Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Española de Cirugía Oral y Maxilofacial
versão On-line ISSN 2173-9161versão impressa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.36 no.4 Madrid Out./Dez. 2014
https://dx.doi.org/10.1016/j.maxilo.2012.08.004
CLINICAL REPORT
Circummandibular wiring made easy: A case report
Facilitación de una ligadura de alambre circunmaxilar: informe de un caso
Jasmeet Singha, Rajib Khadkab, Prakash Chandra Chaturvedib, Vivek Singhb y Puja Raic
a Department of Oral and Maxillofacial Surgery, BBD College of Dental Sciences, Lucknow, India
b Department of Oral and Maxillofacial Surgery, UCMS College of Dental Sciences, Bhairahawa, Nepal
c Department of Oral Medicine and Radiology, Maharana Pratap College of Dental Sciences, Gwalior, India
ABSTRACT
Mandibular fractures are less common in children as compared to adults. The treatment plan in children has to be modified as compared to adults considering the presence of tooth buds and potential disturbances in growth. Use of acrylic splints has been one of the popular techniques in children because of its relatively easy placement and reduced risk of hindrances to growth of jaw. These splints have been traditionally been fixed with the help of cements and circummandibular wires. We describe the use of intravenous cannula stilete instead of traditional bone awl to secure the splint in place.
Key words: Paediatric mandibular fracture. Circummandibular wiring. Intravenous cannula stilete.
RESUMEN
En comparación con los adultos, las fracturas maxilares son menos frecuentes en niños. El plan de tratamiento en niños ha de modificarse en comparación con los adultos considerando la presencia de los brotes dentales y las posibles alteraciones del crecimiento. La utilización de férulas acrílicas ha sido una de las técnicas populares en niños debido a su facilidad de colocación y a la reducción del riesgo de obstáculos en el crecimiento maxilar. Tradicionalmente estas férulas se han fijado con la ayuda de cemento y una ligadura de alambre circunmaxilar. Describimos el uso de una cánula-estilete intravenoso en lugar del instrumento tradicional usado para fijar la férula.
Palabras clave: Fractura maxilar pediátrica. Ligadura de alambre circunmaxilar. Cánula-estilete intravenoso.
Paradoxically, facial injuries in children are much less common than in adults, particularly during the first 5 years of life.1 The incidence is low, ranging from 0.6 to 1.2%. Many pediatric mandible fractures can be treated without surgical exploration of the fracture site.2 In children, the frequent absence of the teeth due to primary teeth exfoliation and the poor retentive shape of deciduous teeth crowns make the traditional use of arch bars and interdental ligature impossible to apply. Splinting the fractured pediatric mandible with an acrylic splint, retained by circummandibular wires, remains a viable option.3 We describe a relatively atraumatic technique for placing circummandibular wires using an intravenous cannula stilete (IVCS) in two cases of pediatric mandibular fracture.
Cases
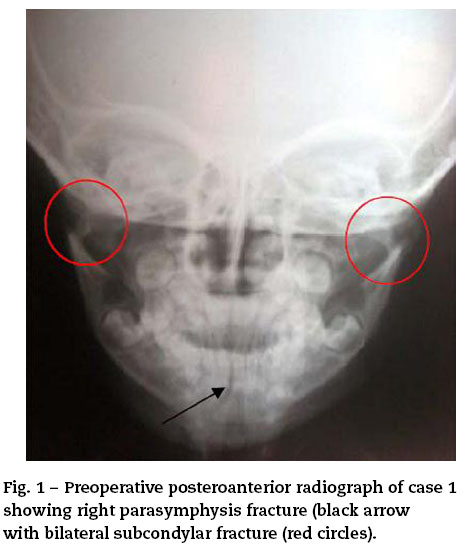
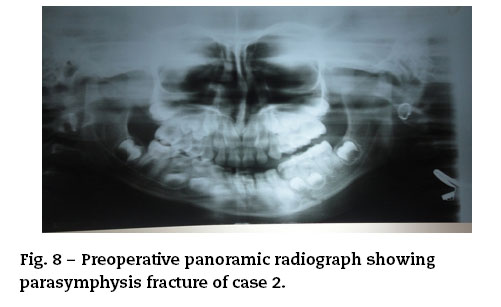
We present two cases, one with right parasymphysis fracture and bilateral subcondylar fracture (Figs. 1 and 2) and another with isolated right parasymphysis (Figs. 7 and 8) fracture aged three and four years respectively. There was a history of fall while playing in both the cases. Intra oral examination revealed complete set of deciduous dentition with mild derangement of occlusion. Closed reduction with open cap splints retained with CMW was planned and executed.
Technique
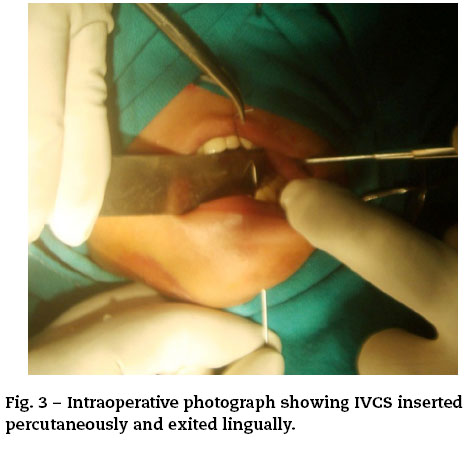
IVCS is inserted percutaneously and exited intraorally on the lingual side taking care to stay as close as possible to the lingual surface of the mandible so as to avoid damage to submandibular gland (Fig. 3). Then the wire is passed through the lumen of IVCS and held intraorally. Now the IVCS is traced back following the lower border of the mandible with bevel facing the bone. IVCS is then exited buccally (Fig. 4) and the wire is cut to the desired length. Preadjusted acrylic splint is seated in place and secured with the help of circummandibular wires (Figs. 5, 6, 9, and 10).
Discussion
Amongst the facial fractures, mandibular fractures are the second most common fractures reported in children preceded by nasal fractures. Mid face fractures are rare in case of children because of its retrusive position relative to prominent calvaria.4 The etiology of mandibular fractures in children differs from adults. Motor vehicle accidents, falls and sports are the most common causes of mandibular fractures in most countries.
The clinical signs and symptoms of a fractured mandible in a child are the same as in an adult: pain, swelling, trismus, derangement of occlusion, sublingual hematoma, step deformity, deviation, loss of sensation due to nerve damage, bleeding, ecchymosis, temporomandibular joint (TMJ) problems, tenderness, movement restriction, open bite and crepitus. Thorough clinical examination, however, may be impossible in uncooperative young trauma patients. Sign and symptoms seen in our cases were restriction in mouth opening, derangement of occlusion, temporomandibular joint (TMJ) problems and tenderness.
The management of mandibular body fractures in children differs from that of adults due to concern for mandible growth and dentition development.5 The goal of treatment is to restore the underlying bony architecture to its preinjury position in a stable fashion as noninvasively as possible with minimal residual esthetic and functional impairment.
Treatment of mandibular body fractures in children depends on the fracture type and the stage of skeletal and dental development.4
Greenstick fractures without displacement and malocclusion are managed merely by close observation, a liquid-to-soft diet, avoidance of physical activities (e.g. sports) and analgesics.3,6
For greenstick/minimally displaced fractures, conservative closed reduction is the most frequently recommended treatment. The closed reduction and immobilization approach can be achieved by means of lingual acrylic splints, circumferential wiring, arch bars, or gunning splints.7
Intermaxillary types of fixation (IMF) including arch-bars or eyelets are splinting devices for the closed reduction of mandibular body fractures in young children.2,4,5 Precarious dental stability is characteristic of the mixed dentition period. Attrition of deciduous teeth further compounded by resorption of roots results in quite a loose anchorage system.4,5 Partially erupted secondary teeth are not yet sufficiently stable in the pediatric soft bone.4 IMF can cause avulsion of the primary teeth which are not sufficiently stable due to the pressure exerted. Furthermore, the conical shape of the primary teeth, with their wide cervical margins and tapered occlusal surface, makes the placement of these IMF devices or eyelets technically challenging.3,8 IMF was also found to restrict normal dietary intake in children resulting in significant weight and protein loss, reduced tidal volume and increases the risk of aspiration of gastric contents should the patient vomit.4 The wires are uncomfortable and may cause damage to the periodontal tissues.9 However, some authors have indicated that IMF using arch bars is safe in children, especially those older than 9 or even 11 years.8
Several studies have recommended the use of prefabricated acrylic splints as a treatment for pediatric mandibular fractures. These splints are more reliable than open reduction or IMF techniques with regard to cost effectiveness, ease of application and removal, reduced operation time, maximum stability during healing period, minimal trauma for adjacent anatomic structures and comfort for young patients.6 Laster et al.7 described a new treatment modality based on nickel-titanium (NiTi) staples which are inserted in a relatively non-invasive and pain-free manner, and their eventual removal, if required, is as quick as their insertion, facilitated by the fact that the staples are not osseointegrated. Other studies have recommended the use of orthodontic components for the treatment of facial fractures: (i) modified orthodontic brackets have been used for maxillomandibular fixation,10 (ii) orthodontic resin has been used for fixation of mandibular fractures in children,9 (iii) orthodontic rubber elastics were used in combination with fixed orthodontic brackets to create compressive horizontal force marginally over the mandibular fracture site from one side to the other11 and (iv) a modified orthodontic splint appliance has been applied to fractures where two orthodontic bands are fit on the primary second molars with rounded stainless steel arch wires soldered to them on the buccal and lingual side.12
Today, open reduction and rigid internal fixation (ORIF) has become the standard of care for management of displaced fractures.3 Mandibular fractures are often substantially displaced, and thus a low-damage, open reduction treatment strategy would be preferable. ORIF includes micro or miniplates or biodegradable devices, which significantly increase the therapy-related risks previously mentioned. Nonetheless, this technique provides stable three-dimensional reconstruction, promotes primary bone healing, shortens treatment time and eliminates the need for early release of the IMF.
However, the suitability for open reduction in the context of pediatric trauma remains controversial3 due to the potential effect of implanted hardware on the growth and development of mandible of the growing child. There is also potential damage to primary teeth and permanent tooth germs which may result in disturbance to their normal development and damage to their pulp causing its obliteration. Furthermore, the rigid internal fixation might create artifacts on CT scans or MRI, be visible or palpated through the child's thin skin and cause pain and early or late infection.3 Therefore, the decision to use ORIF in children should be taken with great caution and only if other means of reduction and fixation are not attainable.
Currently, ORIF with resorbable osteosynthesis plates and screws is increasingly being used for children. These biodegradable materials do not interfere with radiodiagnostic techniques due to their radiolucency and they guarantee sufficient rigidity and stability to enable initial bone healing of the mandible, followed by eventual degradation, resorption and elimination from the body.12 The avoidance of secondary implant removal operations reduces the costs and the amount of physical and psychological trauma. However some authors have pointed of possible resorption of bone adjacent to the Plate13 and moreover it is technique sensitive.
Despite the above, the literature advocates conservative management of mandibular body fractures at young ages which also benefits in decreased immobilization time, decreased muscular atrophy and better oral hygiene.11,12 Acrylic splints retained with circummandibular wires is one of the most commonly used conservative treatment in pediatric patient. Conventionally Kelsey fry bone awl is being used for introducing the wire. However we used 16 gauze intravenous cannula stilete instead of bone awl.
It is pretty easy to place the wire with IVCS as compared to bone awl. As no stab incision has to be given the wound created by an IVCS is inconspicuous compared with that created by an awl producing considerably less tissue morbidity and consequently reduced postoperative oedema and swelling. When the awl travels through the tissue, with the wire crimped, the twisted end of the wire causes trauma to the surrounding soft tissue. Repeated use of an awl causes it to lose its sharpness. When using an awl, the crimped wire, which is potentially contaminated by oral fluids, is made to pass around the mandible. When using IVCS the section of wire exposed to the oral cavity never touches the tissue, but the tip of the IVCS is exposed to the oral cavity and enters the tissue. It is disposable, economical and freely available which makes it a suitable substitute to the conventional awl. Moreover in centers where bone awl is not present IVCS could serve as an alternative.
S. Thomas, V. Yuvaraj have also advocated the use of IVCS for the placement of circummandibular wires instead of traditional bone awl because of the above mentioned advantages.14 V. Rattan has suggested the use of double wire instead of one for additional strength and placement of a vertical groove on the buccal aspect of acrylic splint which prevents slippage of wire. He also suggests the use of lumber puncture needle or the spinal needle.15
We had anticipated a possible difficulty of kinking of wire while the IVCS was being traced back along the lower border of the mandible. But no such difficulty was observed with 16 gauze cannula.
Protección de personas y animales. Los autores declaran que los procedimientos seguidos se conformaron a las normas éticas del comité de experimentación humana responsable y de acuerdo con la Asociación Médica Mundial y la Declaración de Helsinki.
Confidencialidad de los datos. Los autores declaran que han seguido los protocolos de su centro de trabajo sobre la publicación de datos de pacientes y que todos los pacientes incluidos en el estudio han recibido información suficiente y han dado su consentimiento informado por escrito para participar en dicho estudio.
Derecho a la privacidad y consentimiento informado. Los autores han obtenido el consentimiento informado de los pacientes y/o sujetos referidos en el artículo. Este documento obra en poder del autor de correspondencia.
Conflict of interest
None.
References
1. James D. Maxillofacial injuries in children. In: Rowe NL, Williams JL, editors. Maxillofacial injuries, vol. I, 2nd ed. India: Churchill Livingstone; 2009. p. 387-403. [ Links ]
2. Tanaka N, Uchide N, Suzuki K, Tashiro T, Tomitsuka K, Kimijima Y, et al. Maxillofacial fractures in children. J Craniofac Surg. 1993;21:289-93. [ Links ]
3. Zimmermann CE, Troulis MJ, Kaban LB. Pediatric facial fractures: recent advances in prevention, diagnosis and management. Int J Oral Maxillofac Surg. 2006;35:2-13. [ Links ]
4. Kaban LB. Diagnosis and treatment of fractures of facial bones in children. J Oral Maxillofac Surg. 1993;51:722-9. [ Links ]
5. Amaratunga NA. Mandibular fractures in children - a study of clinical aspects, treatment needs, and complications. J Oral Maxillofac Surg. 1988;46:637-40. [ Links ]
6. Kocabay C, Atac MS, Oner B, Gungor N. The conservative treatment of pediatric mandibular fracture with prefabricated surgical splint: a case report. Dent Traumatol. 2007;23:247-50. [ Links ]
7. Laster Z, Muska EA, Nagler R. Pediatric mandibular fractures: introduction of a novel therapeutic modality. J Trauma. 2008;64:225-9. [ Links ]
8. Nishioka GJ, Larrabee WF, Murakami CS, Renner GJ. Suspended circummandibular wire fixation for mixed-dentition pediatric mandible fractures. Arch Otolaryngol Head Neck Surg. 1997;123:753-8. [ Links ]
9. Chen CM, Chen YR. Mandibular fractures in children-immediate reduction and fixation with orthodontic resin. Changgeng Yi Xue Za Zhi. 1990;13:39-47. [ Links ]
10. Magennis P, Craven P. Modification of orthodontic brackets for use in intermaxillary fixation. Br J Oral Maxillofac Surg. 1990;28:136-7. [ Links ]
11. Gawelin PJ, Thor AL. Conservative treatment of paediatric mandibular fracture by the use of orthodontic appliance and rubber elastics: report of a case. Dent Traumatol. 2005;21:57-9. [ Links ]
12. Aizenbud D, Emodi O, Rachmiel A. Non-surgical orthodontic splinting of mandibular fracture in a young child: 10-year follow-up. J Oral Maxillofac Surg. 2008;66:575-7. [ Links ]
13. Bali R, Sharma P, Jindal S, Sharma R. Bone resorption after bioresorbable fixation of a fractured paediatric mandible - a case report. Oral Surg. 2011;4:48-50. [ Links ]
14. Thomas S, Yuvaraj V. Atraumatic placement of circummandibular wires: a technical note. Int J Oral Maxillofac Surg. 2010;39:83-5. [ Links ]
15. Rattan V. Letter to the Editor. Int J Oral Maxillofac Surg. 2010;39:841. [ Links ]
![]() Correspondence:
Correspondence:
E-mail address: jasomfs@gmail.com
(J. Singh).
Received: 11 April 2012
Accepted: 31 August 2012