INTRODUCTION
Acute calculous cholecystitis (ACC) is an inflammatory process of the gallbladder and is one of the most common emergency admissions in surgical clinics 1,2,3,4. Laparoscopic cholecystectomy (LC), especially during the initial phase of development, is the gold standard treatment for ACC due to its safety and efficacy 1,2,5,6. However, early cholecystectomy could result in a morbidity up to 41% with a perioperative mortality of up to 18% in elderly patients with severe comorbidities 1,4.
Percutaneous cholecystostomy (PC) was introduced in the 1980s as a minimally invasive procedure that avoids general anesthesia for the decompression and drainage of gallbladders in patients with ACC 5,7. PC may offer a good solution for the relief of the inflammatory response in patients with a complicated cholecystectomy or high-risk patients with perioperative morbidity or mortality. It is a bridge to a subsequent surgery and a definitive treatment for patients who are unfit for surgery 1,3,7,8. Apart from some studies that focus on the timing of late cholecystectomy after PC, there are no reported data about the timing for removal of the PC tube 9.
Almost one third of patients with ACC treated with PC experienced a recurrence during a mean follow-up of 1.8 years. Gallstones were shown to be related with recurrent cholecystitis after PC tube removal. Therefore, early removal of the PC tube before surgical treatment may be an underlying factor for recurrence 10. In contrast, tube drainage in cholecystostomy cases longer than two weeks is an independent risk factor for early recurrence of late cholecystectomy during interval periods without the PC tube 11. A systematic review that focused on the duration of PC tube placement (ranging between two and 193 days) found evidence of how tube duration might affect outcome 12. In previous studies, the catheter was removed at the beginning of surgery, whereas in other studies the catheter was removed early during the interval period before cholecystectomy 1,2,7,10.
Removal of the PC tube in patients with normal clinical and imaging findings can be a feasible choice due to the risk of recurrent attacks of ACC, especially during the interval period for late cholecystectomy. However, the effect of leaving the PC tube in position until late cholecystectomy has not yet been studied. The purpose of this study was to evaluate the safety and efficacy of PC tube placement and to determine the optimal duration and removal time of the PC tube, either before or after delayed cholecystectomy in ACC patients.
PATIENTS AND METHODS
Patient and data collection
This was a retrospective analysis of a historical cohort study of adult patients (age ≥ 18 years) who underwent PC placement due to ACC between January 2014 and December 2015, using a prospectively held database. The study was performed according to the Declaration of Helsinki and was approved by the local institutional committee. Signed informed consent with regard to the application of PC tube was obtained from all patients. This study was registered in researchregistry.com; the ID number is 3657.
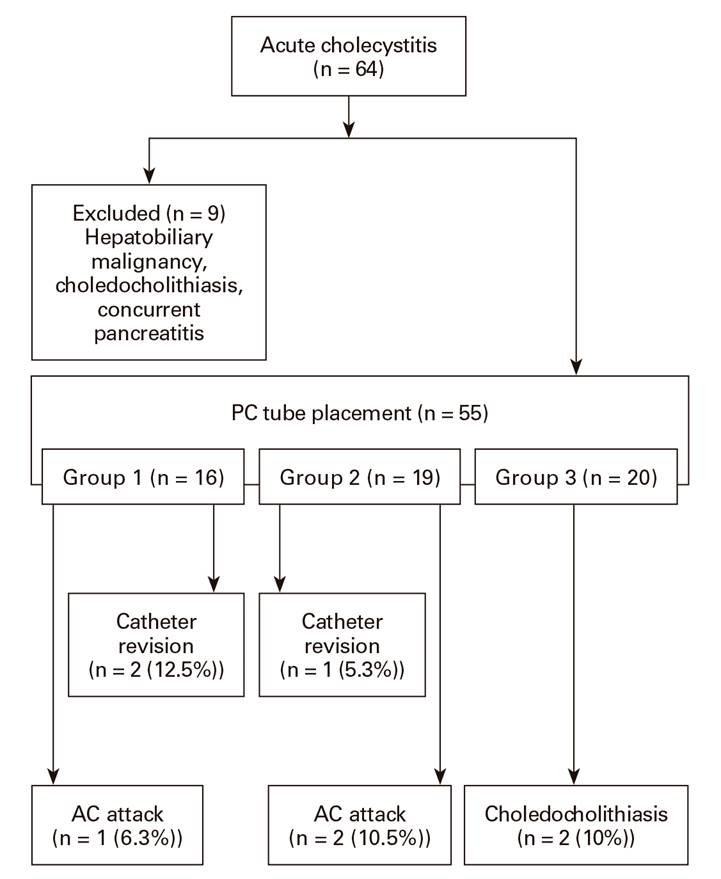
There were 64 patients that underwent PC due to ACC. Nine patients had hepatobiliary malignancy (n = 3), choledocholithiasis (n = 1) or concurrent pancreatitis (n = 5) when ACC was diagnosed. These subjects were excluded. Therefore, a total of 55 patients were finally included.
The diagnosis of ACC was based on clinical presentation, physical examination, laboratory data and imaging studies, including ultrasound and computed tomography according to the 2013 Tokyo Guidelines 13. Upon diagnosis of ACC, patients fasted and were given intravenous fluids and intravenous broad spectrum antibiotics. As per institutional policy, early LC was offered to all patients with ACC. However, patients with a higher American Anesthesiology Score (ASA) (≥ 3) were considered as exceptions for early surgery. The presence of co-morbidities indicated by an ASA score of 3 or more and unresponsiveness to the medical therapy within 48 hours that lasted more than 72 hours from symptom onset were accepted as indications for PC tube placement. The decision to perform PC based on these criteria was mainly at the discretion of the surgical team.
All patients were operated on after PC placement after an average interval period of 6-8 weeks. Patients were grouped according to their treatment modalities: surgical treatment was not recommended in patients over 70 years of age with severe concomitant diseases (ASA score ≥ 3) and patients who were unwilling to undergo surgery (group 1). PC was regarded as the definitive treatment in this group. Subsequent surgical treatment was performed in patients after the removal of the PC tube (group 2). It was left in situ, either with free drainage or clamped until removal at the beginning of the surgery (group 3) (Fig. 1).
Forty-eight hours of clamping was performed if there was clear bile drainage from the PC tube. In the absence of clinical symptoms (fever or right upper quadrant pain), the PC tube was clamped or removed. Decisions to remove the PC tube and the timing of PC tube removal were at the discretion of the attending surgeon. The drainage tube was removed in group 2 subjects when the patients showed no symptoms of recurrence, such as fever or right upper quadrant pain, after the PC tube had been clamped for at least 48 hours, or if a patent cystic duct was identified by cholangiography.
All data were collected using hospital and radiology information which included: age, gender, ASA score and comorbidities. Variables with regard to the treatment modalities included the following: time period between the diagnosis of ACC, PC tube placement and surgery; length of the PC tube; complications after the procedure (dislodgement and ejection of the tube, peri-tubal biliary leakage, bleeding and the need for reinsertion of another tube); surgical complications (conversion to an open surgery, intraoperative complications, bleeding, iatrogenic bile duct injury, surgical site infections, need for endoscopic cholangiopancreatography, mortality) and follow up notes. We specifically investigated the patients with and without a PC tube during the interval period for recurrence of biliary events or gallstone-related complications.
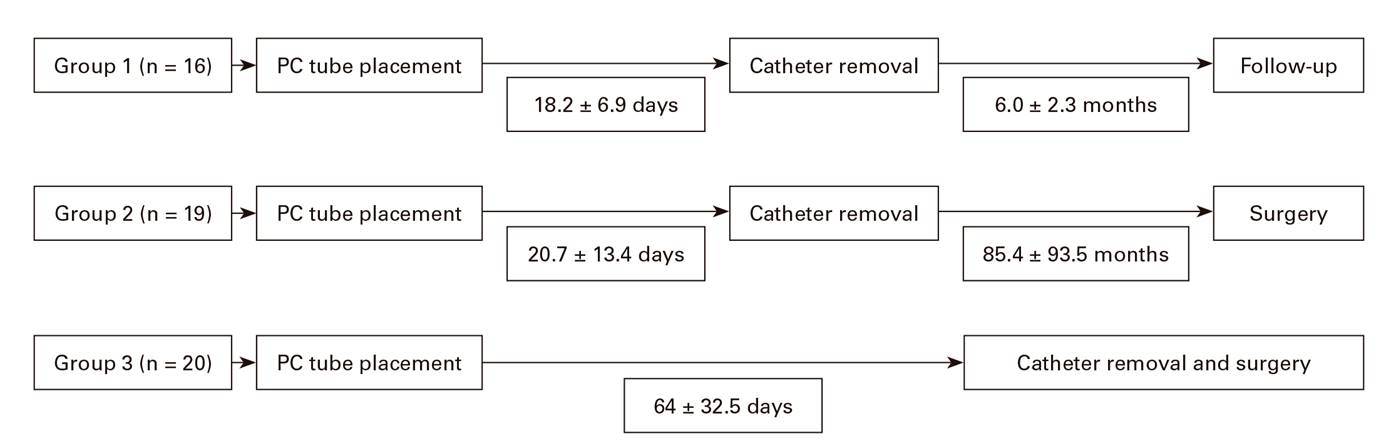
Group 1 was followed during December 2016 via direct interview or phone calls. Thus, the mean follow-up period after the removal of the catheter in this group was 6.0 ± 2.3 months. The patients in groups 2 and 3 were followed up to the end of postoperative one month.
PC placement
The procedure was performed by an experienced radiologist with the patient under local anesthesia. An 8 or 10 Fr pigtail catheter was inserted into the gallbladder through a transhepatic route under ultrasound guidance. After placement, the PC tube was left open with free drainage. Aspirated fluid, which was either bile or pus, was sent for culture analysis. Clinical improvement after PC tube placement was regarded as successful intervention.
Statistical analysis
The development of gallstone-related complications such as recurrent AC attacks, acute biliary pancreatitis, choledocholithiasis and acute cholangitis were the main outcomes. Recurrent AC attacks and acute cholangitis during this period were defined in accordance with the 2013 Tokyo Guidelines 13. Acute upper abdominal pain of a biliary origin associated with hyperamylasemia was defined as acute biliary pancreatitis. Elevated serum bilirubin levels due to common bile duct stones were confirmed by imaging or treated via endoscopic retrograde cholangiopancreatography. These were regarded as choledocholithiasis. All statistical analyses were performed using SPSS 15.0 for Windows (SPSS. Inc., Chicago, IL, USA). Normally-distributed continuous variables were expressed as mean ± standard deviation. Categorical variables were expressed as frequencies and percentages. Variables were compared via a one-way analysis of variance and the Kruskal-Wallis test. The statistical results were presented with 95% confidence intervals. Differences were considered as statistically significant if the p value was less than 0.05.
RESULTS
During the study period, there were 55 AC patients initially treated with PC. The study population consisted of 24 females (43.6%) and 31 males (56.4%) with a mean age of 64.8 ± 15.9 years. Group 1 included 16 patients (29.1%) that were treated conservatively. There were 19 patients (34.5%) in group 2 and 20 (36.4%) in group 3 that were treated surgically after PC tube placement. Demographic variables, ASA score and the distribution of co-morbidities are summarized in table 1. The groups were similar in terms of age, gender and ASA score distribution (p = 0.376, p = 0.984 and p = 0.690, respectively). The groups were also similar according to the presence of co-morbidities (p = 0.461). Hypertension and diabetes were the most common co-morbidities observed in 23 (41%) and 18 patients (32.7%), respectively (Table 1).
PC placement was technically successful in 57 of 59 interventions (96.6%). There were two cases (12.5%) of catheter revisions due to leakage that required a new PC tube placement in group 1 and one case (5.3%) in group 2. Catheter dislodgement was detected in one patient (5%) from group 3. In addition, two patients developed subcapsular biloma and pericholecystic abscesses. The rate of procedure-related complications was 9.1%; five complications in 55 patients (Table 2).
The catheter withdrawal time for group 1 and group 2 was 18.2 ± 6.9 and 20.7 ± 13.4 days, respectively. Surgical treatment was performed in group 2 after a mean of 85.4 ± 93.5 days. In group 3, surgical treatment was performed after a mean of 64 ± 32.5 days while the PC tube was in place (Fig. 2).
One ACC attack (6.3%) occurred in group 1 that required medical treatment during the follow up period of 6.0 ± 2.3 months. Two patients (10.5%) in group 2 had an ACC attack. Two group 3 patients (10%) had choledocholithiasis that required endoscopic retrograde cholangiopancreatography during the waiting period. Considering all groups, the rate of gallstone related complications was 9.1% (five events in 55 patients). There were one (5.3%) and two conversions (10%) to open surgery in group 2 and 3, respectively. Postoperative morbidity rates were 15.8% and 10.0% for group 2 and 3, respectively (p = 0.532) (Table 2). There was no mortality in study group 1.
DISCUSSION
PC is an alternative intervention for the treatment of high-risk patients with ACC as it reduces inflammation and decompresses the gallbladder. However, it is still not currently the standard treatment and its success and procedure-related complications have been questioned. Several groups have studied the indications, success and complications of PC tube insertion with varying numerical values. We did not aim to evaluate these issues but rather investigated the impact of the PC tube on the development of gallstone-related complications after the procedure or during the interval period.
The optimal duration of PC drainage is the main controversial issue. While there are no widely accepted recommendations, periods of three to six weeks with an average of one month are reported 1,9. With regard to tract maturation, ≥ 2 weeks are required after the trans-hepatic approach 1. Morse et al. 14 recommended that the PC tube should remain in place in critically ill patients until cholecystectomy. Although it is difficult to predict which patients have a high risk of recurrent AC after PC tube placement, Wang et al. 1 also suggested keeping the PC tube in place until cholecystectomy in these cases. This is in contrast to the study by Hsieh et al. 11; this study reported that drainage durations longer than two weeks were associated with increased recurrence. Thus, the optimal duration of PC tube placement should be clarified in future studies.
In previous studies, the catheter was removed after confirmation of the patency of the cystic duct 1,2 or until the surgery 1,7,10. However, this was not seen in other studies 3,5. Although rare, Wang et al. 1 showed that 30.8% of patients were discharged with the PC tube in place until cholecystectomy. However, they could not reach a conclusion about the timing. Venara et al. 15 mentioned that the removal of the catheters can generally be performed after temporary clamping and that this is well-tolerated. In this study, we showed the beneficial effect of keeping the catheter in place until cholecystectomy. In addition, some authors used PC tube placement as a bridge and performed early surgery after a mean of 9.68 ± 6.45 days 10. Removal of the catheter after a median of 6.5 days was also performed for the immediate and beneficial effect on ACC 2. Therefore, larger scale studies are needed to clarify the most appropriate approach in relation to PC tube removal, either during the interval period or just before surgery in the operating theatre.
Recurrence after catheter removal is an important issue, especially in patients without surgical treatment. In previous studies, the rate ranged from 4% to 22% 1. Jang et al. 10 showed a recurrence rate of 19% during a mean follow-up period of six months. Wang and Hsieh 1,11 reported that a PC tube drainage longer than 32 days and two weeks was positively correlated with increased recurrence. Mucosal irritation and bacterial translocation through the catheter were thought to be responsible for recurrence. However, the authors still recommended the removal of the catheter after resolution of the acute illness 11. In this study, there were three patients with a recurrent ACC attack in group 1 and group 2, leading to a rate of 8.6% (three of 35 patients). This rate increases during longer follow-up periods 16. The presence of the gallstones is an important factor underlying higher recurrence rates after catheter removal (10). Recurrence even after placement of the PC tube is a real complication. Therefore, a definitive treatment of ACC requires surgery in appropriate patients.
Although an interval period of at least six to eight weeks is recommended by many institutional guidelines, the actual interval period has been shown to be longer, nine to eleven weeks 3,8. In this study, the mean was almost 12 weeks (85.4 ± 93.5 days + 20.7 ± 13.4 days) and nine weeks (64 ± 32.5 days) in group 2 and group 3, respectively. Two patients in group 2 underwent surgery after a very prolonged interval period of more than six months (not shown in the text). Limited operating room availability and recurrent episodes of gallstone-related complications, especially in the PC groups, were important issues forcing surgeons to further postpone surgery 3,8. Our findings also suggest that the actual interval periods for AC patients are longer than those of published guidelines, regardless of whether PC tube placement is applied or the catheter is left in place. Therefore, the timing of surgical treatment should be planned more concisely to prevent possible future recurrences.
The inclusion of a small number of patients in each group was the main limitation of the study. The small number of complications that lead to non-significant conclusions or prevented a detailed statistical analysis was another limitation. Decisions based on the attending surgeon to remove the PC tube or maintain it in situ might be an important factor in the present study. Therefore, the inclusion of more patients in the presence of predetermined criteria for the removal of the PC tube might help physicians to reach more significant results.
CONCLUSIONS
The optimal duration of PC drainage and the timing of PC tube removal remain unresolved. Keeping the PC tube in place until the time of surgery in surgically fit patients might help to prevent recurrent ACC attacks. Some patients are unfit for surgery and leaving the PC tube in place as long as possible might prevent recurrent ACC attacks in these patients.