Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Española de Cirugía Oral y Maxilofacial
versão On-line ISSN 2173-9161versão impressa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.29 no.4 Madrid Jul./Ago. 2007
ARTÍCULO CLÍNICO
Guided bone regeneration using aluminum oxide membrane in combination with osseointegrated implants
Regeneración ósea guiada utilizando membrana de óxido de aluminio en combinación con implantes oseointegrados
M. Isa Majluf1, J. Harán Vega2, G. Moreno Zárate3
1 Profesor Asistente, Departamento de Cirugía
y Traumatología Maxilo-Facial.
2 Cirujano Dentista.
3 Profesor del Departamento de Radiología.
Universidad de Chile, Santiago de Chile, Chile
ABSTRACT
Alveolar bone loss has been a very important cause of complications in osseointegrated implant rehabilitation of edentulous patients. This paper evaluates the effectiveness of aluminum oxide membrane (Allumina) in the collapsed alveolar ridge where implants were used. Seven sites were studied in 5 patients. In each of these sites a HIS implant plus a non-biodegradable oxide aluminum membrane (Allumina®), was placed for 14 weeks. All patients were treated with the same surgical protocol. The average gain (in mm) obtained in decreasing order was as follows: ANM: 1.7 mm, ANME: 1.6 mm, AND: 1.1mm, AV: 1.0mm, AP: 0.5mm. The clinical results were radiographically verified and these showed bone neoformation, in addition to favorable peri-implant bone density. The t-Student statistical analysis based on the clinical results was significant for all the parameters evaluated with the exception of AP.
Key words: Membrane; Allumina; Bony regeneration; Implant.
RESUMEN
La reabsorción ósea de los maxilares ha sido una de las mayores complicaciones al momento de rehabilitar a pacientes con implantes oseointegrados. El siguiente estudio evaluó la efectividad de la membrana de óxido de aluminio (alúmina), en la regeneración ósea de rebordes colapsados y alvéolos en los que se colocaron implantes. De un total de cinco pacientes seleccionados, se estudiaron siete sitios de los cuales tres correspondieron a un solo paciente. En cada sitio (alvéolo o reborde colapsado) se colocó un implante de titanio del sistema HIS y una membrana no biodegradable de óxido de aluminio (Allumina®), la cual fue retirada a las 14 semanas. Todos los pacientes fueron sometidos al mismo procedimiento quirúrgico. La ganancia promedio en mm obtenidos en orden decreciente fue la siguiente: ANM: 1.7mm, ANME: 1.6mm, AND: 1.1mm, AV: 1.0mm, AP: 0.5mm. Los resultados radiográficos ratificaron los resultados clínicos en cuanto a neoformación ósea, observándose además una favorable densidad ósea periimplantaria. El análisis estadístico (basado en los resultados clínicos) t-student fue significativo para todos los parámetros evaluados con excepción de AP.
Palabras clave: Membrana; Alúmina; Regeneración ósea; Implante.
Introduction
Alveolar bone resorption is a physiological process that can arise as a result of dental extraction.11 Sufficient bone volume is considered the most important prerequisite for the long-term prognosis of implants.9 Numerous authors have carried out studies with a large quantity of graft and membrane material with the aim of improving the condition of the ridge, and also in cases of dehiscence when placing the implant. These biomaterials have been used independently and together, and different degrees of success have been achieved.18 Most of the membranes used in guided bone regeneration require a filling material for avoiding collapse.
In 1999 Isa and col. used aluminum oxide membrane for preserving the alveolar ridge after the extraction of lower third molars without graft material, and they obtained excellent results.25 Petersen and cols. used these same aluminum membranes for treating type II fork branches in humans with excellent results.28 This study provides our results with aluminum oxide membranes for improving the condition of the alveolar ridge in which implants were installed, without using graft material.
Material and method
Patients. Inclusion criteria
• Good general and oral health.
• Total absence of any contraindication for rehabilitation with osseointegrated implants.
• Good disposition and capacity for understanding and following instructions strictly.
• Young adults between the ages of 20 and 45.
• Patients with collapsed edentulous areas, with sufficient
remaining bone to permit the initial stability of the implanted structure, or teeth with signs of extraction and bone loss, without any pathologies or infectious processes.
Five patients made up the selected group with 7 "study sites" into which an implant was inserted with its respective membrane.
Site 1- Socket tooth 19; Site 2- Socket tooth 12; Site 3- Socket tooth 8; Site 4-Alveolar ridge in site of tooth 7; Site 5 – Alveolar ridge in site of tooth 8; Site 6 – Alveolar ridge in site of tooth 9; Site 7 – Alveolar ridge in site of tooth 10.
In Sites 1-2 and 3, implants were immediately inserted. Sites 5-6 and 7 related to the same patient.
For this study an aluminum oxide membrane was used as a physical barrier,25 mean thickness (0.06 mm). This was kept in place for 14 weeks.
Clinical study
With regard to the sockets, the following measurements were taken:
Height of the vestibular plate at mean portion. Height of the palatal or lingual plate at mean portion, width of socket at mean portion, width of socket at mesial portion and width of socket at distal portion. In collapsed ridges where the plates could not be distinguished, the measurements were taken once the bony bed that was to house the implant had been made, and these were the following:
Height of the vestibular ridge of the bony bed at mean portion, height of the palatal or lingual ridge of the bony bed at mean portion, width of the ridge at mean portion, width of the ridge at mesial portion and width of the ridge at distal portion. For registering height, two sterile metallic rulers were used. One of them was positioned at the points previously indicated up to an imaginary line that corresponded with the projection of the occlusal plane. For this, another sterile ruler was used in a horizontal direction as a reference. This ruler was put against the incisal borders or occlusal faces of the teeth by the gap. In this way the height was registered in a vertical sense, perpendicular to the reference point.
The thickness dimensions were registered with a metal calibrator.
These measurements were taken at the time of the first surgery before the placement of the implants and membranes, as well as at the second intervention when the membrane was removed at 14 weeks (Fig. 1).
Panoramic and retroalveolar radiographies were
used before the first surgical intervention, with data of not more than a month
before the date of the surgical intervention, and once the membranes had been
removed at 14 weeks in order to measure density and bone height.
Surgical act
In the pre-operative period, Amoxicillin of 750mg was prescribed, 1 tablet 6 hours before the intervention, and Betamethasone 0.6 mg, 5 tablets half an hour before the surgery. Infiltrative anesthetic technique, Mepivacaine at 2%. Tooth extractions were carried out in the immediate implant cases. Then, the two cases in the study were dealt with indistinctly in the following fashion:
Mucoperiosteal crevicular flap with two vertical incisions, from the mucogingival union to the base of the papillae at the edge of the gap (mesially and distally). Making of the bony bed in the collapsed ridge or socket according to the case, insertion of the implant into the surgical bed following the conventional technique. Partial sectioning of the periosteum from the base of the flap in order to give more elasticity. Handling, shaping and installing the membrane, ensuring the bone is completely sealed with the membrane. Suturing, leaving the membrane totally covered.
All the patients were given postoperative medication with Amoxicillin 750 mg every 8 hours for 7 days, analgesics, of choice Nimesulide (Aldoron®) 100 mg 1 tablet every 12 hours depending on the pain, chlorhexidine gluconate rinse at 0.12% twice a day for 14 days. In membrane exposure cases the rinse was continued for longer.
Revulsive treatment was given for controlling the edema and instructions were given to the patient not to speak or gesticulate much. When wishing to communicate they had to do this in writing for at least the first week. Finally, the evaluations were carried out the second day after the surgery, then weekly during the first month, and every two weeks for the remaining months. The patients with exposed membranes were followed weekly. (Fig. 2)
Results
Clinical results. After the first intervention, there was only slight inflammation that did not continue for more than three days. As there were no major complications, the patients continued using Chlorhexidine (Perio-Aid®) for the 15 days indicated. In 3 patients (Sites N°1, N°2, and N°4) there was premature exposure. Sites N°1 and N°4 were those with the greatest exposure, and as there were no associated signs or symptoms of infection, the patients were instructed to use additional antiseptic and to maintain good plaque control for the remainder of the study. Due to this, the barrier did not have to be removed before the stipulated time.
At 14 weeks the membranes were removed. Those with premature exposure were easily removed and large flaps were not required. Under the more exposed membranes and in relation with the inside area (over the defect) granulation tissue could be observed but only on the surface, as on carrying out the second clinical measurements the presence of newly formed tissue could be observed underneath. Site Nº2, despite slight exposure, did not show these characteristics as when the membrane was removed, tissue with a periosteal appearance could be observed with new bone underneath. In the remaining Sites without exposure (Nº3, Nº5, Nº6 and Nº7), the same pattern was repeated on removing the membrane, as tissue that was more or less like periosteum could be observed that was firm and thick, with a transparent appearance, and which was in the process of maturing.
In general, all the new clinical measurements revealed new bone tissue formation, with the exception of Site Nº1 that had vestibular and palatal height that was slightly lower. However, the dimensions in relation to the width of the ridge increased favorably, especially mesially and distally.
Dehiscences concerning the implants were noticeably repaired in most cases, with the exception of Site Nº1, as the vestibular defect remained.
A special mention should be made of Site Nº4 that initially had a very collapsed ridge and premature membrane exposure. The recovery of the ridge dimensions, especially of the mean, mesial and distal widths in this site was noteworthy.
Tables 1 and 2 give a summary of the clinical measurements taken before and after the placement of membranes and implants, as well as the millimeters gained during the study period.
The clinical results are reflected in the
average mm measurement in all the sites, which were favorable. A special mention
should be made of the general recovery of the medial and mesial aspects, with an
average of 1.7 mm and 1.6 mm
respectively (Figs. 3 and
4).
Statistical analysis
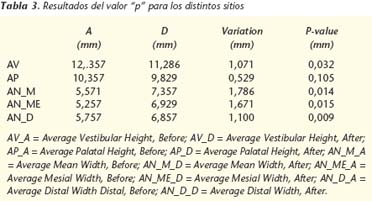
The clinical results were subjected to a statistical t-Student analysis for paired samples. This test was chosen because it allows the comparison of two values, before and after, in the same observation unit.
The results of the pvalue for the different sites are registered in table 3.
The results of the statistical analysis reveal that the changes in height and thickness of the ridge, before and after membrane placement, are statistically significant in all the parameters evaluated, with the exception of the palatal Height parameter that had a final p-value that was more than 0.05.
Discussion
For our study we used aluminum oxide membrane, which unlike other membranes allows maintaining the space underneath without any graft material, for repairing mainly periimplant bone defects and for recovering and maintaining the dimensions of the alveolar ridge.
Our study period was limited to 14 weeks. After this period the new height and thickness of the ridges was recorded. Membrane removal in this period and not afterwards, could encourage the bone tissue that has formed to mature, as the membrane used is impermeable and nutrients are not able to pass through to the reparation area. It is the periosteum itself that has to encourage this process once the barrier has been removed. The results reveal on average a greater amount of bone tissue in the parameters evaluated. Palatal height was the only parameter evaluated that did not have a statistically significant result. In spite of this, the values of the second measurements of this parameter gave a final positive result. That is to say, a gain in mm was obtained, but to a lesser extent than in the rest.
The difference in the results regarding palatal and vestibular height should not be surprising if we take into consideration that, in general, dehiscences arise in the vestibular area. On the other hand, numerous studies carried out previously18 have attributed to the membranes used for GTR, a greater ability for alveolar ridge recovery in a horizontal sense than in a vertical sense, mainly due to the tendency of these to collapse, as a result of pressure from soft tissues.
The membrane used in this study showed no sign of collapse and in all cases the results were favorable. However, given the fact that a medium thickness membrane was used, which is not usually indicated for a considerable height increases, this gain was achieved and a large space underneath was avoided, particularly heightwise, on being adapted to the sites in the study. This could have been the motive for the later height measurements being clinically less significant.
Site Nº1 that corresponded to the socket of tooth 19, was the only site situated in the mandible and the only site to suffer height loss, vestibular as well as palatal. The type of irrigation in the mandible and the design of the flap (Newman) could explain in part these results. Vascular supply to the mandible depends principally on soft tissue supply, particularly from the periosteum, which on being sectioned from its base could limit part of the irrigation to the area, hampering the osteogenesis process.24-26 In this site in particular, we did not consider premature membrane exposure on its own, as a reason behind the loss in bone height, given the very good results in other sites, which similarly suffered exposures, but were situated in the maxilla unlike in this case.
Premature exposure of the membrane in Sites 1,2 and 4 could be related to more than one factor. The patients in Sites 1 and 4 were individuals with jobs that required them to communicate verbally (kindergarten teacher and Vet respectively). This could have favored the traction of the flap with the periosteum that was sectioned practically at its base. On the other hand, the implant situated in Site Nº1 was immediate, and this made it necessary to section the periosteum more deeply in order to give the flap greater elasticity and to cover the implant and the membrane of a wide socket in the molar region.
Perhaps the surgical protocol could be slightly modified, and a prudent post-extraction time period could be observed, until a sufficient amount of soft tissue appeared that would enable us to avoid sectioning the periosteum and to suture with less tension.
On the other hand, in spite of the implant in Site 4 being immediate, that is, it had sufficient soft tissue to enable good primary closure, the membrane became exposed prematurely. In spite of this, the results of the second measurements in this site were noteworthy. Premature exposure of the membrane in this case did not lead to any complication or bone loss as occurred in the study of other membranes with premature exposure that led to infection and bone loss.22-23-25 The use of chlorhexidine rinses in patients with premature exposure without doubt contributed to maintaining good plaque control and any infectious complications that would have hastened the removal of the membrane were avoided.
Site Nº3 did not suffer membrane exposure despite having an immediate implant, and in the radiographic evaluation an intact alveolar bone crest could be observed at three and a half months. That is to say, the aluminum membrane also served to maintain the original dimensions of the border, and even to increase them, and an average mm gain was obtained in all the parameters studied. This fact is of great importance if we consider the future rehabilitation of the site, as the membrane encourages bone regeneration in the area and it halts one of the most trivial problems of dental extractions, which is bone resorption.
Conclusions
Aluminum oxide membrane is capable of maintaining extra-skeletal tissue isolated from the bone repair site, and it avoids the migration of epithelial cells and of connective tissue. Even in the cases where the membrane became exposed, dehiscences were repaired on installing the implants, which led to an increase in the vertical (except in site Nº1) as well as horizontal dimension of the ridge, despite not using any graft material underneath, and the space created was filled by the blood clot, which hypothetically favors the concentration of growth factors and therefore, of osteogenesis.
Suggestions
• Aluminum oxide membranes should be used in a larger number of patients.
• Histological studies should be carried out of the tissue formed directly underneath the membrane.
• Microbiological studies should be carried out on the adherence of bacteria to the membrane.
• Finally we would like to suggest waiting for mucosal closure before placing the implants and membranes once the extraction has been carried out. In this way, primary closure tension can be avoided and the sectioning the periosteum.
Acknowledgments
To the company Demac for donating Allumina® membrane.
To Doctor Benjamín Martínez, ex-pathologist of the "Univesidad de Chile" and staff member of the "Bioestadística de la Universidad Mayor" for his assessment in the statistical analysis.
![]() Correspondence:
Correspondence:
Dr. Mario Isa Majluf
Apdoquindo 4100 dpto. 601 Las Condes
Santiago de de Chile, Chile
Email: Isamohor@ctcinternet.cl
Recibido:
16.01.06
Aceptado: 01.06.07
References
1. Christop y cols. Single stage surgery combining transmucosal implant placement with guided bone regeneration and bioresorbable materials. Clin Oral Impl Res 2001;12:9-18. [ Links ]
2. Otti P, y cols. The Procera AllCeram Sistem. Int J Periodontics Restorative dent 2000; 20:151-61. [ Links ]
3. Malmquist J, y cols. Successful implant restoration with the use of barrier membranes. J Oral Maxillofac Surg 1999;57:1114-6. [ Links ]
4. Dupoirieux L, y cols. Comparative study of three different membranes for guided bone regeneration of rat cranial defects. Int J Maxillofac Surg 2001;30:58- 62. [ Links ]
5. Dörfer C, y cols. Regenerative periodontal surgery in interproximal intrabony defects with biodegradable barriers. J Clin Periodontal 2000;27:162-8. [ Links ]
6. Zitzmann N, y cols. Long-term results of implants treated with guided bone regeneration: A 5-year prospective study. Int J Oral Maxillofac Impl 2001;16:355- 66. [ Links ]
7. Karapataki S, y cols. Healing following GTR treatment of intrabony defects distal to mandibular 2nd molars using resorbable and non-resorbable barriers. J Clin Periodontal 2000;27:333-40. [ Links ]
8. Cruz M, y cols. Utilicao da alumina como membrana na Regeneracao Guiada dos Tecidos. Odontologico Moderno Sao Paulo 1993;20:6-13. [ Links ]
9. Yasonuri S, y cols. Aumento del reborde alveolar con redes de titanio y hueso autógeno. Oral Surg Oral Med Oral Pathol 2000;89:268-70. [ Links ]
10. Nociti F, y cols. Absorbable versus non-absorbable membranes and bone grafts in the treatment of ligature-induced peri-implantitis defects in dogs: A histometric investigation. Int J Oral Maxillofac Impl 2001;16:646-52. [ Links ]
11. Barry K, y cols. Extraction site reconstruction for alveolar ridge preservation. Part 1: Rationale and material selection. Journal of Oral Implantology 2001;27:187-93. [ Links ]
12. Barry K,y cols. Extraction site reconstruction for alveolar ridge preservation. Part 2: Membrane-Assisted surgical technique. Journal of Oral Implantology 2001;27:194-7. [ Links ]
13. Bunyaratavej P, y cols. Collagen Membranes: A Review. J Periodontol 2001;72:215-29. [ Links ]
14. Celleti R, y cols. Guided tissue regeneration around dental implants in immediate extraction sockets: Comparison of e-PTFE and a new titanium membrane. Int Periodont Rest Dent 1994;14:243-53. [ Links ]
15. Mohamed A, y cols. Immediate implants in fresh posterior extraccion sockets: Report of two cases. J Oral Implantol 2001; 2:123-6. [ Links ]
16. Marlin E, Gher et. al. Combined dental implant and guided tissue regeneration therapy in humans. Int J Periodont Rest Dent 1994;14:333-47. [ Links ]
17. Nociti F, y cols. Absorbable versus nonabsorbable membranes and bone grafts in the treatment of ligature-induced periimplantitis defects in dogs. Clin Oral Impl Rest 2001;12:115-20. [ Links ]
18. Massimo M, y cols. Vertical ridge augmentation using a membrane technique associated with osseointegrated implants. Int J Periodont Rest Dent 1994;14:497-511. [ Links ]
19. Diès F, y cols. Bone regeneration in extraction sites after inmediate placement of an e-PTFE membrane with or without a biomaterial. Clin Oral Impl Res 1996; 7:277-85. [ Links ]
20. Von Arx, y cols. Lateral ridge augmentation using difeerent bone fillers and barriers membrane application. Clin Oral Impl Res 2001;12:260- 9. [ Links ]
21. Buser D, y cols. Regeneration and enlargement of jaw bone using guided tissue regeneration. Clin Oral Impl Rest 1990;1:22-32. [ Links ]
22. Gher M, y cols. Bone grafting and guided bone regeneration for immediate dental implants in humans. J Periodontol 1994;65:881-91. [ Links ]
23. Wang H; y cols. Adherence of oral microorgenisms to guided tissue membranes: In vitro study. J Periodontol 1994;65:211-8. [ Links ]
24. Testut L, Jacob O. Tratado de Anatomía Topográfica con aplicaciones medicoquirúrgicas. 1964:207. [ Links ]
25. Isa M y col. Uso de la membrana Allumina® en la preservación del reborde alveolar postextracción. Magazine Internacional College of Dentists Section Four 2001;8:61-8. [ Links ]
26. Walter JB, Hamilton MC, Israel MS. Principles of pathology for dental students. (4a.ed). Edinburgh: Churchill Livingstone, 1981;p.p.570. [ Links ]
27. Guitián P, y cols. Preparación de cavidades por microabrasión. Facultad de Medicina y Odontología de la universidad Santiago de Compostela. http://www.infomed.es/mode/mode97/mesa3.html. [ Links ]
28. Peterson A, y cols. Avaliacao cínica da técnica de regeneracao tecidual guiada utilizando uma barreira de óxido de alumínio no tratamento de lesoes de furca classe II em humanos: relato de 12 casos. Projecto fundo de incentivo a pesquisa (FIP), nº 94/022 Pontificia Universidad de Católica de Minas Gerais. [ Links ]
29. Wilson T, y cols. Implants placed in immediate extraccion sites: a report of histologic and histometric analysis of human biopsies. Int J Oral Maxillofac Impl 1998;13:333-41. [ Links ]
30. Steven G, Lewis. Sisitema de implantes Branemark. Editorial Espax S.A. 1991; p.p. 1-10. [ Links ]
31. Nyman, y cols. New attachment following surgical treatment of human periodontal disease. J Clin Periodontol 1982;9:290-6. [ Links ]
32. Takashi T, y cols. Migration of osteoblastic cells on various guided bone regeneration membranes. Clin Oral Impl Res 2001;12:332-8. [ Links ]
33. Rocuzzo M, y cols. Comparative study of a bioresorbable and a nonbioresorbable membrane in treatment of human bucal gingival recessions. J Periodontol 1996;67:7-14. [ Links ]
34. Piattelli A, y cols. Histological evaluation of bone reaction to aluminium oxide dental implants in man. Biomaterials 1996;17:711-4. [ Links ]











 texto em
texto em