My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.110 n.1 Madrid Jan. 2018
https://dx.doi.org/10.17235/reed.2017.5092/2017
ORIGINAL PAPERS
Insertion of fully covered self-expanding metal stents in benign biliary diseases
1Servicio de Gastroenterología y Endoscopia. Hospital El Cruce Dr. Néstor Carlos Kirchner. Florencio Varela. Buenos Aires, Argentina
INTRODUCTION
Plastic biliary stents were first used in 1980 1 and the use of self-expanding metal stents began at the end of the same decade 2) (3. Initially, both types of stents were used to treat malignant biliopancreatic pathologies and were later used to treat benign ductal obstructions.
Benign biliary stenosis that mainly occurs post-surgery was the first non-tumor stenotic indication for the use of biliary stents, initially via the insertion of two or more plastic stents 4. At present, fully covered self-expanding metal stents (FCSEMS) are gaining acceptance for the treatment of these types of stenoses. Its greater expansion strength, radial diameter, permeability and the low number of procedures mean that the range of indications has increased 5) (6. In this article, we evaluate the effectiveness and the complications associated with the use of temporary endoscopic FCSEMS for the treatment of benign biliary pathologies. These are classified as obstructive and non-obstructive (Fig. 1).
MATERIALS AND METHODS
This was a retrospective and observational study using a prospective database. The study was conducted in a tertiary care center from March 2012 to May 2016. Patients with a FCSEMS inserted due to a benign biliary disease were included.
The indications, technical success rates (placement and extraction of stents), resolution rates and complications were recorded. The WallFlex Biliary Rx Fully Covered FCSEMS was used which was 10mm in diameter x 60mm in length (Boston Scientific).
Definitions
Surgical bile duct injury (SBDI): obstruction (ligation, clipping and cicatricial stenosis) or total or partial section of the main bile duct or the aberrant ducts that drain a hepatic segment.
Complex choledocholithiasis: multiple lithiasis (three or more, at least one of them larger than 20mm) and/or lithiasis larger than 20mm and/or lithiasis impacted in the bile duct.
Type II papillary stenosis: narrowing of the bile duct at a papillary level, without compromising the distal common bile duct up to a length of 10 mm (inflammatory origin).
Refractory or high grade biliary fistulas: continuity of the biliary tree that generates biliary discharge that occurs during ERCP, before the opacification of the intrahepatic biliary branches. These are refractory to the sphincterotomy or to the use of plastic stents.
Post sphincterotomy hemorrhage: papillary bleeding following sphincterotomy, refractory to the standard endoscopic treatment (injection, thermal methods and/or hemoclips).
Bile duct perforation: continuity in the bile duct wall in any area.
Post-transplant stenosis: reduction of the bile duct caliber after a liver transplant.
RESULTS
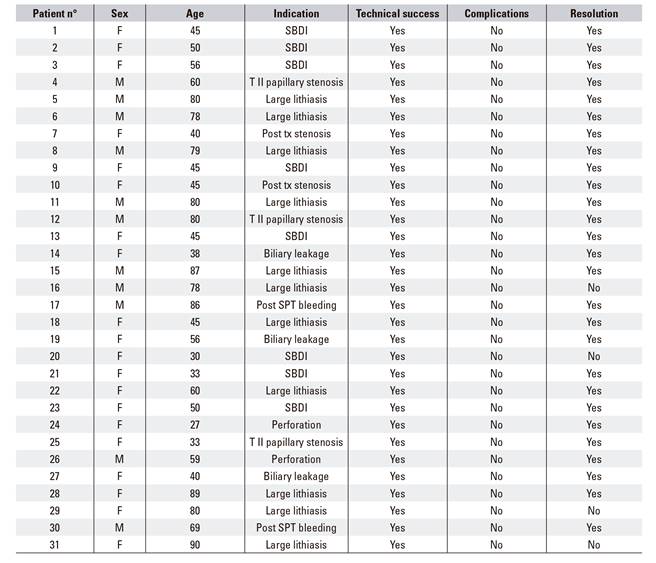
Thirty-one patients were included and the average age was 57 years old (27-90) and 66% were female (20) Thirty-four FCSEMS were inserted according to the following indications, 8 (25%) SBDI, 11 (31%) complex choledocholithiasis, 3 (8.3%) refractory or high grade biliary fistulas, 2 (6 %) post liver transplant stenoses, 3 (8.3%) type II papillary stenoses, 2 (6 %) iatrogenic biliary perforations and 2 (6%) post papillotomy refractory bleeds (Table 1). The insertion technical success rate was 100%. The resolution rate for the underlying pathology was 88%; 87.5% (7/8) in SBDI, 73% (8/11) in complex choledocholithiasis and 100% for the remaining indications. The average time from placement to extraction was 133 days (10-180 days) (Table 2). The use a second stent was necessary in 3 cases. There were 2 cases with SBDI and failure of the first treatment and 1 case of a resolved stenosis with the second stent and the other required surgical treatment. The third case was due to a post-transplant stenosis and was resolved with a second stent. The three patients with choledocholithiasis that did not respond to the FCSEMS were resolved via surgery.
Table 1 Indications for the insertion of fully covered self-expanding metal stents

SBDI: surgical bile duct injury.
Table 2 Average placement time of fully covered self-expanding metal stents

SBDI: surgical bile duct injury.
Thirty-three of 34 FCSEMS were endoscopically extracted with no technical complications. The other stent was extracted during the pancreacticoduodenectomy procedure from a patient with resectable pancreatic cancer. The indication for the use of a FCSEMS in this case was a post sphincterotomy bleed refractory to the endoscopic therapeutic. No complications were registered during stent placement, stent extraction or due to stent migration (Table 3).
DISCUSSION
FCSEMS seems to resolve the problem of prolonged biliary drainage for malignant biliary stenoses. Due to its greater permeability compared to plastic stents, this technique is currently the first option for the treatment of extra hepatic malignant biliary stenoses. Furthermore, the indications for these stents also include benign biliary pathologies. It is important to note that the resolution rate for benign biliary pathologies using FCSEMS was 88% in this study, similar to that reported in the literature.
Many authors have emphasized the importance of plastic biliary stents in the treatment of complex choledocholithiasis, post-surgical stenoses and biliary fistulas. The mechanism of action is to ensure biliary permeability, to apply friction in the case of complex choledocholithiasis, to maintain a continued and progressive dilation in stenoses and to reduce the transpapillary pressure gradient in fistulas. With regard to benign stenoses, the resolution rates via multiple endoscopic sessions using a plastic stent are variable, between 40 and 90% according to different series 4) (7. FCSEMS adds some special features that result in increased resolution rates of up to 91-92% 8) (9.
In the case of complex choledocholithiasis, the greater radial expansions compress and grind the stones which ultimately lead to breakage, softening and a reduction in size (Fig. 2). Recent studies have also demonstrated that FCSEMS are an effective and reliable option for cases of a failed conventional extraction of lithiasis 6) (10) (11) (12) (13) (14). In the context of stenoses, the FCSEMS creates a continued radial dilation that is equal to the action of three plastic stents, both at the papilla and the common bile duct from the initial ERCP (Fig. 3). The articles published in this area highlight a greater biliary clearance rate with a lower number of procedures. Thus, this technique is more cost-effective than the use of plastic stents 5) (8) (9. The study by Coté et al. 8 in 2016 is the only randomized and controlled study performed in this area. This study confirmed the hypothesis that metal stents are not inferior to plastic stents when used as an initial strategy and in fact resolve the stenosis in fewer sessions.
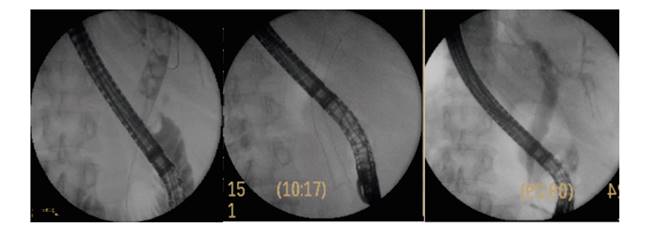
Fig. 2 Complex choledocholithiasis. Insertion of a fully covered self-expanding metal stent. ERCP following the extraction of the stent.

Fig. 3 Post laparoscopic cholecystetomy stenosis. Insertion of a fully covered self-expanding metal stent. Stenosis resolution.
The study of Wang et al. 15 in 2009 that included 13 cases, recommended the insertion of FCSEMS in complex biliary fistulas, defined as those that do not respond to the initial endoscopic treatment with sphyncterotomy and a plastic stent. The authors claim that the inserted stent can remain for up to sixteen months and there were no difficulties for the extraction. Our study showed a resolution of 100% without any migrations and the average placement time was one hundred days. In the 2 cases of post sphyncteroyomy papillary bleeding, a FCSEMS was used due to the failure of the standard hemostasis techniques (injection and thermal and mechanical methods). This was due to the benefits that these stents provide such as a radial force of compression and a greater drainage diameter of the bile duct. The case reported by García-Cano and collaborators 16 in 2016 of a post sphyncterotomy choledochal perforation responded to the insertion of a FCSEMS, which was withdrawn without difficulties two months later. As highlighted by the authors, bile duct perforations have excellent resolution rates when metal stents are used. The 2 cases reported here were resolved with the same treatment and no surgical intervention was required.
There were no significant complications during the placement and extraction of these stents. The percentage of reported distal migrations and papillary tissue hyperplasia without clinical consequences is low 5) (6. This situation did not arise during any of the thirty four procedures reported here. However, one limitation of the study is the limited sample size and the retrospective design.
CONCLUSION
The FCSEMS are highly effective for the resolution of benign biliary pathologies and can therefore be considered as a reliable and effective alternative in some cases. The validation of this technique for the treatment of a benign biliary pathology requires randomized and cost-effective studies.
BIBLIOGRAFÍA
1. Srinivasan I, Kahaleh M. Review Biliary stents in the millennium. Adv Ther 2011;28(11):960-72. DOI: 10.1007/s12325-011-0067-4 [ Links ]
2. Huibregtse K, Cheng J, Coene PP, et al. Endoscopic placement of expandable metal stents for biliary strictures--a preliminary report on experience with 33 patients. Endoscopy 1989;21(6):280-2. DOI: 10.1055/s-2007-1012969 [ Links ]
3. Irving JD, Adam A, Dick R, et al. Expandable metallic biliary stents: results of a European clinical trial. Radiology 1989;172(2):321-6. DOI: 10.1148/radiology.172.2.2664861 [ Links ]
4. Costamagna G, Pandolfi M, Multignani M, et al. Long term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents. Gastrointest Endosc 2001;54:162-8. DOI: 10.1067/mge.2001.116876 [ Links ]
5. García-Cano J, Taberna-Arana L, Jimeno-Ayllón C, et al. Use of fully covered self-expanding metal stents for the management of benign biliary conditions. Rev Esp Enferm Dig 2010;102:526-32. DOI: 10.4321/S1130-01082010000900003 [ Links ]
6. García-Cano J, Reyes-Guevara AK, Martínez-Pérez T, et al. Fully covered self-expanding metal stents in the management of difficult common bile duct stones. Rev Esp Enferm Dig 2013;105:7-12. DOI: 10.4321/S1130-01082013000100003 [ Links ]
7. Draganov P, Hoffman B, Marsh W, et al. Long-term outcome in patients with benign biliary strictures treated endoscopically with multiple stents. Gastrointest Endosc 2002;55(6):680-6. DOI: 10.1067/mge.2002.122955 [ Links ]
8. Coté GA, Slivka A, Tarnasky P, et al. Effect of Covered Metallic Stents Compared With Plastic Stents on Benign Biliary Stricture Resolution A Randomized Clinical Trial. JAMA 2016;315(12):1250-7. DOI: 10.1001/jama.2016.2619 [ Links ]
9. Jeng KS, Sheen IS, Yang FS. Are expandable metallic stents better than conventional methods for treating difficult intrahepatic biliary strictures with recurrent hepatolithiasis? Arch Surg 1999;134:267-73. [ Links ]
10. Mizukami Y, Saito H, Obara T. Temporary use of an accuflex stent for unextractable common bile duct stones. J Gastroenterol Hepatol 2000;15:680-3. DOI: 10.1046/j.1440-1746.2000.02200.x [ Links ]
11. Minami A, Fujita R. A new technique for removal of bile duct stones with an expandable metallic stent. Gastrointest Endosc 2003;57:945-8. DOI: 10.1016/S0016-5107(03)70050-9 [ Links ]
12. Cerefice M, Sauer B, Javaid M, et al. Complex biliary stones: treatment with removable self-expandable metal stents: a new approach. Gastrointest Endosc 2011;74:520-6. DOI: 10.1016/j.gie.2011.05.026 [ Links ]
13. Horiuchi A, Nakayama Y, Kajiyama M. Biliary stenting in the management of large or multiple common bile duct stones. Gastrointest Endosc 2010;71:1200-3. DOI: 10.1016/j.gie.2009.12.055 [ Links ]
14. Curvale C, Guidi M, Hwang H. Resolución de coledocolitiasis compleja con stent metálico removible. Reporte de un caso. Rev Gastroenterol Mex 2016;81(1):56-8. [ Links ]
15. Wang AY, Ellen K, Berg CL, et al. Metallic stents in the management of complex biliary leaks: preliminary data-a case series. Endoscopy 2009;41:781-6. DOI: 10.1055/s-0029-1215050 [ Links ]
16. García-Cano J, Ferri-Bataller R, Gómez-Ruiz CJ. Common bile duct perforation sealed with a metal fully-covered stent. Rev Esp Enferm Dig 2016;108(8):495-6. [ Links ]
Received: June 06, 2017; Accepted: August 16, 2017











 text in
text in