INTRODUCTION
Acute pancreatitis (AP) is generally mild and self-limiting but can cause serious and life threatening complications in 20% of the cases. Thoracic complications of AP are uncommon and are usually represented by pleural effusion, pneumonia or pancreatic pleural fistula. However, enzymatic mediastinitis is a very uncommon complication in association with AP 2. The few cases reported so far occurred in patients treated conservatively. Herein, we describe the case of a 76-year-old female who developed an EM during the postoperative period after an open necrosectomy for acute necrotizing pancreatitis.
CASE REPORT
A 76-year-old female with no relevant medical history was admitted due to multi-organ failure (MOF) secondary to acute pancreatitis (alcoholic etiology). The patient was admitted to the Intensive Care Unit (ICU) and required cardiovascular and respiratory support. She presented signs of diffuse peritonitis. An abdominal computed tomography (CT) scan seven days after admission showed 50% necrosis of the pancreatic gland. A conservative management was initially attempted with empirical antibiotic therapy (meropenem and vancomycin), fluid resuscitation and enteral feeding via a nasojejunal tube. There was no clinical or radiological improvement during her stay in the ICU.
Four weeks later, the patient developed abdominal distension and a high temperature. A new CT-scan demonstrated multiple non-communicating peripancreatic collections. Gas bubbles were detected within the largest collection (Fig. 1), therefore a percutaneous drainage was inserted. Purulent exudate was obtained and Candida spp was isolated. Therefore, fluconazole was added to the treatment regimen.
Eight days following the percutaneous drainage, and in absence of clinical improvement, a new CT scan suggested no radiological changes. Due to the anatomical location of the collections and the unavailability of endoscopic drainage in that moment, an open surgical necrosectomy was performed. Three large collections were identified during surgery (retrogastric, retrorenal and paraaortic regions) and these were drained. Pancreatic necrosis was also removed and three drains were left in place (21 Fr silicone drains). The postoperative course was initially uneventful, with a daily drain output of approximately 100 ml of pancreatic fluid from the retrogastric drain. There was no output from other two drains (retrorenal and paraaortic region) and they were removed. The patient was transferred subsequently to the ward due to clinical improvement.

Fig. 1 Abdominal CT scan showing a large peripancreatic collection containing gas bubbles (yellow arrow).
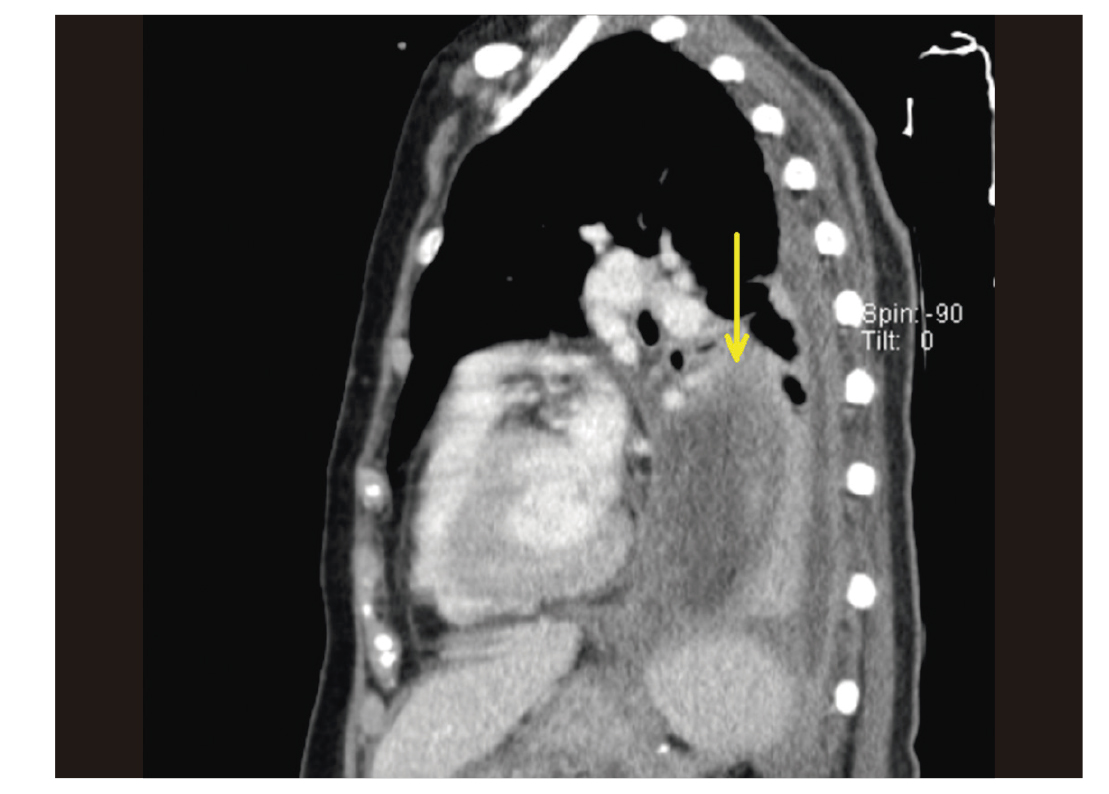
Unfortunately, the retrogastric drain was accidentally removed two weeks after surgery. Five days later, the patient was admitted to the ICU as an emergency due to acute respiratory failure associated with hemodynamic instability and atrial fibrillation. A new thoracic and abdominal CT scan showed a large collection located in posterior mediastinum, which was not present in the previous CT scan (Fig. 2). A new small peripancreatic collection was also identified.
Due to the clinical conditions, an open thoracotomy was urgently performed. A mediastinal collection was drained and a purulent exudate was obtained. A percutaneous drainage of the peripancreatic collection was also performed. Medical management of the cardiac and respiratory failure was successful after mediastinal surgical drainage. As the clinical situation improved, the patient was transferred to the ward and discharged three weeks later, with a daily abdominal drain output of around 100 ml (controlled fistula) and no symptoms (medical treatment with octreotide).
Three months later, a pancreatic magnetic resonance imaging (MRI) showed a disruption of the Wirsung's duct in the pancreatic body. Endoscopic management was offered (pancreatic stent) but the patient refused any invasive treatments. The drainage was removed nine months later. After a two-year follow-up, the patient is well and has not been admitted to hospital. She has also stopped drinking alcohol.
DISCUSSION
Acute pancreatitis can lead to several types of complications. Thoracic complications of AP are uncommon but they should be kept in mind due to their serious consequences. Acute mediastinitis is a very uncommon but life-threatening complication of AP.
The digestion of the parietal peritoneum by pancreatic enzymes (similarly to pancreatic-pleural fistula) and its passage to the thoracic cage through the esophageal or aortic hiatus have been suggested as possible mechanisms 2,3. The diffusion of pancreatic fluid to the mediastinum has also been defined as wirsungo-mediastinal fistula 6. This concept refers to the anatomical disruption of the Wirsung's duct, which may cause pancreatic ascites and mediastinal collections.
This is the first case that describes EM as a complication of surgical necrosectomy. Previous studies related to this entity have reported an EM episode during the conservative management of AP. In the case described here, pancreatic necrosectomy was performed to drain the peripancreatic collections but the accidental withdrawal of the surgical drain may have contributed to EM development. Pancreatic fluid started to collect within the abdomen when the drain fell out, which might have allowed pancreatic enzymes to reach the mediastinum. This raises the concern that EM could also occur following an elective pancreatic surgery in case of an uncontrolled pancreatic fistula.
The occurrence of thoracic symptoms such as chest pain, abrupt dyspnea and tachycardia in patients with AP should raise the suspicion of EM. These symptoms may be confused with other thoracic complications such as acute myocardial infarction, pulmonary thromboembolism and aortic dissection, etc. Serious complications related to EM (such as those described previously) should be considered as they are life-threatening complications. In these cases, diagnosis or treatment delay can lead to patient death.
A review of the available literature with regard to EM as a complication of pancreatitis identified only eleven cases (Table 1). A conservative management was attempted in most cases. However, surgical drainage of the mediastinum and abdominal control of the pancreatic leak was usually required 4. As shown in table 1, EM usually occurs in patients with chronic pancreatitis or recurrent acute pancreatitis with pancreatic duct disruption. In our case, there is no clear evidence of chronic pancreatitis, although ductal disruption has been previously described as a complication of invasive treatment for necrotizing pancreatitis and has usually led to an external pancreatic fistula.