Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Española de Cirugía Oral y Maxilofacial
versão On-line ISSN 2173-9161versão impressa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.42 no.4 Madrid Out./Dez. 2020 Epub 01-Fev-2021
https://dx.doi.org/10.20986/recom.2020.1144/2020
CASE REPORTS
Thrombosis of external jugular vein aneurysm. A case report
1Servicio de Cirugía Oral y Maxilofacial, Hospital Universitario Cruces. Barakaldo, España
2Servicio de Anatomía Patológica, Hospital Universitario Cruces. Barakaldo, España
3Servicio de Radiodiagnóstico, Hospital Universitario Cruces. Barakaldo, España
INTRODUCTION
Venous aneurysms were firstly described by Harris in 19281. S. Kallenberger, surgically performed the first external jugular vein (EJV) phlebectasia in a 8-year-old child2. There is no clear definition towards venous aneurysms, neither of a global consens towards its measurment limits. They can appear in every location, including cervical, thoracic, visceral and in extremities. In the neck are presented as unilateral, soft, painless, non-pulsatile mass which increase with Valsalva maneuver. Diagnosis is based in a correct physical exploration and it is confirmed with non-invasive imaging. They are usually asymptomatic in the cervico-facial territory, of favorable evolution and in spite of surgical complications (rupture, thromboembolism), they are infrequent. There are several reports that describe saccular venous aneurysms that originate silent pulmonary embolisms3. It is important to distinguish this anomaly from other neck pathological entities. It is a rare pathologic entity and based on its shortage of references, the case of an external jugular vein aneurysm (EJV) with thrombosis in a 79 year old woman is reported. We emphazise its clinic course, diagnosis and therapeutic management that will depend on its location.
CASE REPORT
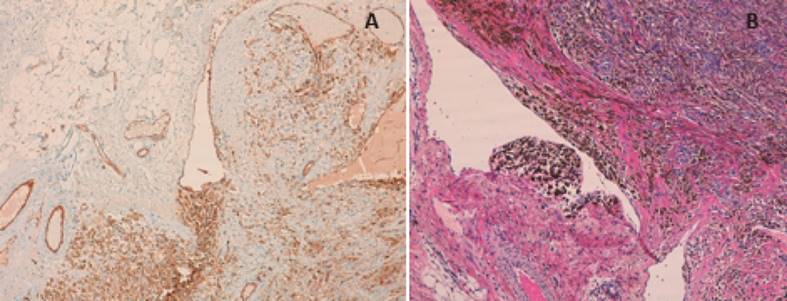
79-year-old patient with medical history of arterial hypertension treated with con Eprosartan and Parkinson's disease treated with Levodopa and Benserazide. Consults for a 4 month-long mass of about 3 cm, without size variation with Valsalva maneuver, soft consistency , non-pulsatile and without deep structure fixation, in the anterior neck triangle. Refers mild intensity and chronic somatic pain. No palpable lymphadenopaties or tumours are identified. Contralateral physical examination is normal. No history of trauma nor of central vein catheterization. Doppler ultrasonography which identifies a 31 x 5 x 44 mm lesion, ovoid, well defined above all hypoechoic (Figure 1) and a Computed Tomography (CT) of supra-aortic trunks is done (Figure 2). After agreeing on a conservative attitude, anticoagulation therapy with Acenocumarol is started. After 3 months, the patient refers new pain episodes and a supra-aortic trunk magnetic resonance angiography (MRA) is requested, which describes a ecstasy-like lesion with a pseudoaneurysm in the right EJV with thrombosis inside and a internal jugular vein (IJV) with normal aspect. Throughout a transverse cervical incision and previous proximal and distal EJV ligature, aneurismectomy is performed (Figura 3). Postoperative elapses without incidents and the patient is finally released after 6 month follow-up. Histopathological diagnosis shows a aneurysmal dilatation with an organized thrombus and recanalization (Figure 4).

Figure 1. Ultrasound image of right laterocervical region. Hypoechoic mass of 3 cm in diameter, superficial to sternocleidomastoid muscle and in relation with EJV can be appreciated without Doppler signal, while EJV has positive signal (arrow).

Figure 2. A-C: Computed Tomography Angiography of supra-aortic trunks showing saccular image in relation with EJV (Arrow). C. Volume Rendering.
DISCUSSION
Venous aneurysm describes an isolated saccular or fusiform dilatation of a vein. Dimensional limits are not well established and authors like McDevitt et al.4 pose to consider a venous aneurysm as such, dilatation has to be double the normal vein diameter. Cervical venous aneurysms are infrequent because of the low pressure that the superior vena cava territory supports and can stand in different cervical regions. In order of frequency they appear in the: IJV, EJV and lastly in the anterior jugular vein1,5,6,7,8. Numerous terms have been employed to describe it: varicocele, venous ecstasy, venous cyst, venous aneurysm and aneurysmatic venous varicosity. EJV aneurysms with thrombosis in adult patients are an infrequent pathology with few cases described in literature.
In pediatric age they are more common in boys, have a fusiform morphology, they are normally located on the right side and recieve the name of phlebectasia(1,5;6,7,8). Phlebectasia though sporadic as it could, can be from congenital origen and thoracic, cervical location6,7. It is present in many overgrowth syndromes such as Klippel-Trenaunay, CLOVES (congenital, lipomatous, overgrowth, vascular malformations, epidermal nevi and spinal/skeletal anomalies), FAVA (Fibroadipose vascular anomaly)9. In adults, they are normally acquired (trauma, inflammation, tumours etc.), they have saccular morphology and locate in the left side due to the compression exerted by an atheroesclerotic aorta on the left innominate vein6,7,8. The etiology of the exposed case could not be identified.
Diagnosis of this entity is basically clinic. Generally, it is based on the presence of a cervical mass, asymptomatic, that increases in size with efforts1,7. Clinic varies with respect to the usual presentation in the presented case: there is no modification with Valsalva maneuvers and continuos pain because of surrounding structures compression is generated.
Within the range of studies to be carried out, Doppler ultrasonography is the method of choice1,3,5,6,7. It allows to differentiate between cystic and solid lesions and establish the origin of the lesion from adjacent structures, it can also differentiate vascular from nonvascular lesions. Complementary imaging studies can be performed to complete its diagnosis like: CT in venous phase, multidetector angiography (MDCT) and MRA1,3. Underline that CT in adult patients should include thoracic and cervical territory to discard a compressive tumour origin. The definitive diagnosis is provided by the microscopic examination of the surgical specimen.
There are some aneurysms of the EJV described1,6,7, but a few of them with thrombosis in its interior. Case reports from literature are analyzed showing, only one, bilateral affection with the presence of thrombosis10. It is important to include EJV aneurysms in the differential diagnosis with lesions like cystic higroma, laryngocele, faringocele, cervical neumocele and with cysts and tumours of the superior mediastinum1,3,5,6. These are easily discarded with the realization of thorax radiography or CT.
Surgical resection is reserved for those cases were the aneurysm has cosmestic implications or presents complications such as thrombosis, spontaneous bleeding or pain1,3,5,6,7,8. Surgical resection consists of vein proximal and distal ligature and total aneurysm excision, so that histopathological diagnosis can be obtained (Figure 4). Conservative treatment with periodical follow-up is reserved for asymptomatic aneurysms3,7,8. Prognosis is favorable and although risk is low, complications like rupture, thrombosis, silent pulmonary embolisms or thrombophlebitis can appear. On the contrary, intraabdominal and inferior extremeties venous aneurysms increase the risk of severe complications.
In conclusion, EJV aneurysm is an unsual pathology, but more exceptional yet if it presents thrombosis in its interior. In spite of that, it is a lesion that should be taken into account while making the differential diagnosis of any neck soft tissue mass. Diagnosis with the help of Doppler ultrasonography is affordable and in symptomatic patients surgical resection is the choice technique.
REFERENCES
1. Çolaklar A, Akkaya H. Saccular aneurysm of the external jugular vein: An unusual case of a neck mass. Oman Med J. 2019;34(5):456-9. DOI: 10.5001/omj.2019.82. [ Links ]
2. Sander S, Elicevik M, Ünal M, Vural Ö. Jugular phlebectasia in children: Is it rare or ignored? J Pediatr Surg. 1999;34(12):1829-32. DOI: 10.1016/s0022-3468(99)90323-8. [ Links ]
3. Parashi H, Rawekar K, Joshi M, Namdev H, Jadhao M, Bohsle K. Saccular aneurysm of external jugular vein with partial trombosis. Asian Cardiovasc Thorac Ann. 2018;26(8):625-7. DOI: 10.1177/0218492316686477 [ Links ]
4. McDevitt DT, Lohr JM, Martin KD, Welling RE, Sampson MG. Bilateral popliteal vein aneurysms. Ann Vasc Surg. 1993;7(3):282-6. DOI: 10.1007/BF02000255. [ Links ]
5. Al-Shaikhi A, Kay S, Laberge J. External jugular venous aneurysm: An unusual cause of a neck mass in a young child. J Pediatr Surg. 2003;38(10):1557-9. DOI: 10.1016/S0022-3468(03)00526-8. [ Links ]
6. Battal B, Dursun E. External jugular vein aneurysm: Clinical and radiologic imaging findings. Int J Otolaryngol. 2011;2011:485293. DOI: 10.1155/2011/485293. [ Links ]
7. Mohanty D, Jain BK, Garg PK, Tandon A. External jugular venous aneurysm: A clinical curiosity. J Nat Sc Biol Med. 2013;4(1):223-5. DOI: 10.4103/0976-9668.107296. [ Links ]
8. Thakur U, Savlania A, Sahu SK, Reddy A. Image diagnosis: Classic external jugular vein aneurysm. Perm J. 2019;23:19.021. DOI: https://doi.org/10.7812/TPP/19.021. [ Links ]
9. Cronenwett J, Johnston K, Rutherford R. Rutherford's Vascular Surgery. 8th ed. Philadelphia: Saunders/Elsevier; 2010. p. 1047-8. [ Links ]
10. Peña Cortés R, Salvador Calvo R, Torres Hernández JA, Lozano Sánchez FS. Bilateral aneurysm of external jugular vein and sequential bilateral thrombosis. Angiología. 2017;69(3):196-7. DOI: 10.1016/j.angio.2016.10.008. [ Links ]
Received: April 15, 2020; Accepted: May 02, 2020











 texto em
texto em