On March 14th, 2020, the Spanish government officially declared the onset of a national lockdown following the health emergency caused by the COVID-19 pandemic (Real Decreto 463/2020). As a result, mobility was strictly restricted to only basic needs, with a prohibition to stay in the street if not under one of these exceptions. This decision was made following an international attempt to control the increasing number of citizens infected by the COVID-19, which was causing the collapse of the whole health care system.
However, there was a sector of population, especially vulnerable to this new health crisis, whose rights as citizens were in a legal limbo. These people were those whose house are the streets, and who had no place to stay and fulfil the lockdown. Thus, throughout Spain, national and regional authorities started to provide emergency shelters for homeless people in order to guarantee their rights as citizens during the current health crisis.
In Madrid, city council authorities (represented by SAMUR Social) in coordination with the Military Emergency Unit (UME), the Spanish Red Cross, and the International Feria of Madrid (IFEMA), proposed the provision of an Emergency Social Service for sheltering those who, for different reasons, were in a homelessness situation, and were thus more vulnerable to the crisis (Tsai & Wilson, 2020). This emergency shelter, with a capacity for 150 people, opened on March 20th, 2020, just six days after the onset of the lockdown, and was located in IFEMA pavilion 14. The service was focused on fulfilling the basic needs of people who were sheltered there, while also monitoring possible health problems that could need specialised medical attention, also providing specialised psychological and social assistance, something that has been already proved as fundamental in these situations (Leung et al., 2008).
The emergency shelter was set up in just 48 hours, an organizational milestone, both in material and human resources terms. In such a short time, 63 auxiliary social care workers were hired. For the service management, their psychological well-being was one of the most important concerns. Scientific literature is rich in examples about the risk of burnout and psychological distress in social care professionals who work with people in a homelessness situation (Lemieux-Cumberlege & Taylor, 2019; Schiff & Lane, 2019). Usually, homeless people bear a hard vital background. Many of them have lived multiple traumas, both before and after becoming homeless (Guillén, et al., 2020; Vázquez et al., 2018) – and a history of abuses, violence, substance addiction, or dual pathology are common too (Calvo et al., 2020). Thus, social care workers assisting the homeless population are frequently exposed both to traumatised people and to their traumatic experiences. It is well known that this secondary exposure may cause what is known as secondary traumatisation or “secondary traumatic stress” (STS; Schiff & Lane, 2019). Also, in the context of the COVID-19 pandemic, there are studies pointing out the impact that being directly exposed to the virus has on the mental health of emergency and health services workers (Greenberg, 2020).
Over the last few years, secondary exposure to traumatic experiences has been effectively related to higher levels of burnout, stress, and depression among workers in the homeless sector (Lemieux-Cumberlege & Taylor, 2019; Schiff & Lane, 2019). Traditionally, burnout has been defined as “a state of physical, emotional, and mental exhaustion that results from long-term involvement in work situations that are emotionally demanding” (Schaufeli & Greenglass, 2001), although Maslach et al. (2001) also take into consideration the depersonalisation and reduced feelings of personal accomplishment likely to appear in burnout workers. Diving into this last concept of personal accomplishment, Stamm (2010) considered that, on a professional level, burnout would be a dual phenomenon, consisting of “compassion satisfaction” and “compassion fatigue”. The former would refer to positive emotions that people have when feeling they are doing their work well. The later would consist of burnout in its classical definition (low-mood, irritability, lack of concentration, frustration, helplessness, and exhaustion) and by STS, which, similarly to Post-traumatic Stress Disorder (PTSD), would be characterised by sleep difficulties, anxiety, fear, intrusive memories, and avoidance (Ludick & Figley, 2017).
As just mentioned, there are two key requirements for considering the presence of burnout: 1) to be under emotionally demanding conditions in the workplace and 2) to have been “long-term” exposed to that demanding and stressful situation. There are reasons to consider that working during the peak of a global pandemic in an emergency shelter for homeless people, when there is very little information and knowledge about the virus, can be regarded as an “emotionally demanding and stressful condition”. However, what about the second requirement? Where do we draw the line of “long-term exposition”? Is one month enough? Maybe six? So far, there are no clear cues in this regard. The World Health Organisation (WHO, 2019) includes “burnout” under the section of “Problems associated with employment or unemployment” in the ICD-11 (code QD85). However, there are no time specifications. Thus, we could take as a reference for how long the existence of symptoms are required to be present in other related mental disorders. Hence, for the diagnosis of a major depressive disorder, the symptoms must be present for at least two weeks; for the diagnosis of PTSD, the symptoms should have lasted for at least one month; for the adjustment disorder, the presence of the symptoms must be of, at least, one month too (WHO, 2019). Taking this information into account and considering the aforementioned lack of scientific specifications for the required length of exposure to a stressful or emotionally demanding situation for regarding the presence of burnout, it could be stated that exposures over a month-length could be regarded as long enough as for developing burnout symptomatology.
In addition to all that has been said about the risk factors for burnout, anxiety, and depression in social care workers in the homeless sector, we should not forget that they were dealing with a completely new situation: working in an emergency shelter for homeless people during a global pandemic, in times of generalised fear and anguish (Dubey et al., 2020). Thus, workers were not only exposed to secondary traumatisation for the said reasons, but also to primary traumatisation, since they were going to assist people who just came from streets, which involved a higher risk of been exposed to COVID-19. There are already many studies showing how frontline health and social care workers during the first wave of the COVID-19 pandemic had higher rates of PTSD, depression, anxiety, and burnout symptoms than average (Luceño-Moreno et al., 2020). However, the authors of this paper have not found any study yet which treats the psychological consequences that working with homeless population during the COVID-19 pandemic may have on the social care workers assisting people in emergency shelters.
This exploratory study tries to make a contribution in this field, studying the percentage of social care professionals working in an emergency service for homeless people during the COVID-19 pandemic who showed clinically significant levels of psychological fatigue, lack of work satisfaction, depression, and/or anxiety. Aiming to know the evolution of these symptoms, the study examined whether there were any significant measurement differences throughout April and May.
Method
Participants
Out of the 63 social care workers who were part of the IFEMA Pabellón 14 staff, 44 took part in the study (we did not care about the reasons of the other 19 social care workers for not taking part in the study, as participation was voluntary). Because of the haste with which the hiring had to be conducted, and taking into consideration that the lockdown had just started a few days earlier, social care workers who were hired were mainly recently graduated students in their 20s (mean age: 27.62 years-old; range: 22-49); 79.37% of them were women.
Their job in the service was to make sure that health requirements were satisfied by the residents (i.e., social-distance, frequent handwashing, use of masks in closed areas, shower area checks, etc.), control of common areas, organisation of social activities with the residents, and supervision of the daily distribution of food and clothes (when laundry was done). Workers wore gloves and facemasks at all times and were provided with working clothes. All workers had several training sessions before and during the duration of their service. The training consisted of health protection, tasks performance, and psychological counselling.
Measurements
For the exploratory study, three questionnaires were used to measure burnout, working satisfaction, depression, and anxiety levels.
Professional Quality of Life, 4th version (ProQoL-IV; Stamm, 2010). This questionnaire was developed to measure the negative and positive effects of helping others who are experiencing psychological pain and/or trauma. The Spanish version of the instrument has been validated, with good psychometric properties (Galiana et al., 2017). The total scale is composed of 30 items organized in a Likert scale with 6 possible responses, ranging from 0 (never) to 5 (always). The ProQoL-IV has three subscales.
Compassion satisfaction. It measures the pleasure a worker may feel from being able to do his/her work well. Higher scores on this scale represent a greater satisfaction related to worker ability to be an effective caregiver in his/her job. Scores below 33 may indicate a satisfaction problem in the workplace.
Burnout. It is associated with feelings of hopelessness and difficulties in dealing with work or in doing it effectively. These negative feelings may reflect the perception that efforts make no difference, or they can be associated with a very high workload or a non-supportive work environment. Higher scores on this scale mean that the worker is at higher risk for burnout (scores over 27).
Compassion fatigue. Also called secondary traumatic stress (STS) and related to vicarious trauma (VT), this subscale measures the psychological impact of secondary exposure to extremely stressful events. The symptoms may include being afraid, having difficulty sleeping, or avoiding things that remind you of the event. Scores above 17 may indicate higher risk of significant compassion fatigue.
Beck Depression Inventory-II Spanish Short-Version (BDI-II; Beck et al., 1996; BDI-II-Short-Version; Sanz, et al., 2005). This short version was composed by the 11 BDI-II items which showed better psychometric properties. All items show four different statements, from lower to higher severity levels for each depressive symptom, of which participant has to choose the one that reflects better his or her state in the last two weeks. Items are scored from 0 to 3. Total scores above 7 indicate clinical depressive symptomatology. In psychometric studies, the BDI-II-Short Version presents adequate internal consistency reliability indices, both for the psychopathological population (Cronbach’s alpha = .83) and for the general population (Cronbach’s alpha = .78) (Sanz et al., 2005).
Beck Anxiety Inventory-Fast Screen, Spanish Short-Version (BAI-FS; Beck et al., 1997; Sanz & García-Vera, 2012). This short version is composed by the 7 BAI items which showed better psychometric properties. Each of the 7 items has to be classified in a Likert scale 0-3, from lower to higher severity levels for each anxiety symptom. Total scores above 5 indicate clinical anxiety symptomatology. The BAI-FS presents good psychometric indices, such as an alpha consistency coefficient of .82 for the general Spanish population (Sanz & García-Vera, 2012).
Procedure
For the current study, we asked for the voluntary participation of the 63 social care workers who were part of the staff. They worked in three different 12 hour-shifts: day, night, and rotating shift. We asked them to fulfil two sets of questionnaires for measuring their burnout, working satisfaction, depression, and anxiety levels.
The first set of questionnaires consisted of the ProQoL-IV, while the second was composed of the BDI-II and the BAI-FS. For the study, there were four measuring times for each set of questionnaires, as follows:
- Set 1 (ProQoL-IV): first week of April, third week of April, first week of May, and third week of May.
- Set 2 (BDI-II; BAI-FS): second week of April, fourth week of April, second week of May, and fourth week of May.
Service psychologists explained the study to all social care workers and invited them to participate. They were told that the study data were confidential and, in any case, their participation would not have any effect (positive or negative) on their job position. Participants who voluntarily took part on the study signed a consent form where all the details of the study were explained and after having answered all the questions they might ask. They were informed that they could decide to abandon the study at any moment without any consequence. Participants then self-filled in the set of questionnaires during the first part of the morning break. One of the two psychologists were with them, in case they needed any support or had any questions while filling the questionnaires.
In order to guarantee participants anonymity, and considering that it was a study with repeated measures, psychologists asked participants to choose a personal secret code for identifying their files, with two letters and four digits, ensuring thus anonymity.
Data Analyses
Data analyses were conducted using the statistical program SPSS 25®. Using G*Power program, it was stated that for a mean-differences test the sample size for achieving an α = .95 had to be of at least 45 participants. Our sample was just one participant below the requirement, so we consider the sample size was good enough. However, the sample results did not follow a normal distribution. Thus, it was necessary to use non-parametric tests for exploring whether there were any differences in the mean score of the questionnaires depending on the measurement moment.
We consider that each measurement time made up an independent measure. We wanted to make an exploratory study about the levels of “work satisfaction”, “burnout”, and “compassion fatigue”, as well as the levels of “depression”, and “anxiety” symptomatology of social care workers in the service. Thus, from our point of view, the importance was not in the individual answers, but in the answers as a whole. Thus, in order to detect any possible statistically significative difference in the mean scores of the symptomatologic questionnaires across the four measurements, we conducted a Mann-Whitney U test, which is a nonparametric test that allows two groups to be compared without making the assumption that values are normally distributed.
Results
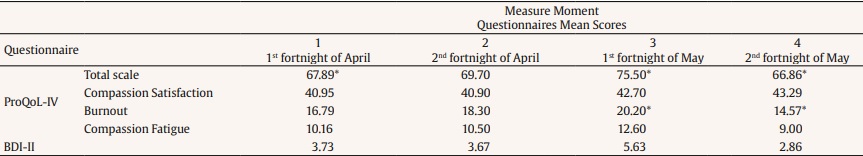
As it can be seen in Table 1, there were almost no statistically significant differences in the measures of the different inventories across time. The scores remained relatively stable across the eight weeks span when working satisfaction, depression, and anxiety symptoms were measured.
However, there are two exceptions. In the ProQoL-IV total scale, there were statistically significant differences between the first and third measures (Z = 0.016) (first week of April and first week of May), when there was an 11% increment in the scores, and between the third and fourth measure (Z = 0.02) (first and third week of May), when there was a 12.45% reduction in the scores. The other statistically significant difference in the measures across time was found in the ProQoL-IV Burnout scale, between the third and fourth measure (Z = 0.03), when there was a 27.15% reduction in the scores. It should be noted that, in all questionnaires, during the third measurement time (first and second week of May) mean scores rose and that, in the fourth measurement time (third and fourth week of May), there was a generalised reduction nonetheless.
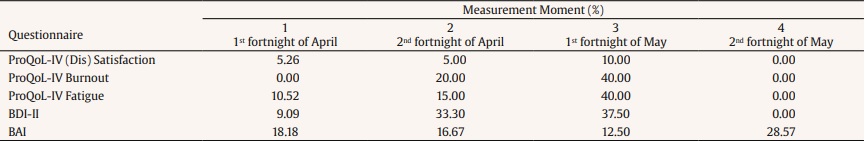
Another important aspect to highlight is that, despite the commented tendencies, in no moment the mean scores were over the cut point which marks the presence of a significant psychopathological symptomatology. In Table 2, the percentage of workers with clinical levels of dissatisfaction (this is an inverse scale), burnout, fatigue, depressive, and anxiety symptoms are shown for each measurement moment. These results are shown in percentages as what we would like to provide is a general picture regarding the psychological well-being of service workers. As Maxwell (2010) claims, for qualitative researchers, it is best not to use numbers for showing results, as they may lead to misinterpretations by the readers.
Discussion
As it was presented in the introduction of this paper, the main goal pursued by the researchers was to conduct an exploratory study about how working in an emergency service for homeless people during an exceptional situation, such as the COVID-19 pandemic, could influence the psychological well-being of the workers. Although there was a steady increase of studies about how health since the beginning of the pandemic and social care workers were psychologically affected by being in the frontline of the fight against the virus (Luceño-Moreno et al., 2020), there was a clear lack of research on how social care workers who worked with homeless people were touched by this exceptional situation.
Thus, the preliminary results from this exploratory study may help get an initial frame about how the current situation for workers in this sector is and which paths should be walked in order to guarantee their best psychological well-being. This is an important point because, as Wright and Cropanzano (2000) pointed out, psychological well-being is one of the main predictors of job performance. It should not be forgotten that homeless people are in a very vulnerable position, even more if we take into account a scenario of global pandemic (Benfer & Wiley, 2020; Tsai & Wilson, 2020).
First thing that should be highlighted is that, overall, there were few variations in mean scores in job satisfaction, depression symptoms, and anxiety levels throughout the two months of measurements. This may indicate that workers were well adapted to their working environment, with no great variations in how they had to face their duties, which may have helped them maintain good levels of psychological well-being. However, it is true that in the third measurement time (first fortnight of May), an increase in burnout, fatigue, depression, and anxiety symptoms can be noticed. It was just during these two weeks when there was a considerable uncertainty about what was going to happen with service residents by the end of the month, as the shelter was about to close, but no reallocation measures for them had already been announced. Residents knew about it, and social care workers were the ones who had to deal with their understandable distress and worry. This may be behind this particular change of tendency.
Another important issue was that at no time mean scores of job satisfaction (measured by the ProQoL-IV), depression or anxiety symptomatology (measured by the BDI-II and the BAI-FS) were above the cut score proposed by its authors as sign of possible clinical problems. This is good news, as it indicates (preliminary) that the psychological well-being of service workers remained at healthy levels. It may indicate that job demands were not high and were well shared and organised between workers, and that workers felt a good working engagement (Tesi et al., 2019). By analysing these results in more detail, we can observe how, on average, workers showed good levels of job satisfaction and low levels of burnout and fatigue, while there was little incidence of depressive or anxiety symptomatology, results which are similar to those found by Luceño-Moreno et al. (2020) in a population of Spanish health practitioners during the COVID-19 crisis. These results are in line with other studies which have found that job satisfaction was linked with lower levels of depression, distress, and psychosomatic disorders (Bakker, 2011).
In addition, an important percentage of social care workers showed significant scores in job dissatisfaction, burnout, fatigue, depression, and anxiety measures. These results are consistent with results found in other studies assessing the psychological impact of the COVID-19 pandemic on Spanish health and emergency workers (although, the majority of these studies used a cross-sectional design). Thus, in these studies, it was detected that between 32.8% and 79.5% of emergency workers showed anxiety symptoms, while between 27.4% and 63.7% displayed depressive symptoms (Berdullas-Saunders et al., 2020; Luceño-Moreno et al., 2020), figures which are also similar to those detected in health practitioners of other countries (Lai et al., 2020). It may indicate that, in spite of the special characteristics of our sample in comparison with the health practitioners who are usually studied (doctors and nurses in a hospital setting), psychological consequences would be alike.
The exception would be the first fortnight of May, but the possible reason behind it has already been explained above. It is also very important to highlight that, at the end of the service, no worker referred significative levels of job-dissatisfaction, burnout, fatigue, or depressive symptomatology. It is true that, in that last fortnight, 28.57% of respondents showed significant levels of anxiety symptomatology. This should be taken into account for future experiences, in order to provide some kind of psychological support and coping strategies during and before the end of the contract, something that has already been proved useful in workers of the homeless sector (Wirth et al., 2019).
This research also reflects the relevance of preventive psychological training and supervision in order to avoid the development of psychological distress and impairment. As it has been explained, overall, an appropriate psychological wellbeing of the social workers in the service was granted. The reasons for it may lie in the different initiatives that were carried out throughout the time that the service was running. As it has been mentioned in the Method section, all workers went through several training workshops before and during the service. These workshops were focused on providing the workers with the necessary tools both from a physical (i.e., how to ensure an adequate protection against the COVID-19 by using gloves and masks and keeping social distance; basic training on self-defence and protection against possible violent behaviours) and psychological (i.e., counselling and discussion sessions, one-to-one sessions at demand, trainings in emotions management) point of view. The importance of this professional support to promote a psychologically safe work environment has already been highlighted by several studies which examined the psychological toll paid by health and emergency workers during the COVID-19 pandemic (Bredicean, 2021; De Kock et al., 2021; Nyashanu et al., 2020).
Thus, it seems vital to keep on implementing this kind of training and support measures for workers in order to grant their psychological wellbeing. In addition, the study results prove how giving information and certainties to workers counter the appearance of distress and emotional discomfort, thus preventing the possible display of more severe psychological problems in the medium-term. As in any other aspect of life, communication should be a must in any working environment, even if what it means to disclose is that there are no clear cues/information (honesty with the worker should always be a priority) yet.
In conclusion, these exploratory results showed how Spanish social care workers were, overall, psychologically well prepared for facing a challenging and exceptional task, such as working in an emergency shelter for homeless people during a global pandemic such as the COVID-19. Due to the small sample size, results should be read with perspective. Although it is a good beginning, the current study should be replicated in the future, including further measures of job satisfaction and post-traumatic stress symptomatology questionnaires. It would also be interesting to replicate the current study using repeated-measures. Thus, there would be an empirical underpinning for drawing conclusions about the evolution of the psychological well-being in the same set of subjects. Finally, in future research, the likely effect of psychological intervention on workers’ work engagement and the development of copying strategies should be studied, by checking how it could affect their psychological well-being.