Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Cirugía Oral y Maxilofacial
versión On-line ISSN 2173-9161versión impresa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.31 no.2 Madrid mar./abr. 2009
DISCUSIÓN
Mandibular osteosynthesis failure. Biomechanical and therapeutic considerations. Two clinical cases
Fracaso de la osteosintesis mandibular. Consideraciones biomecánicas y tratamiento. A propósito de dos casos clínicos
Sergio Martínez-Villalobos Castillo
Grupo AO España CMF. Member European AO-CMF Specialty Board. Hospital Universitario "Virgen de las Nieves". Granada. España
The prolonged controversy regarding mandibular osteosynthesis that faced off the French and Belgian schools, followers of the biomechanical principles of Champy, against AO-ASIF postulates in the two last decades of the 20th century is now completely outdated. The principles of the techniques known, respectively, as «Semi-rigid Fixation» and «Internal Rigid Fixation», are now established as simple surgical techniques rather than competing, mutually exclusive, philosophies. The concept of «Adapted Fixation» currently is accepted universally as the point of encounter between the two positions, forming the central axis of proper therapeutic planning adapted to the biomechanical needs and the particular fracture or osteotomy of each individual patient.
The starting point is to identify the patients biological reality and the intrinsic characteristics of the fracture in order to decide whether the patient in question requires osteosynthesis. A fixation technique must be chosen that provides «Sufficient Stability» and a "Functionally Stable» solution for the bone-plate binomial. Minimizing the maxillomandibular fixation period (MMF) must be a priority, not only to ensure the patients postoperative comfort by shortening as much as possible the period of «stomatognathic disability» but, above all, to prevent the deleterious effects of prolonged MMF (fracture disease, Robert Danis 1949).
The diagnosis is based on a global analysis of the patients biological situation, which can determine per se the type of fixation necessary to ensure fracture healing, forestalling potential local and systemic complications in cases in which an insufficient fixation must be reinforced with a period of prolonged MMF in certain patients with multiple pathologies. At the same time, meticulous analysis of the mechanical characteristics of the fracture is essential for rational decision- making. The aim is to understand the simple concept, often overlooked in the course of routine practice under the whirlwind pressures of care, that «we dont operate on radiographs, we operate on patients».
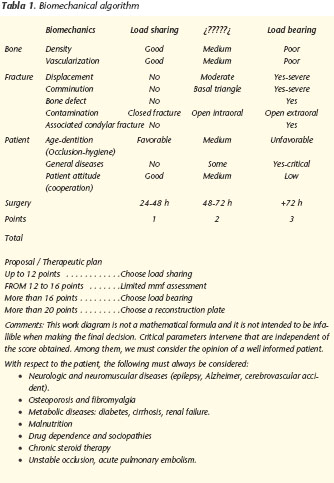
In my opinion a meticulous diagnosis that systematically takes weighs all these parameters is of capital importance in making well-informed decisions. It doesnt matter what the decision is, but it should never be based solely on the simple action of «making a radiograph of the face». An algorithm can be very useful for applying to all cases of mandibular fracture as a reasoned exercise for planning treatment, which includes the type of approach and fixation to be used and the need for MMF. This is an exercise that we should demand from our interns in every case (Table 1).
After this detailed medical and surgical analysis we will be better prepared to assess the biomechanical situation of each fracture as «Load Sharing» or «Load Bearing» in order to design the appropriate «Adapted Fixation».
Conceptually, a load-sharing situation is one in which the patient and the patients overall biological status are capable of ensuring the healing of a particular fracture. In these cases, osteosynthesis has a secondary or coadjuvant role and the task of healing is shared between the patient and the bone. In load-bearing situations, in contrast, either the patients biological circumstances or the fracture characteristics, or both, are such that the fixation system plays a prominent role in the repair process and bone consolidation.
Osteosynthesis failure usually is secondary to an unfortunate therapeutic approach in which the principles cited above have not been properly assessed, rather than to errors in the surgical technique. Nonetheless, it is evident that technical skill and a minimum surgical experience in the management of implants are necessary, particularly with the stronger bicortical fixation implants.
The authors are right in their idea of presenting two resounding failures (a double failure in the first case) as the result of an incorrect biomechanical assessment, although I do not agree with their claim that these situations are uncommon. Many of our patients undergo more or less prolonged periods of MMF that could have been avoided if suitable fixation had been used, although most of them do not have to return to the operating room. I also suspect that there are many other patients with osteosynthesis failures of discrete clinical importance that are not readmitted to hospitals and, for one reason or another, end up coexisting with a poor functional result that might have been avoided.
We can learn much from the two cases presented by the authors, which I will discuss in detail:
The first case was a patient with Downs syndrome who had a double fracture of the left mandibular body and right angle. These two elements of information suffice to label the situation unequivocally as load-bearing. I have to disagree with the authors claim that uncooperative patients may require MMF: in my opinion, the opposite is true. A patient with Downs syndrome should not be a candidate for maxillomandibular fixation, even if only because of their lack of cooperation. However, this patient had the additional problem of a «complex,» or not simple, double fracture. Mixed osteosynthesis was performed using with small plates with an extraoral approach on the right side (which I believe is unacceptable) that failed to provide the necessary stability in this case. The evidence of the panoramic radiograph can be interpreted as indicating that this woman had focal osteomyelitis of the right angle that caused her to lose her second molar. She had to undergo prolonged MMF with maxillo-mandibular screws in an attempt to solve the problem. This was another error, doing no more than delay the inevitable reintervention and new fixation. Unfortunately, the second intervention failed, probably not due to the presence of especially pathogenic germs or the patients lack of hygiene. The 2.5 reconstruction plate was not placed in the middle of any locus, it was placed in the neutral zone of the mandibular angle-body. At least three screws were placed accurately in the trajectory of the inferior dental nerve and, more importantly, one of them was inserted in the fracture locus. The bridge osteosynthesis technique was erroneous because it is well established that the reconstruction plate must be placed in the basal area, generously bridging the fracture area. At least three screws (and better four) must be inserted on both sides of the plate in healthy bone. On this occasion, the error was more technical than conceptual (although it also was conceptual) and the outcome was failure. The presence of a small locking plate in the basal is anecdotic because it was biomechanically useless. It may be thought that after five months of focal osteomyelitis with its typical exacerbations and sterile periods of MMF associated with kilograms of antibiotics by different routes the patient only received the third and definitive reconstructive surgery with an immediate bone graft and bridge osteosynthesis by chance. It is noteworthy that the presence of an infected consolidation failure (focal osteomyelitis) is not a contraindication for performing nonvascularized bone graft, as long as the osteosynthesis is adequate and provides sufficient stability for bone healing without counterproductive mechanical disturbances. Finally, we must assume that the followup panoramic radiograph was not made at one year of the postoperative period, but in the immediate postoperative period, and that there is a risk that MMF screws may have been overlooked under the mucosa. Whatever the case, it should be emphasized that even with the graft, MMF was not necessary and does not contribute anything to graft revascularization and viability when fixation is adequate and soft tissue coverage is sufficient.
In the second case presented, we have a typical failure of fixation with small plates in a jaw with moderate atrophy, an unfavorable «slide» fracture, and bilateral condylar fractures that require early active mobilization: This is unequivocally a load-bearing situation. The postoperative orthopantomography speaks for itself, showing inadequate reduction (presumably by an intraoral approach) and an obviously insufficient osteosynthesis. Months later, the typical avascular pseudoarthrosis with consolidation failure and collapse of the proximal mandibular fragment was evident. Even in the absence of infection, this situation is functionally unviable. The repair surgery performed confirmed that bone grafts are of choice in cases in which the defect is more than 1 cm wide. Again, I have to assume that the orthopantomography shown is from the immediate postoperative period and not 6 months, due to the presence of MMF screws.
Finally, the authors briefly discuss the benefits of locking plates for the fixation of fractures and mandibular defects. It is known that stability is achieved with conventional plates by the perfect adaptation of the plate to the bone profile and perpendicular compression by the screws of the plate against the bone. It has been demonstrated that compression jeopardizes the vascularization of the cortical bone, which may unfavorably affect consolidation. In locking plates, the stability of the osteosynthesis system depends on the mechanical unit of the plate affixed by its screws (as a an external locking device), which diminishes the focal compression of the cortical and favors locus revascularization and fracture healing. Therefore, the use of Unilock type locking systems is a technique of choice in cases that are compromised or complicated either initially or as a consequence of failure.
In conclusion, and parting from the idea that any patient may experience complications even in the best hands, we must critically examine our errors and failures, looking backward to consider what might have ensued or been avoided if our selection or planning had been different. More likely, we will reach the same conclusion that once was transmitted to us by a Master:
«We will rarely regret using a stronger fixation system when using a clean surgical technique but, in contrast, on many occasions we will regret not using one.»
Prof. Brian Alpert











 texto en
texto en