheral nerves. In: Rosai and Ackerman's Surgical Pathology. Edinburgh: Mosby; 2004:2263-75. [ Links ]
2. Yeh YH, Hsieh CB, Chan DC, et al. Mesenteric schwannoma: A case report and review of the literature. J Med Sci 2011;31:43-6. [ Links ]
3. Tang SX, Sun YH, Zhou XR, et al. Bowel mesentery (meso-appendix) microcystic/reticular schwannoma: Case report and literature review. World J Gastroenterol 2014;20:1371-6. DOI: 10.3748/wjg.v20.i5.1371. [ Links ]
4. Simon GC. Two cases of large benign schwannoma of the mesentery. Sem Hop 1969;45:2541-6. [ Links ]
5. Lao WT, Yang SH, Chen CL, et al. Mesentery neurilemmoma: CT, MRI and angiographic findings. Intern Med 2011;50:2579-81. DOI: 10.2169/internalmedicine.50.6198. [ Links ]
6. Burke KA, Amin MD, Álvarez LF, et al. Mesenteric neurilemmoma: A case study. Int J Surg 2013;11:566. DOI: 10.1016/j.ijsu.2013. 05.026. [ Links ]
7. Kilicoglu B, Kismet K, Gollu A, et al. Case report: Mesenteric schwannoma. Adv Ther 2006;23:696-700. DOI: 10.1007/BF02850308. [ Links ]
8. Kim SH, Choi BI, Han MC, et al. Retroperitoneal neurilemoma: CT and MR findings. AJR Am J Roentgenol 1992;159:1023-6. DOI: 10.2214/ajr.159.5.1414767. [ Links ]
9. Pilavaki M, Chourmouzi D, Kiziridou A, et al. Imaging of peripheral nerve sheath tumors with pathologic correlation: Pictorial review. Eur J Radiol 2004;52:229-39. DOI: 10.1016/j.ejrad.2003.12.001. [ Links ]
10. Murakami R, Tajima H, Kobayashi Y, et al. Mesenteric schwannoma. Eur Radiol 1998;8:277-9. DOI: 10.1007/s003300050379. [ Links ]
![]() Correspondence:
Correspondence:
Diego Luis Carrillo-Pérez.
Department of Internal Medicine.
Instituto Nacional de Ciencias Médicas y Nutrición "Salvador Zubirán".
Vasco de Quiroga, 15, Col. Sección XVI.
14080 Tlalpan, México D. F.
e-mail: djiego51@gmail.com
Received: 17-02-2016
Accepted: 20-02-2016