Introduction
Perinatal mental health research and clinical practice has disproportionately targeted depression (Dennis et al., 2017), despite a significant comorbidity with anxiety (Falah-Hassani et al., 2016). Today, existing data suggest that anxiety across pregnancy is highly prevalent and deserves clinical attention similar to that given to depression. In this sense, in the systematic review and meta-analysis carried out by Dennis et al. (2017) it was found that prevalence of self-report anxiety symptoms was 18.2% in the first-, 19.1% in the second-, and 24.6% in the third trimester of pregnancy. The overall prevalence for anxiety symptoms across the three trimesters was 22.9%. In Spain, Soto-Balbuena et al. (2018) using Spitzer et al.’s (2006) GAD-7, a general anxiety scale, found a prevalence of anxiety during pregnancy of 19.5%, 16.8%, and 17.2% in the first-, second-, and third trimesters, respectively. It should be noted that women may experience specific fears during pregnancy, such as fear of incompetence as mother, pain after birth, loss of own life and the baby’s life, and worries about physical, personal, and marital changes due to pregnancy and birth (Huizink et al., 2004).
The relevance of evaluating perinatal anxiety is due to its comorbidity with depression and its impact on both the mother and her offspring. The presence of anxiety and depression during pregnancy represents a risk factor that increases the chance of developing postpartum depression (Míguez et al., 2017). Furthermore, obstetrically, pregnancy-related anxiety has been associated with premature birth, longer duration of labor, greater probability of using analgesics, and low weight at birth (Dunkel Schetter & Tanner, 2012). Pregnancy-related anxiety has also been associated with consequences such as depression and anxiety in descendants at 14 and 15 years of age (Van den Bergh et al., 2008), and attention deficit and hyperactivity disorder among descendants aged 8 and 9 years (Van den Bergh & Marcoen, 2004).
The adverse outcomes associated with pregnancy-related anxiety demonstrate the need to carry out adequate and specific assessments. However, in both clinical practice and research these specific fears and concerns are not taken into account by general anxiety evaluation scales. One of the most commonly used measures to assess perinatal anxiety is the State-Trait Anxiety Inventory (STAI; Spielberger et al., 1970). As a consequence, they may not detect every woman that actually experiences high levels of anxiety in this period of life. The results derived from the use of general scales could therefore be underestimating its prevalence. On the other hand, they may also include false positive rates due to the ambiguity of some items for pregnant women. That is, some items in general anxiety scales have somatic contents, such as nausea or fatigue, which are common symptoms experienced by many pregnant women, and may lead to misclassification of certain women (Brunton et al., 2015). Likewise, pregnancy-specific anxiety is a robust predictor of birth-related and childhood outcomes, independent of general anxiety measures (Dunkel Schetter & Tanner, 2012; Reck et al., 2013).
Therefore, there is a need to develop valid and reliable tools to screen pregnancy-specific anxiety (Askarizadeh et al., 2017), such as the Pregnancy Related Anxiety Questionnaire (PRAQ). The original version of the PRAQ is made up of 55 items and was developed in The Netherlands (Van den Bergh, 1990). It has been adapted and used in different countries (e.g., Aksoy-Derya et al., 2018; Askarizadeh et al., 2017). Huizink et al. (2004) proposed a reduced version of 10 items with three factors instead of the original five-factor scale, which resulted in a significant loss of information in this regard. In Spain, Vázquez et al. (2018) carried out the adaptation of the PRAQ in its original version. PRAQ shown good psychometric properties and proved to be a valid measurement of pregnancy-specific anxiety. However, despite the utility of this scale, the large number of items of the PRAQ-55 could make the scale difficult to use in clinical practice. Furthermore, the sample was circumscribed to the first trimester of pregnancy and only included nulliparous women. Therefore, the results cannot be generalised to all pregnant women, since pregnant women’s concerns may be different in each trimester and the prevalence of anxiety varies throughout pregnancy (Matthey & Ross-Hamid, 2012).
In view of these data, the aims of the present study were to obtain a brief Spanish version of the PRAQ-55 to be administered to all pregnant women across all trimesters of pregnancy and to assess the instrument’s validity and reliability.
Method
Participants
The study sample consisted of 569 pregnant women who completed the questionnaires in each trimester of their pregnancy. In the first trimester of pregnancy, sample’s age ranged from 18 to 45 years (M = 32.80, SD = 4.75). The majority of the participants were married or lived with their partner (94.9%) and 46.4% of them had university studies. Concerning their employment situation, 75.0% of the sample were employed. Regarding parity, 59.4% were primiparous and 40.6% were multiparous. Pregnancy was planned in 85.9% of cases.
Instruments
Socio-demographic and obstetric-gynaecological questionnaire. An ad hoc questionnaire was built for this study, which included information about socio-demographic variables (e.g., age, marital status, educational level, occupational status, and personal monthly income), previous obstetrical history and current pregnancy (e.g., number of previous pregnancies, planned pregnancy, complications, etc.). Additionally, information about psychopathological disorders and psychological/pharmacological treatment was collected.
Pregnancy Related Anxiety Questionnaire-55 (PRAQ-55; Van den Bergh, 1990). PRAQ-55 is a scale that refers to specific fears and worries related to pregnancy and describes how a woman feels at that moment. The original version consisted of 55 items and seven response options, distributed in five subscales (1: concern for changes in oneself and in relationships; 2: fear for the integrity of the baby; 3: feelings about oneself; 4: fear of childbirth; and 5: concerns about the future and ability as a mother). In the present study, the Spanish version (Vázquez et al., 2018) was used. Nevertheless, in order to facilitate the scale’s clinical usefulness, response options were reduced from 7 to 5. In this way, item responses use a 5-point scale (1 = nothing, 2 = almost nothing, 3 = something, 4 = quite, 5 = much). Therefore, the total score can range from 55 to 275, so that the higher the score, the higher the pregnancy-related anxiety. Based on previous studies (Matthey et al., 2013; Witteveen et al., 2016), PRAQ total score’ 85th percentile was used to identify women with high scores on pregnancy-related anxiety. Finally, this questionnaire was initially created to be used with nulliparous women due to item 35 content, “I am afraid of the labor, because I have never been through it before, I am afraid of the unknown”. To overcome this limitation certain authors removed (Aksoy-Derya et al., 2018; Koelewijn et al., 2017; Westerneng et al., 2015) or modified (Fontein-Kuipers et al., 2015; Huizink et al., 2015; Mudra et al., 2019) this item when evaluating multiparous women. However, studies often use this item without any change in both nulliparous and multiparous women (Askarizadeh et al., 2017; Dubber et al., 2015; Matthey et al., 2013; Van Bussel et al., 2010). In this study, item 35 second part, “because I have never been through it before, I am afraid of the unknown” was removed to facilitate interpretation regardless of parity. In this sample, PRAQ-55 reliability was .97 in first-, second-, and third trimester of pregnancy.
Edinburgh Postnatal Depression Scale (EPDS). EPDS (Cox et al., 1987) is a self-reported questionnaire designed to detect depressive symptoms, asking about how women have been feeling over the past 7 days. This scale includes 10 items with four response choices, each of them having a single value between 0 and 3. The higher the value, the more severe the symptom. The present study used the Spanish version of the EPDS (Vázquez & Míguez, 2019), which showed good internal consistency in first- (α = .81), second- (α = .82), and third trimester (α = .85).
State-Trait Anxiety Inventory (STAI). STAI (Spielberger et al., 1970; Spanish version: TEA, 1982) consists of two self-reported scales to measure two distinct anxiety concepts: state-anxiety and trait-anxiety. Both scales contain 20 statements, rated on a 4-point Likert scale that prompts the respondent to describe how she currently feels (state-anxiety) or how she generally feels (trait-anxiety). For example, the state-anxiety items could be 0 = not at all, 1 = somewhat, 2 = moderately so, 3 = very much so. The total score ranges between 0 and 60, in such a way that the higher the score, the higher the level of anxiety. The cut-off point used for state-anxiety was 32 or more, which corresponds to the 75th percentile to screen high anxiety in women. In this sample, reliability of the state-anxiety scale was .91 in first trimester and .92 in second and third trimesters of pregnancy, respectively. Reliability of the trait-anxiety scale was .88 in first trimester.
Procedure
The sample was recruited in their first trimester of pregnancy in the obstetric control visit to the reference hospital (northwest of Spain). Pregnant women were invited to participate in this longitudinal study which took place from September 2015 to July 2017. Inclusion criteria were the following: being 18 years of age or older, participating voluntarily in the study, and speaking and reading Spanish. From the 620 women evaluated in first trimester, 33 had an early miscarriage, 7 had a preterm birth, and 11 did not want to participate in the study. The study sample was made up of 569 pregnant women with a normal risk status, who completed the questionnaires in all three trimesters of their pregnancy. Participation rate in the study was 91.8%.
Written informed consent was obtained from all subjects. Individual administration of the different questionnaires (paper and pencil) were carried out by one psychologist in first trimester of pregnancy (T1), between 8th and 14th week of pregnancy (M =10.87, SD = 2.36); in second trimester of pregnancy (T2), between 20th and 24th week (M = 20.70, SD = 1.22); and in third trimester of pregnancy (T3), between 32th and 36th week (M = 34.64, SD = 1.26). In each pregnancy trimester, all the questionnaires were provided during routine prenatal appointments. Average evaluation time was 30 minutes in each trimester. Participants did not get any type of incentive for their participation.
This study was reviewed and approved by the Clinical Research Ethics Committee of Galicia, Spain, and has therefore been performed in accordance with the ethical standards laid down in the Declaration of Helsinki 1964 and later amendments.
Statistical and Psychometric Analysis
PRAQ-20 factor structure was examined by means of exploratory (EFA) and confirmatory (CFA) factor analysis using SPSS v22 for Windows and FACTOR v10 program, respectively. Specifically, our shortened 20-item version, the PRAQ-20, was derived from the Spanish version (Vázquez et al., 2018) by retaining items with the highest factor loadings in the three trimesters of pregnancy on each of the five subscales. In this study the criterion used to retain items in each factor was a score > .50 in the factorial load. This procedure was repeated in each trimester of pregnancy with the aim of checking whether the scale’s factor structure remains stable regardless of the time of evaluation of pregnancy-related anxiety. EFA was performed to determine whether the PRAQ-20 shows a similar factor structure in our sample to that found by Vázquez et al. (2018). Particularly, Kaiser-Meyer-Olkin (KMO) test of sampling adequacy and Bartlett’s sphericity test was performed to show the data as suitable. Method for factor extraction was Unweighted Least Squares (ULS) and the criterion for determining the number of factors was the Parallel Analysis (PA). Then, factor analysis was carried out to calculate the rotated principal component matrix using Oblimin method.
CFA was performed to obtain goodness of fit measures. Model fit was assessed using a combination of fit indices: chi-square divided by degrees of freedom (χ2/df), Comparative Fit Index (CFI), Goodness of Fit Index (GFI), Root Mean Square Error of Approximation (RMSEA) and Standardized Root Mean Square Residual (SRMR). When chi-square is divided by its degrees of freedom the result should be less than 6 if it is to indicate a reasonable fit to the data (Kline, 2011). Other fit criteria include CFI and GFI values greater than. 95 are indicative of good model fit (Hu & Bentler, 1999), whereas SRMR values lower than. 08, and RMSEA values lower than. 06 are considered good fitting models (MacCallum et al., 1996).
Additionally, Cronbach’s α was calculated to determine PRAQ-20 internal consistency reliability, and concurrent validity coefficients were calculated using Pearson correlation.
To establish PRAQ cut-off point, scale’s percentiles were calculated. The 85th percentile was used to identify women with high pregnancy-specific anxiety. On the other hand, prevalence of general anxiety assessed with STAI and pregnancy-related anxiety assessed with PRAQ was estimated. Finally, differences between prevalence obtained with each of the anxiety scales were analyzed with the Pearson’s chi-square statistic.
In this research, a p-value <.05 was considered significant.
Results
Construct Validity
The analysis revealed a Kaiser-Meyer-Olkin (KMO) index of .91 in first-, .92 in second-, and. 93 in third trimester of pregnancy, respectively, and a statistically significant Bartlett’s test (< .001).
EFA results for this scale support a model consisting of five factors: factor 1, “concern for changes in oneself”, is made up of items 15, 31, 44; factor 2, “fear for the baby’s integrity”, composed of items 5, 6, 7, 8, 9, 11, 21; factor 3, “feelings about oneself” composed of items 25, 27, 28; factor 4 “fear of childbirth”, made up of items 10, 35, 36, 37; factor 5, “concern about the future”, composed of items 40, 42, 53. The same model is obtained in each trimester of pregnancy with a variance explained of 67.97%, 72.29%, and 72.98%, respectively (Table 1).
Table 1. Structure Matrix Correlations of the CFA and Reliability for the PRAQ-20
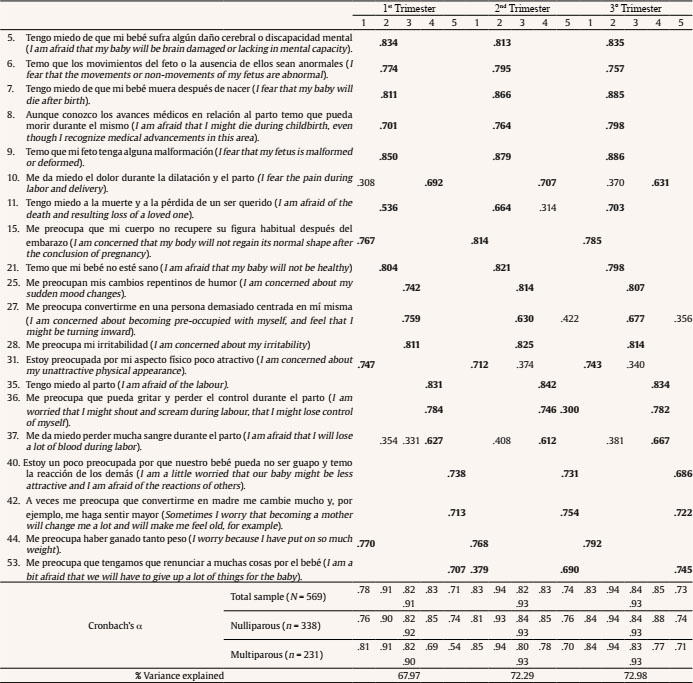
Note. Factor 1 = concern for changes in oneself; factor 2 = fear for the integrity of the baby; factor 3 = feelings about oneself; factor 4 = fear of childbirth; factor 5 = concern about the future.
Values < .30 were deleted.
For data of first trimester of pregnancy, the following fit index values were found after CFA: χ2/df = 0.97, RMSEA = .00, SRMR = .02, GFI = .99, CFI = .99. For data of second and third trimester of pregnancy, the following fit index values were found: χ2/df = 0.97, RMSEA = .0, SRMR = .02, GFI = .99, and CFI = 1.0.
Reliability
In this sample, the reliability of the total PRAQ-20 scale was .91 in first trimester and .93 in second and third trimesters, respectively. Reliability of factors ranged from .71 to .94. Reliability of the total PRAQ-20 scale in nulliparous women was .92 in first trimester and .93 in the second and third trimesters, respectively. Concerning multiparous women, reliability was .90 in first trimester and .93 in second and third trimesters, respectively. Reliability of factors in nulliparous women ranged from .74 to .94 and in multiparous women ranged from .54 to .94 (Table 1).
Concurrent Validity
Table 2 summarizes PRAQ-20 concurrent validity, which was evaluated by correlating PRAQ measures with STAI and EPDS in first-, second-, and third trimester. Correlation between EPDS, state-STAI, and trait-STAI with both total PRAQ and each of the factors ranged from .25 to .47 in first trimester, from .30 to .53 in second- and from .34 to .56 in third trimester, respectively. On the other hand, correlation of different factors among themselves, as well as with the total PRAQ ranged from .29 to .85 in first trimester, from .35 to .88 in second- and from .34 to .88 in third trimester, respectively.
Table 2. Correlations of the PRAQ-20 and EPDS, and STAI by Trimester of Pregnancy

Note. Factor 1 = concern for changes in oneself; factor 2 = fear for the integrity of the baby; factor 3 = feelings about oneself; factor 4 = fear of childbirth; factor 5 = concern about the future.
**p < .001.
On the other hand, Table 3 summarizes the correlation of PRAQ-20 with PRAQ-55 in first-, second-, and third trimester. Correlation between PRAQ-20 and both total PRAQ-55 and each of the factors ranged from .33 to .98 in first trimester, from .40 to .99 in second-, and from .43 to .99 in third trimester, respectively.
Table 3. Correlations of the PRAQ-20 and PRAQ-55 by Trimester of Pregnancy
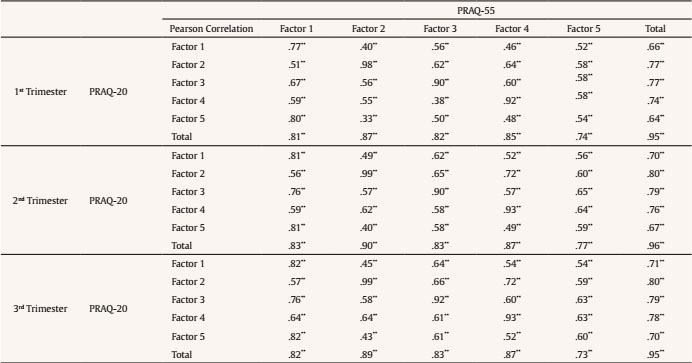
Note. PRAQ-55. Factor 1 = concern for changes in oneself and in relationships; factor 2 = fear for the integrity of the baby; factor 3 = feelings about oneself; factor 4 = fear of childbirth; factor 5 = concerns about the future and ability as a mother.
PRAQ-20. Factor 1 = concern for changes in oneself; factor 2 = fear for the integrity of the baby; factor 3 = feelings about oneself; factor 4 = fear of childbirth; factor 5: concern about the future
**p < .001.
Pregnancy-related Anxiety with PRAQ-55 and PRAQ-20 vs General Anxiety
Average PRAQ-55 scores for each trimester of pregnancy were 122.48 (SD = 41.71), 117.59 (SD = 44.02), and 116.96 (SD = 43.95), respectively. Concerning the PRAQ-20, average scores were 50.66 (SD = 16.76) in first trimester, 47.37 (SD = 17.93) in second trimester, and 44.68 (SD = 18.02) in third trimester. Finally, average STAI scores were 16.96 (SD = 10.25), 14.29 (SD = 9.02), and 15.94 (SD = 9.87), respectively.
Figure 1 shows prevalence of pregnancy-related anxiety with PRAQ-55 considering a cut-off point ≥ 165 and with PRAQ-20 considering a cut-off point ≥ 67. Likewise, prevalence of general anxiety with STAI-state was obtained considering a cut-off point ≥ 32.

Figure 1. Prevalence Pregnancy-specific Anxiety with PRAQ-55 and PRAQ-20 and Prevalence General Anxiety with STAI, in each Trimester of Pregnancy.
Difference in prevalence between pregnancy-related anxiety (PRAQ-55) and general anxiety (STAI) was statistically significant in first- (χ2 = 2.91, p = .004, Cramer’s V = .22), second- (χ2 = 5.62, p < .001, Cramer’s V = .16), and third trimester of pregnancy (χ2 = 3.40, p < .001, Cramer’s V = .27). In particular, prevalence of pregnancy-related anxiety with PRAQ-55 was higher than general anxiety.
Likewise, difference in prevalence between pregnancy-related anxiety (PRAQ-20) and general anxiety (STAI) was statistically significant in first- (χ2 = 3.84, p < .001, Cramer V = .24), second- (χ2 = 5.99, p < .001, Cramer’s V = .17), and third trimester of pregnancy (χ2 = 2.71, p = .006, Cramer’s V = .31). Specifically, prevalence of pregnancy-related anxiety with PRAQ-20 was higher than general anxiety.
Finally, prevalence found between PRAQ-55 and PRAQ-20 was not statistically significant in either first- (χ2 = 0.87, p = .386), second- (χ2 = 0.32, p = .747), or third trimester of pregnancy (χ2 = 0.62, p = .535).
Discussion
A longitudinal study of a large sample of 569 pregnant women was carried out to get a Spanish brief version of PRAQ, as well as to analyse its psychometric properties. The results revealed that PRAQ-20 could be a suitable tool for screening pregnancy-specific anxiety, regardless of parity, in Spanish pregnant women.
Regarding PRAQ-20 construct validity, findings were consistent with results of the Spanish PRAQ-55 version (Vázquez et al., 2018) and the Spanish brief version is also structured across five factors. However, factor 1 lost the second part of its statement “…and in relationships” to better adjust to the items that are finally part of it (15, 31, 44). Similarly, items 40, 42, and 44, which were previously part of factor 1 (Vázquez et al., 2018), now make up factor 5. It should be noted that this same structure remained constant in the three trimesters of pregnancy. After conducting factor analyses, the same structure has been kept as in the Spanish validation of the scale (Vázquez et al., 2018), where only nulliparous women were included. This fact could indicate that the scale behaves the same way with both nulliparous and multiparous women. This would facilitate the usefulness of the scale, since no distinction should be made between both groups of women when administering the questionnaire. On the other hand, correlations between PRAQ-20 and PRAQ-55 were high when comparing same factors (specifically factors 1, 2, 3, and 4) of both scales with each other (ranged from.77 to .99). Correlations were also high when comparing total scores of both scales with each of the factors (ranged from .70 to .96). This data would justify the use of PRAQ-20 as a tool equivalent to PRAQ-55. Concerning factor 5, correlations are lower in all cases (ranging from .54 to .70). This is due to the fact that factor 5 items are not the same in both scales, as most were removed.
On the other hand, CFA supported five-factor scale structure yielded by EFA and goodness of fit measures revealed a good fit of the model. It should be noted that, despite the existence of a smaller version such as PRAQ-10 (Huizink et al., 2004), a version of 20 items was validated due to the fact that in PRAQ-10 all the items of factor 3 (feelings about oneself) and factor 5 (concern about the future) of the original version of 55 items are lost. Therefore, relevant information could have been lost.
In terms of concurrent validity, results obtained show moderate correlations among total PRAQ scale, EPDS, and STAI. Likewise, in terms of anxiety, these data would be consistent with other study (Huizink et al., 2004) which discovered that only about 8-27% of pregnancy-related anxiety variance was explained by general anxiety, concluding that both general and pregnancy-related anxiety should be taken into account as distinct, i.e., complementary and non-exclusive entities. Similarly, accumulating evidence confirmed that pregnancy-related anxiety is a distinct anxiety type (Anderson et al., 2018).
Total PRAQ-20 scale reliability in each trimester of pregnancy was excellent. Likewise, Cronbach’s α of five factors is considered between acceptable and excellent. This shows that it is an instrument that presents good internal consistency, both at general level and in subscales.
In this research, the difference between prevalence found with PRAQ-55 and PRAQ-20 was not statistically significant. Therefore, it could be stated that, despite reduction in the number of items, PRAQ-20 could be valid for identifying women with pregnancy-related anxiety. In this way, it facilitates even more the application of the scale in clinical practice, as it reduces time needed to carry out the evaluation in less than five minutes. On the other hand, statistically significant differences were found between prevalence reported with PRAQ (PRAQ-55 and PRAQ-20) and prevalence obtained with STAI. These results are consistent with those found in the adaptation of PRAQ-55 (Vázquez et al., 2018) and would continue to corroborate two hypotheses proposed by Huizink et al. (2004): on the one hand, data about pregnancy-related anxiety prevalence obtained with general anxiety scales could be underscoring the real number of women with high anxiety levels during pregnancy; on the other hand, it would be confirmed that general anxiety and pregnancy-related anxiety could be different entities.
The prevalence of pregnancy-specific anxiety in this study using the 85th percentile, in both PRAQ-55 and PRAQ-20, ranged from 12.1% to 18.1%. Other authors (Fontein-Kuipers et al., 2015; Koelewijn et al., 2017) found a prevalence of 11% and 30.8%, respectively, although they do not provide data per trimester, only on overall pregnancy. Therefore, they have not taken into account that the trajectory of prevalence of anxiety varies in each trimester of pregnancy. The trajectory of pregnancy-specific anxiety in this study, with both PRAQ-55 and PRAQ-20 questionnaires, decreases from first trimester (16.0% and 18.0%) to third trimester (13.5% and 12.1%). One possible explanation for this downward trajectory could be that specific fears and concerns decrease throughout the weeks of pregnancy because women adapt themselves to their new situation, receive information, and have more knowledge about the entire process of pregnancy and childbirth. In this sense, many women attend maternal education sessions in third trimester aimed to diminish fears and concerns of pregnant women concerning childbirth and postpartum period. As a consequence, participation in maternal education sessions should be encouraged, since it would allow for the detection and implementation of interventions in order to reduce anxiety.
The most important strength of this study is that it is the first to use PRAQ in Spain in a large sample of pregnant women to evaluate pregnancy-related anxiety in each trimester of pregnancy. The reduction in the number of items, as well as the possibility of being used at any time in pregnancy with both nulliparous and multiparous women makes PRAQ-20 a useful scale in daily clinical practice to detect women with pregnancy-specific anxiety versus general anxiety scales. A limitation is that we need to be cautious when considering the cut-off point used, as having a clinical interview would be ideal. Furthermore, discriminant validity of the measure has not been analysed, and all the women from the sample were from the same geographical area in Spain.
The Spanish brief version of the Pregnancy Related Anxiety Questionnaire (PRAQ-20) would be made up of 20 items, divided into five factors, with five response choices, each of them having a single value ranging from 1 to 5. As a consequence, total score can vary between 20 and 100, so the higher the score, the higher the level of pregnancy-specific anxiety. A cut-off point ≥ 67 (85th percentile) was used to detect women with high levels of pregnancy-specific anxiety. Psychometric properties of PRAQ-20 indicate that it could be a useful scale in clinical practice to measure pregnancy-specific anxiety in Spain. Its use during pregnancy would allow for early detection of women with high levels of specific anxiety, thus allowing for implementation of interventions according to women’s needs, which would contribute to improving prenatal care. It would be recommended that all pregnant women are screened for anxiety from the first trimester as part of routine care during pregnancy. Those who score high on several assessments should be referred to mental health services for diagnostic evaluation and treatment if necessary.














