Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 no.7 Madrid jul. 2017
https://dx.doi.org/10.17235/reed.2017.4795/2016
ORIGINAL PAPERS
Endoscopically placed stents: a useful alternative for the management of refractory benign cervical esophageal stenosis
Óscar Nogales1, Ana Clemente1, Aránzazu Caballero-Marcos1, Javier García-Lledó1, Leticia Pérez-Carazo1, Beatriz Merino1, María López-Ibáñez1, M. Dolores Pérez-Valderas1, Rafael Bañares1,2,3 and Cecilia González-Asanza1
1Department of Gastroenterology. Hospital General Universitario Gregorio Marañón. Instituto de Investigación Sanitaria Gregorio Marañón. Madrid, Spain.
2CIBEREHD. Madrid, Spain.
3Faculty of Medicine. Universidad Complutense de Madrid. Madrid, Spain
ABSTRACT
Introduction: Benign esophageal strictures are relatively frequent and can severely affect the quality of life of a patient. Stenting has been proposed for the treatment of refractory cases. Lesions affecting the cervical esophagus are more difficult to treat, and the placement of stents in this location has traditionally been restricted due to potential adverse events. The aim of this study was to describe the efficacy and safety of endoscopic stenting in the management of refractory benign cervical esophageal strictures (RBCES) in a single-center cohort study.
Methods: We analyzed 12 patients with RBCES (Kochman's criteria) and severe dysphagia. We recorded previous endoscopic treatments, stricture characteristics and demographic data. The two types of stents used were fully covered self-expandable metallic stents (FCSEMS) and uncovered biodegradable stents (BDS). FCSEMS were removed eight weeks after placement, and BDS were followed-up until degradation. We assessed technical and clinical success, rate of stricture recurrence and adverse events.
Results: The mean age of participants was 64 years (range 30-85). A total of 23 stents (13 FCSEMS and 10 BDS) were placed in 12 patients (median 1.92, range 1-4). The technical success rate was 96% (22/23 stents). Eight patients (66.6%) maintained adequate oral intake at the end of follow-up (median 33.3 months, range 3-84 months). Migration was recorded in 7/23 stents (30.4%) and epithelial hyperplasia in 4/23 stents (17.4%). No severe adverse events were noted. All patients complained of minor cervical pain after placement that was well controlled with mild analgesia.
Conclusions: Endoscopic stent therapy seems to be effective and safe in the management of RBCES.
Key words: Esophageal stents. Benign esophageal strictures. Cervical esophagus.
Introduction
Benign esophageal strictures are associated with gastroesophageal reflux disease, caustic ingestion, esophageal surgery and radiotherapy (1). This condition can diminish quality of life due to severe dysphagia, malnutrition and weight loss. Additionally, patients have an increased risk of aspiration pneumonia. Endoscopic dilatation has traditionally been treated with bougies or balloons. However, up to 10-15% of benign esophageal strictures are refractory according to Kochman's criteria (4), thus indicating a lack of improvement after endoscopic dilatation (2,3). Although an algorithm for the management of these strictures has not been established, the use of esophageal stents has been proposed (5-9).
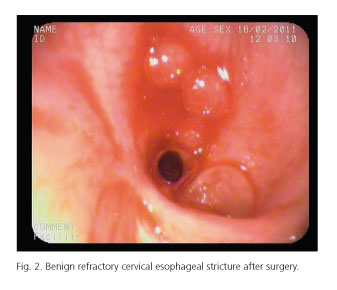
Lesions affecting the cervical esophagus are particularly difficult to treat due to their location. In fact, the placement of a stent in the cervical esophagus has traditionally been restricted because of the risk of potential adverse events such as tracheal compression, proximal migration, intractable pain and, most commonly, foreign body sensation (10,11). Nevertheless, some reports have suggested the possibility of treating this type of stricture by placing a stent in the cervical esophagus (12). Optimal management is unclear due to the fact that findings in the literature are heterogeneous and include both malignant and benign strictures, and the recommendation for radiological or endoscopic approaches differ between studies. Appropriate management is especially important in the case of benign stenosis, in which survival is longer and the impact of the stricture on the patient's quality of life may be more significant. The type of stent to be used in this context is also controversial.
The aim of this study was to describe the feasibility, efficacy and safety of endoscopic stenting in the management of refractory benign cervical esophageal strictures (RBCES).
Patients and methods
Patients
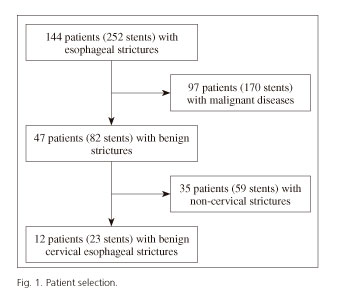
We performed a non-randomized, retrospective cohort study at a single, tertiary-care center. We searched our endoscopy database for all patients treated with stents in the last seven years and selected those where the stricture was the consequence of a benign process in the cervical esophagus (n = 12) (Fig. 1). The cervical location of the stricture was defined as between 15 and 19 cm from the incisors (Fig. 2).
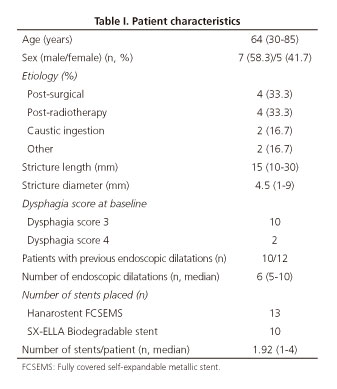
We assessed demographic data (sex, gender), the etiology and characteristics of the stricture, previous endoscopic treatments, severity of dysphagia before and after endoscopic treatment(s) (according to a previously defined dysphagia score [13]), type of stent, technical and clinical success and need for additional interventions (other endoscopic procedures or surgery).
Ten patients received through-the-scope (TTS) balloon dilatation prior to stent placement (median number of procedures: 6, range 5-10). The median maximum balloon diameter was 14 mm (range 12-16 mm). Wider diameters were achieved due to the severe fibrosis in most of cases and the risk of perforation. Two patients did not strictly fulfill Kochman's criteria as previous balloon dilatation was not performed. One patient had a long (3 cm), subacute (30 days after caustic ingestion) caustic injury with concomitant strictures in the middle and distal esophagus and was considered as a better candidate for stenting as a first option (patient # 6). The other patient had complete aphagia due to a long post-radiotherapy stricture, clearly suggesting that the initial treatment should be stent placement (patient # 9).
Stent type and placement
The two types of stent used were a fully-covered self-expandable metal stent (FCSEMS) (Hanarostent Esophagus Asymmetric and Hanarostent Colon/Rectum TTS, M.I. Tech, South Korea) with a diameter of 20 mm, and an uncovered biodegradable stent (BDS) (SX-ELLA, ELLA-CS, Czech Republic), with a diameter of 30 x 25 x 30 mm. The type of stent was chosen according to its availability at the time of the procedure.
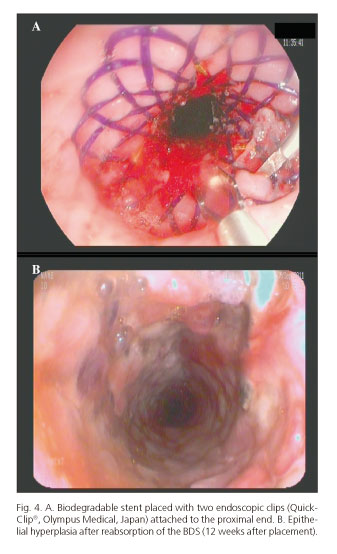
All endoscopic procedures were performed in the Endoscopy Unit of the Hospital General Universitario Gregorio Marañón, in Madrid (Spain), using deep sedation without orotracheal intubation. The endoscopist decided whether or not to use fluoroscopy depending on the individual characteristics of the patients. This was necessary in cases where the stricture was located in the first 3 cm distal to the upper esophageal sphincter, thus the gastroscope for control or stent deployment was placed above the upper esophageal sphincter to complete the procedure. All stents were placed over a guide wire that was advanced through the stricture using fluoroscopy or under direct visualization with a gastroscope (EVIS EXERA III video system and GIF-H190 gastroscope, Olympus Medical, Japan; and Pentax Medical EPK-1000 processor and EG-3490K Pentax gastroscope). Prior dilatation was only performed when the delivery system could not be passed through the stricture. Stents were placed at least 2 cm above the proximal end of the stenosis in an attempt to achieve minimal sensation of pain and decrease the risk of migration. Endoscopic clips (1-3 clips per stent; QuickClip2 Long, Olympus Medical, Japan) were placed at the proximal end of the stent to anchor it in place and prevent distal migration.
Patients were instructed to call the unit if clinically relevant events appeared during the follow-up period. No intermediate endoscopic procedures were scheduled, although endoscopic examinations were performed when dysphagia worsened during follow-up or when another significant symptom appeared.
According to usual clinical practice, FCSEMS were scheduled to be removed eight weeks after placement (Fig. 3). BDS-treated patients received endoscopic examinations every eight weeks until the stent was completely degraded or when another significant symptom appeared (Fig. 4).
Definitions
Placement was considered to be technically successful when the stent could be deployed in the correct pre-established location. According to the expected maximal expansion time, clinical success was pre-defined as the presence of a dysphagia score < 2 one week after the procedure.
Recurrence of dysphagia was defined as worsening of at least 1 point in the dysphagia score at any time during follow-up. Recurrence of dysphagia was treated by insertion of an additional stent and/or endoscopic balloon dilatation.
Significant epithelial hyperplasia was defined as worsening of the dysphagia score by at least 1 point.
Statistical analysis
Descriptive data are presented as mean, median (range), or percentage, as appropriate. The t test was used to compare continuous variables. Fisher's exact test was used to compare proportions. All analyses were performed using IBM SPSS Statistics for Windows, version 19.0 (IBM Corp., Armonk, New York, USA). Statistical significance was set at p < 0.05; all p values were two-tailed.
Results
Twelve patients with RBCES were treated with stents at our institution from February 2008 to January 2015. The median age was 64 years (range 30-85). Five patients were women (41.7%) and seven were men (58.3%). The etiology of the strictures is shown in table I.
The dysphagia score before endoscopic treatment was ≥ 3 in all patients. Median stricture length and diameter were 15 mm (range 10-30 mm) and 4.5 mm (range 1-9 mm), respectively. Two patients had at least another stricture in the medium or distal esophagus.
Treatment and outcome are summarized in table II. A total of 23 stents were placed in 12 patients (median stents per patient: 1.92, range 1-4). Thirteen of the stents were FCSEMS and ten were BDS. Twenty-two of the 23 stents were correctly deployed (technical success: 96%). Only one patient required the insertion of a second stent (during the same procedure) due to the misplacement of a BDS distal to the stricture. Three patients did not have an initial clinical response and received alternative therapy (two surgical interventions and one endoscopic gastrostomy with a pediatric endoscope). Four of the remaining patients had a complete response with resolution of dysphagia and did not require an additional intervention. In the remaining five patients (three with FCSEMS and two with BDS), dysphagia reappeared after stent removal or reabsorption and was successfully treated with additional stenting in four cases, plus additional TTS balloon dilatations (1-3 sessions per patient) in three cases. Therefore, 8/12 (66.6%) patients maintained an adequate oral intake at the end of follow-up (median: 33.3 months, range 3-84 months). Those patients who did not respond to stent therapy (4/12 patients) underwent percutaneous endoscopic gastrostomy with a pediatric endoscope (n = 2) or surgery (n = 2).
All patients complained of mild cervical pain after placement, although this was well controlled with non-steroidal anti-inflammatory drugs during the first 3-5 days, except for one patient who required early stent removal (third day post-placement) due to uncontrollable pain and foreign body sensation.
The stent migrated in seven of the 23 cases (30.4%). Interestingly, migration was observed in 7/13 FCSEMS (53.8%) but not in BDS (0%; p = 0.005) cases. All the migrated FCSEMS were successfully repositioned using endoscopy. In addition, significant epithelial hyperplasia was recorded in four of 23 stent cases (17.4%), all of which involved BDS. No hyperplasia was recorded in patients who received an FCSEMS (40% vs 0%; p = 0.01). Argon plasma coagulation plus TTS balloon dilatation was used as a rescue treatment in patients who developed hyperplasia, although the results were poor. No severe adverse events (including perforation, hemorrhage, pulmonary aspiration, death) were observed.
Discussion
Refractory benign esophageal cervical strictures represent a real clinical challenge as they usually require complex surgical procedures, the consequences of the condition are severe and few efficacious therapeutic alternatives are available. Although endoscopic alternatives for the management of this condition have been reported, the findings are heterogeneous and based on studies of both benign and malignant stenosis. Consequently, the results are not easily generalized. In this study, we show that endoscopic management of this complex condition based on sequential dilatation and stenting is both safe and effective. First, our approach was easily applied as shown by the fact that the scheduled procedure could be completed in all cases. This finding is consistent with previous reports showing similar success rates, suggesting that the endoscopic approach should probably be the first option for RBCES. Importantly, the current series included very severe cases, as indicated by the degree of dysphagia, which prevented solid oral intake in all cases. Second, our approach proved to be successful with two-thirds of patients able to resume normal oral intake in the long term. This finding is especially relevant as other series failed to show similar results in benign strictures, mainly owing to the heterogeneity of the findings, which also included malignant stenosis. In the study of malignant and benign cervical strictures by Choi et al. (14), 16 patients were treated, of whom only four had benign stenosis (three caustic injuries, one post-surgical) and were treated with FCSEMS (covered nitinol stents). Temporary stent placement was unable to achieve a long-lasting improvement in any of the four patients. Gallo et al. (15) performed a retrospective study of ten patients with benign strictures that were treated with three different stent types, and found a 100% clinical response rate. As in our study, additional dilatation sessions (1-3 sessions) were necessary to maintain oral intake in three cases.
We also showed the procedure to be safe. There were no severe adverse events and all the patients were discharged early from hospital. Of note, pain was recorded in all cases, although this was transient and easily controlled. In one case, the stent had to be removed due to intractable pain. Our approach required consecutive endoscopic interventions for various reasons, such as stent migration, epithelial hyperplasia and, more commonly, early recurrence of dysphagia after removal or reabsorption of the stent. It is noteworthy that a relatively high number of stents were required to maintain clinical efficacy. In fact, only four cases were successfully treated with a single stent. Consequently, intensive follow-up with an early and aggressive endoscopic approach is clearly recommended in the management of this condition.
Our study is not without limitations. Our series was retrospective and the endoscopic intervention was designed case by case. Therefore, we are unable to recommend a homogeneous approach for the management of RBCES. In fact, we used two types of stent that differ in their mechanical characteristics and natural history. No specific stent for the upper esophagus (asymmetrical design) was used (except in one case, patient # 1) due to a lack of availability at our institution. Colorectal stents used in our cohort had the advantage that they are TTS devices, easier to deploy compared to those that have to be placed in parallel. Although the small sample size precludes a definitive conclusion, it seems that both types of stent provided similar results. Not surprisingly, a greater incidence of epithelial hyperplasia was observed with the BDS, and the FCSEMS migrated more frequently. Nevertheless, further studies are required to confirm these promising results.
No additional fixation (except for endoscopic clips) was used to prevent migration, especially for FCSEMS (more prone to migration). Perhaps other fixation devices such as endoscopic suturing could reduce migration, but the cervical esophagus can be a cumbersome and is also a difficult location to perform these techniques due to technical problems (narrow working area). Moreover, the availability of these devices is low in endoscopy units and could increase the costs to the procedure.
In conclusion, endoscopic stent placement seems to be effective and safe in the management of refractory benign cervical esophageal strictures. However, consecutive endoscopic interventions are commonly required to maintain clinical efficacy.
References
1. De Wijkerslooth LR, Vleggaar FP, Siersema PD. Endoscopic management of difficult or recurrent esophageal strictures. Am J Gastroenterol 2011;106(12):2080-91;quiz2092. DOI: 10.1038/ajg.2011.348. [ Links ]
2. Didden P, Spaander MC, Bruno MJ, et al. Esophageal stents in malignant and benign disorders. Curr Gastroenterol Rep 2013;15(4):319. DOI: 10.1007/s11894-013-0319-3. [ Links ]
3. Raymondi R, Pereira-Lima JC, Valves A, et al. Endoscopic dilation of benign esophageal strictures without fluoroscopy: Experience of 2,750 procedures. Hepatogastroenterol 2008;55(85):1342-8. [ Links ]
4. Kochman ML, McClave SA, Boyce HW. The refractory and the recurrent esophageal stricture: A definition. Gastrointest Endosc 2005;62(3):474-5. DOI: 10.1016/j.gie.2005.04.050. [ Links ]
5. Repici A, Conio M, De Angelis C, et al. Temporary placement of an expandable polyester silicone-covered stent for treatment of refractory benign esophageal strictures. Gastrointest Endosc 2004;60(4):513-9. DOI: 10.1016/S0016-5107(04)01882-6. [ Links ]
6. Sharma P, Kozarek R, Practice Parameters Committee of American College of Gastroenterology. Role of esophageal stents in benign and malignant diseases. Am J Gastroenterol 2010;105(2):258-73;quiz274. DOI: 10.1038/ajg.2009.684. [ Links ]
7. Siersema PD. Treatment options for esophageal strictures. Nat Clin Pract Gastroenterol Hepatol 2008;5(3):142-52. DOI: 10.1038/ncpgasthep1053. [ Links ]
8. Wadhwa RP, Kozarek RA, France RE, et al. Use of self-expandable metallic stents in benign GI diseases. Gastrointest Endosc 2003;58(2):207-12. DOI: 10.1067/mge.2003.343. [ Links ]
9. Repici A, Vleggaar FP, Hassan C, et al. Efficacy and safety of biodegradable stents for refractory benign esophageal strictures: The BEST (Biodegradable Esophageal Stent) study. Gastrointest Endosc 2010;72(5):927-34. DOI: 10.1016/j.gie.2010.07.031. [ Links ]
10. Shim CS, Jung IS, Bhandari S, et al. Management of malignant strictures of the cervical esophagus with a newly-designed self-expanding metal stent. Endoscopy 2004;36(6):554-7. DOI: 10.1055/s-2004-814555. [ Links ]
11. Conio M, Caroli-Bosc F, Demarquay JF, et al. Self-expanding metal stents in the palliation of neoplasms of the cervical esophagus. Hepatogastroenterol 1999;46(25):272-7. [ Links ]
12. Profili S, Meloni GB, Feo CF, et al. Self-expandable metal stents in the management of cervical oesophageal and/or hypopharyngeal strictures. Clin Radiol 2002;57(11):1028-33. DOI: 10.1053/crad.2002.0988. [ Links ]
13. Gaspar LE, Winter K, Kocha WI, et al. Swallowing function and weight change observed in a phase I/II study of external-beam radiation, brachytherapy and concurrent chemotherapy in localized cancer of the esophagus (RTOG 9207). Cancer J 2001;7(5):388-94. [ Links ]
14. Choi EK, Song HY, Kim JW, et al. Covered metallic stent placement in the management of cervical esophageal strictures. J Vasc Interv Radiol 2007;18(7):888-95. DOI: 10.1016/j.jvir.2007.04.017. [ Links ]
15. Gallo A, Pagliuca G, De Vincentiis M, et al. Endoscopic treatment of benign and malignant strictures of the cervical esophagus and hypopharynx. Ann Otol Rhinol Laryngol 2012;121(2):104-9. DOI: 10.1177/000348941212100206. [ Links ]
![]() Correspondence:
Correspondence:
Óscar Nogales Rincón.
Department of Gastroenterology.
Hospital General Universitario Gregorio Marañón.
C/ Doctor Esquerdo, 46.
28007 Madrid, Spain
e-mail: oscar.nogales@salud.madrid.com
Received: 25-12-2016
Accepted: 13-03-2017