My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 n.8 Madrid Aug. 2017
https://dx.doi.org/10.17235/reed.2017.4605/2016
LETTERS TO THE EDITOR
Hepatic glycogenosis: a diagnostic challenge
Glucogenosis hepática diabética: un nuevo reto diagnóstico
Key words: Hepatic glycogenosis. Diabetes mellitus.
Palabras clave: Glucogenosis hepática. Diabetes mellitus. Glucogenosis hepatocitaria.
Dear Editor,
Recently, several cases of hepatic glycogenosis (HG) have been reported (1,2). García-Suárez et al. (1) described a young female patient with poorly controlled type 1 diabetes, right upper quadrant pain and elevated serum transaminases and GGT. After other causes of liver disease were excluded and a liver biopsy was performed, the patient was diagnosed with HG.
HG is rare and can be misdiagnosed as steatohepatitis. To date, less than 20 cases have been reported in adults.
Case report
A 39-year-old female was admitted with right hypochondriac pain. She had type I diabetes treated with insulin with a poor metabolic control (HbA1c 10.6%).
Physical examination showed hepatomegaly and short stature. Blood tests revealed AST 7,500 U/l and ALT 2,150 U/l. Abdominal ultrasound identified a "bright" liver without lesions or abnormal vessels. Magnetic resonance (MR) cholangiography showed a normal biliary tract without lithiasis and abdominal computed tomography (CT) showed hepatomegaly. The workup for hepatitis was negative.
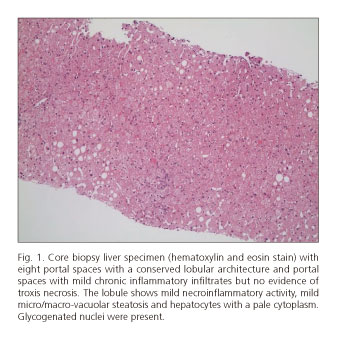
A liver biopsy was performed due to the suspicion of glycogenic liver disease. The histological study (Fig. 1) revealed minimal non-specific chronic inflammatory infiltrates in the portal tracts, mild micro/macro-vacuolar steatosis and hepatocytes with glycogenated nuclei without giant mitochondria. The findings were compatible with HG.
Optimizing insulin treatment resulted in clinical improvement and normalization of liver enzymes. Outpatient follow-up was unremarkable with a good glycemic control and normal liver enzyme levels.
Discussion
HG is rare in adults but should be suspected in patients with poorly controlled type 1 diabetes, right hypochondriac pain and elevated transaminases. Moreover, as seen in the case report by García-Suárez et al., GGT can also be elevated. Diagnosing HG requires a high clinical suspicion, with other causes of liver disease ruled out and a liver biopsy. The treatment and prognosis differ from non-alcoholic steatohepatitis. The treatment consists of optimizing the treatment of diabetes.
Diana Horta1, Maria-Rosa Escoda2 and Luigi Melcarne1
Departments of 1Digestive Diseases and 2Pathology. Parc Taulí Sabadell.
Hospital Universitari. Universidad Autónoma de Barcelona.
Sabadell, Barcelona. Spain
References
1. García-Suárez C, Álvarez B, Castro Ortiz E, et al. Hepatopatía glicogénica: una causa infrecuente y reversible de aumento de transaminasas en el paciente diabético. Caso clínico. Rev Esp Enferm Dig 2015;107(2):111-2. [ Links ]
2. Marco Silva, Margarida Marques, Hélder Cardoso, et al. Glycogenic hepatopathy in young adults: A case series. Rev Esp Enferm Dig 2016;108(10):673-6. DOI: 10.17235/reed.2016.3934/2015. [ Links ]
3. Giordano S, Martocchia A, Toussan L, et al. Diagnosis of hepatic glycogenosis in poorly controlled type 1 diabetes mellitus. World J Diabetes 2014;5(6):882-8. DOI: 10.4239/wjd.v5.i6.882. [ Links ]











 text in
text in