INTRODUCTION
Metastasis to the oral cavity rarely occurs and constitutes 1 % of all oral cavity malignancies1.
The mandible, particularly the posterior region, is more commonly affected than the maxilla, whereas the gingiva is most frequently involved than the bone2).
The metastatic disease in the oral cavity can manifest itself as tumefaction, pain, exophytic mass, paresthesia and numbness, toothache, dentoalveolar swelling, and loose teeth2.
The male-to-female ratio is almost equal with a ratio of 1:1.1. The mean age of patients is 45 years1 and their primary tumors are different in males and females. Breast, followed by lungs, thyroid, adrenal gland, colon or rectum and genital organs, are the most common in women, whereas in men is the lung, followed by the prostate, kidney, bones, and adrenal gland1,3. The diffusion through Batson's venous system is the principal process of the oral cavity metastasis1.
Overall, the lung is the most usual primary site metastasizing to the jaw, and the most common histologic type is adenocarcinoma4).
CLINICAL CASE
A 64-year-old female presented to our hospital complaining of left mandibular ascending ramus and angle pain and swelling. The pain started 7 months before, without any apparent dental symptom and she noted the swelling in the previous 3 months. Apart from these complaints, she had an history of intermittent hemoptysis during the last month. No oral, pharyngeal or laryngeal lesions were found. At the time of presentation, the patient was in the maintenance phase of treatment for promyelocytic leukemia for the last 6 months.
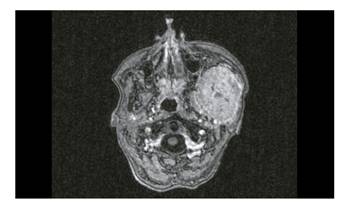
Head and neck Computed Tomography (CT) scan showed an expansive and erosive lesion of the left mandibular ascending ramus with 28 x 16 x 24 mm and central necrosis. (Figure 1 and Figure 2). A biopsy was performed, and the result was a carcinoma of unknown origin. Due to the hemoptysis, the patient did a thoracic, abdominal and pelvic CT scan that reported a 25 mm nodule on the superior segment of the inferior lobe of the right lung, lymphadenopathies of the right hilum and a great trochanter lytic lesion with 43 mm.

Figure 2. CT coronal image from the mandibular metastasis on the left ascending ramus at the time of the biopsy.
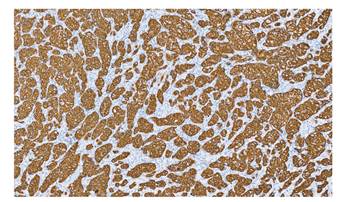
The broncholaringoscopy identified a sessile lesion of the right main bronchus from which a sample was collected for pathology. The histologic result was a primary adenocarcinoma of the lung (AE1/AE3+, CK7+, Cam5,2+, TTF-1) (Figure 3). The patient was staged was a T1cN1M1.
Despite chemotherapy targeting the primary tumor, the mandible metastasis continued to grow (Figure 4), and the patient died from lung cancer disease 8 months after the oral metastasis diagnosis.
DISCUSSION
The diagnosis of metastatic lesions of lung cancer to the jaws could be difficult due to their symptoms that can often mislead the physician to look for oral cancer instead. Although the lung is the most usual primary site metastasizing to the jaw (first in men and third in women), and the most common histologic type is adenocarcinoma4 as the case presented here, this patient lacks the most common symptom present in 90 % of the patients-anesthesia and paraesthesia1. This is related with is location on the ascending ramus instead of the body of the mandible, the most usual location.
The diagnosis of a metastatic lesion was the first indication of a malignancy in 27.6 % at Irani et al, but since metastatic disease to the oral cavity constitutes only 1 % of all oral cavity malignancies, this type of tumor's first presentation is a rare occurrence in an oral and maxillofacial surgeon's practice.
Metastatic tumors of the oral cavity are a diagnostic challenge has they do not exhibit a pathognomonic radiographic appearance. The majority of jawbone malignancies are osteolytic lesions with ill-defined margins5 and can also be described as destructive, irregular, "moth-eaten" radiolucencies. This radiologic presentation is compatible with the well-known capacity of primary lung and breast tumors (the most common to spread to the jaws) to easily degrade the collagen matrix of bone6. Unfortunately, these characteristics are not helpful in the differential diagnosis with oral cancer invading the bone since the imaging features of both entities are very similar. Certain tumors may induce reactive new bone formation and produce a mixed radiopaque (osteoblastic metastasis) and radiolucent lesion that can be mistaken for a fibro-osseous lesion. This pattern is characteristically seen with metastatic breast and prostate carcinomas7. Some metastatic lesions may present the sunburst subtype of periosteal reaction, which are a sign of rapid growing bone pathology. Osteosarcoma, Metastasis (especially from sigmoid colon and rectum), Ewing's sarcoma, Hemangioma, Meningioma, Tuberculosis, Tropical ulcer and rarely Fibrous dysplasia are the differential diagnoses of a sunburst periosteal reaction8.
After the hypothesis of a primary head and neck tumor is excluded, the follow investigation should be guided by the histopathologic findings and the definitive diagnosis is given by the biopsy results. In most cases, metastases to the maxillofacial region have a glandular element; hence, the initial sites of interest to be considered, should be the lung, breast, colon, prostate, and kidney. In our clinical case the biopsy was P40- (a marker for squamous cell differentiation) which led to the glandular element search. All the adenocarcinomas are positive for general glandular epithelial markers cytokeratines as AE1/AE3 and Cam 5,2 but they differ in specific cytokeratins depending on tumor origin. The lung adenocarcinoma is CK7+ as found in our patient's biopsy and in this specific case it was also negative for thyroid transcription factor 1 (TTF-1). TTF-1 is positive in thyroid tumors and in 75 % of the lung adenocarcinomas8. His absence (more common in males) implies a poorer prognosis with worse Eastern Cooperative Oncology Group performance status, greater metastatic burden at primary diagnosis, and more adrenal gland metastases9.
CT scans are often capable of identifying the primary tumor site, and positron electron transmission scanning with fluoro- deoxyglucose is usually used when other imaging modalities fail5.
Lung carcinomas are most often detected in metastatic stage, and the common sites of metastases are brain, bones, and adrenal glands. The pathogenesis of the mandibular metastasis is not fully understood but it is believed that, after the diffusion through Batson's venous system1, the abrupt angulation of the vessels in the mandibular molar and premolar regions causes slowing of the bloodstream which helps malignant cells deposit at this location10.
The treatment depends on the site of origin, the degree of metastatic spread of the primary disease, the age and the overall status of the patient. If the primary tumor was successfully treated and the patient's medical condition permits, the metastatic lesion should be aggressively treated8, including surgical resection and reconstruction. The extent of reconstruction depends on the status of the patient and size of the metastatic tumor with all techniques up for discussion in selected patients.
Unfortunately, oral metastases are usually evidence of a widespread disease and indicate a poor prognosis with reported survival time after oral metastases diagnosis of 3.7-8.25 months2.
With the extensive nature of the metastatic disease, these patients classically have been deemed as nonsurgical candidates. As consequence, the treatment modalities are palliative in most cases. Local treatment with radiotherapy of jaw metastasis is effective in diminishing pain and lesion volume as well as preventing loss of function. For soft tissues metastasis, surgery may be the most suitable approach to obtain the same results4.
Any treatment should be discussed by a multidisciplinary team to give each patient the best quality of life possible.