Loneliness is a phenomenon that is becoming a matter of increasing concern in developed countries. This concern increases interest in its study, especially in large cities with high population density, where more and more resources are being allocated to specific plans to mitigate its effects. Loneliness affects individuals at any age and has particular connotations among older people. The issue of loneliness currently concerns professionals in various fields (health, sociology, etc.) and even political authorities because of the effects of loneliness on individual and social health, on the population's well-being and its relation with social support networks, but it was already a concern in the middle of the last century (Sheldon, 1948). The concept of loneliness is a multidimensional psychological construct that has conventionally been considered as an unpleasant experience caused by the contrast between expectations and a person's real social relationships (De Jong Gierveld, 1987). We start from an unpleasant feeling that is a source of stress, clearly differentiating loneliness from living alone and regardless of whether it may have a positive added value as a component of active aging (Rodríguez-Rodríguez et al., 2017). Certainly, there is no single loneliness but many kinds, and one of them corresponds to loneliness by choice or by a new life situation, but managing its advantages and valuing the independence it produces, which is considered as a strength for the elderly. In fact, the Active Aging Index (promoted by the UNECE - United Nations Economic Commission for Europe), which is calculated from a series of components, considers living independently as a positive factor, either alone or with a partner (UNECE, 2019). Therefore, a distinction has been made between loneliness and feeling of isolation, highlighting the circumstances of living alone and an extreme social isolation (Smith & Victor, 2019). Loneliness can also be found at other levels: latent solitude, common in those people who do not have satisfactory social and affective relationships and who behave similarly as people who feel alone, but do not manifest the feeling of solitude; there is also a desired solitude, an indifferent solitude, and an unwanted solitude. The latter is the one we are going to refer to hereafter on, and it is the one that has drawn most studies’ attention. We will use terminology such as loneliness and unwanted solitude indistinctly.
Loneliness has been associated with a large number of organic and psychological disorders. It is mainly associated with pathologies related to hypothalamic-pituitary-adrenal axis, hyperstimulation, cardiovascular risk, high blood pressure, high cholesterol, sleep disorders, migraine, immune function, effects on transcription of some genes, etc. (Christiansen et al., 2016; Hawkley & Cacioppo, 2010). Not only is it associated with increased morbidity, it has also been associated with increased risk of mortality (Holt-Lunstad et al., 2015). Cognitive aspects have also been widely studied and are considered a risk factor for cognitive impairment and dementia (Boss et al., 2015). Regarding mental health, it has been associated with depression, anxiety, low self-esteem, emotional instability, negative thoughts about oneself, etc.; it has also been associated with certain personality traits, such as shyness, reduced sociability, or avoidance behaviors (Ausín et al., 2017; Cacioppo et al., 2010; Martín-María et al., 2020). Also, the neurobiological basis of isolation has been studied to contribute to its global understanding (Bzdok & Dunbar, 2020).
Drawing on the literature review, we conclude that loneliness is a multidimensional construct associated with multiple variables. These variables are objective (physical health, sociodemographic variables such as living alone, etc.) and subjective (that is, subjectively assessed, such as mental health, especially depression and anxiety, perception of health and quality of life, etc.), hence the importance of assessing all these variables to study their association with loneliness among the elderly.
One problem that arises concerns is how to assess and measure loneliness. It can be done with scales or structured questionnaires or with some questions. There are several scales, among them Jong Gierveld Scale (De Jong Gierveld & Van Tilburg, 2006) and ESTE Scales of social loneliness (Rubio & Aleixandre, 1999). In population-based studies, the basic assessment is made with one or more direct questions that usually include “Do you live alone?” and “Are you feeling or have you felt alone?”. The correspondence between these types of questions and the validated scales has been the subject of studies with mixed results (Victor, Grenade et al., 2005).
In Spain, several important studies or surveys on loneliness have been carried out, some of them population-based, among them Ausín et al., (2017), Losada et al., (2012), and Martín-María et al., (2020). The present study is included in these epidemiological cross-sectional studies with a representative sample of the population.
The aim of this study is to describe the situation of loneliness in the elderly through a transversal population study and to analyze the relationships with different variables of mental health, diseases, pain, and health perception.
Based on previous studies, we start from the hypothesis that the feeling of loneliness is a multidimensional construct associated with objective and subjective variables. In the first place, we propose that variables related to mental health and quality of life are associated with the feeling of loneliness in the elderly. Secondly, we expect to find an association between loneliness and physical health variables, although, given the subjective component of loneliness, these will have less weight in explaining the feeling of loneliness.
Method
Sample
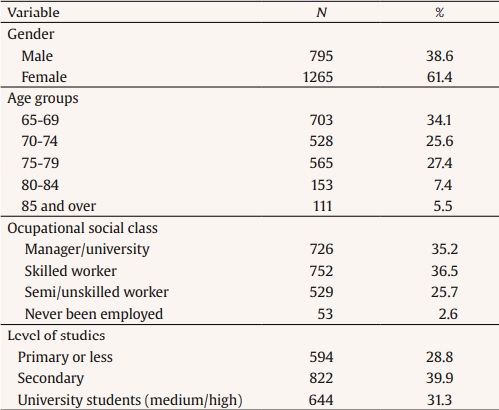
The present research is a transversal, descriptive, epidemiological study with an analytical approach. The sample was taken from the Health Study of the City of Madrid, 2017. Based on the census, a stratified random sampling was made according to the districts of the city with a probability sampling by age and sex. Total N of the study was 9,676, of which 8,845 were full interviews and 831 were unfinished interviews. They were conducted to people from 15 to 98 years old. In the present study of loneliness, data were taken from respondents over 65 years of age. The sample includes 2,060 people aged between 65 and 98 years old.
Procedure and Instruments
The survey was carried out on the telephone. A structured questionnaire with closed-ended questions was used. Most of the questions required yes/no responses; when they were open questions, questions with yes/no answers were asked until all the possible answer options were included. The survey and its protocols were approved by the Carlos III Health Institute Ethics Committee (No. CEI PI 51-2017-v2). At the beginning of the interview, participants received information regarding the origin of the interview, the objectives and other aspects related to the study and they were informed that the data was confidential and anonymized, making their identification impossible; they voluntarily participated when they consented. Interviewers were personnel trained for this task by professionals.
In the field of health, direct questions were asked about illnesses suffered, consumption of various types of drugs, and health-related issues such as disability, sleep, attendance at health services, pain, alcohol consumption, etc. The 12-item Goldberg General Health Questionnaire was also applied. There are versions of 60, 30, 28, 20, and 12 items, and it is a recommended instrument to be used in health surveys (McDoweel, 2006). This questionnaire has been used in Primary Care and in epidemiological studies with the general population as a screening test of non-psychotic mental health pathology (symptoms of depression, stress, suicidal ideation, coping, etc). It can be administered using a Likert scale (with 4 options, range 0-48) and a score of two categories (0-0-1-1) (range 0-12); its use as a scalar variable presents a cut-off point (3/4) indicating probable case/no case (Bones-Rocha et al., 2010); the 12-item version presents, when used as a screening for mental pathology, a sensitivity of 83.4% and a specificity of 76.3% (Goldberg et al., 1997). In the Spanish population (Rocha et al., 2011) the internal consistency of the instrument has a Cronbach's alpha of .90; in the factor analysis (KMO = .93) the variance explained by a single factor is 73%, so it can be used as a one-dimensional scale, and 89% in the three-factor model; several authors have shown the multidimensionality of the GHQ. In this sample, Cronbach's alpha is .792; Hotelling's T square, F = 475.53, p < .001; Spearman-Brown coefficient is .813; Gutman's coefficient .810.
To measure Health Related Quality of Life (HRQOL) the COOP-Wonca was used (Wonca Classification Committee, 1990). The COOP-Wonca is a 5-point response scale, with 1 representing the best and 5 representing the worst level of functioning (range 9-45). It is used face to face as a regular questionnaire with verbal stimuli or through charts that exemplify the various items, and it can also be self-administered. It includes questions about fitness, feelings, daily and social activities, health and changes in health, pain, etc. It is used in population studies, but also in primary care; we used the 9-item version and the adaptation of Lizán and Reig (1999). These authors find that Cronbach's alpha coefficient is .82; Gutman's coefficient is .82, and the corrected Spearman-Brown coefficient is .82; test-retest reliability at two weeks varied between .52 and .72 for the 9 questions; in subjects who did not experience changes this reliability was between .66 and .81; in factor analysis they only found one factor. A psychometric study of administration was carried out on the telephone (Pedrero-Pérez & Díaz-Olalla, 2016); the internal consistency was .93 and factor analysis found a single factor that explained 78.8% of variance. Since the survey was conducted by telephone, it was not possible to use the charts, so the contents of each item were converted into verbal stimuli in the same way as responses. In this sample, Cronbach's alpha is .750, and Hotelling's T squared, F = 1935.86, p < .001. Spearman-Brown coefficient is .738 and Gutman's coefficient is .736.
To evaluate the presence of diseases, including depression and anxiety, questions such as “Has your doctor told you that you have the disease?” were asked, this mode of survey being frequent in population-based studies (Comijs et al., 2002). Objective cognitive performance was studied with five questions about time orientation (TO): day of the week, day of the month, current month, current season, and current year. In this sample, Cronbach's alpha is .978, and Hotelling's T square, F = 31.399 (p < .001), intraclass correlation = .899 (IC = .890, .908); Spearman-Brown coefficient is .966; Gutman's coefficient is .941. In factor analysis (KMO = .885) the variance explained by a single factor is 92.09%, hence it can be used as a one-dimensional scale.
These questions were taken from Mini Mental State Examination (Folstein et al., 1975) and a variable was constructed with them, i.e, the number of failures from each of the subjects, and it also assesses the objective memory performance (Sweet et al., 1999). Memory complaints answer the question “¿Do you have memory problems?”. Subjective cognitive decline (SCD) was assessed with 7 questions of a scale constructed for the purpose of the survey, taking into account the SCD criteria (Jessen et al., 2014); however, in the current article these questions were used independently of each other, and the scale was not employed.
Regarding loneliness, several specific questions were asked: “Do you live alone?”, with answers Yes/No; “Have you felt lonely in the last year?”, with answers always, almost always, quite a few times, rarely, never or almost never; and “How many people do you live with?”.
Data Analysis
The statistical analysis was performed with the SPSS program (IBM SPSS Statistics for Windows, v. 20.0. Armonk, NY, IBM Corp.). The dependent variable was “feeling lonely” or loneliness. Throughout most of the analysis, the feeling of loneliness variable was categorized in a dichotomous way Yes/No (Yes: always, almost always, and quite a few times; No: rarely, never, and almost never). Categorical variables were coded so that the highest number always indicated the greatest burden or pathology. Thirty-six variables were studied, in addition to the epidemiological ones, in relation to solitude; all of them were grouped a priori in 5 blocks (see Table 2), to analyze which of the variables in each group had a higher predictive value. To study the association between the dependent variable and the independent variables, according to whether they are categorical or scalar, we used ANOVA, with η2 effect size, contingency tables with Cramer's V statistic for the effect size (when both variables were categorical), and Pearson's correlation coefficient (r). For the predictor study, logistic regression was used with odds ratio (OR) and its confidence interval (CI), the -2log likelihood as the model's statistic of fit and the Nagelkerke's R2 (a correction of Cox and Snell's R2) to show the explained variance. The effect sizes were interpreted according to the following criteria: Cramer's V, .10 = small effect, .30 = medium effect, .50 = large effect, ANOVA, η2, = .01 = small effect, .06 = medium effect, .14 = large effect, multiple regression, R2, .02 small effect, .13 = medium effect, and .26 = large effect (Cohen, 1988).
Most of the questions were administered to the entire sample, although some variables included non-responding participants and were considered “missing” data. The question “do you have memory problems?” was asked to 49.5% of the sample and, of these participants, those who answered “yes” were administered the rest of the cognitive complaint's questions.
Results
General Data
In Table 1 we can see the main epidemiological data of the sample. The age range is 65-98 years, mean age = 73.26 (DT = 6.19). We can see that 9.24% of the entire older population feels lonely; 27.5% of them live alone, of whom 19.7% report feeling lonely, and 5.3% report feeling lonely despite living with others. There is an association between feeling lonely and living alone (χ2 = 100.99, p < .001, Cramer's V = .22).
Loneliness and Health Variables
In Table 2 we present bivariate relationships between loneliness and each of the health variables, with corresponding statistics and effect size.
Table 2. Association among Dependent (loneliness) and Independent Variables

Note. Cramer's V and η2 = effect size.
Feeling of loneliness is associated with all the mental health-related variables, especially with depression (32.5% of people reporting depression refer feeling lonely) and chronic anxiety (30.9% of them feel lonely). The frequency of self-reported depression in the study is 11.2%. Subjects who live alone reported suffering from depression more frequently (14%) compared to subject who do not live alone (10.2%) (χ2 = 5.90, p = .015; V = .05). Loneliness is also significantly associated with quality of life, perception of health status, and other health-related variables (including some chronic diseases). With regard to the HRQL items (COOP-Wonca), among those who show a much worse quality of life the percentage of reported loneliness is higher, and this happens for all questions, with those who say that “their life has been much worse” (54% report loneliness) standing out against those who say, in the same item, that “they have done very well” (2.8% report loneliness), as well as those with limitations in their social activities (52% report loneliness) against those who show no limitations (6.8% report loneliness).
Among those who perceive their health as very bad, 30.4% feel lonely, compared to 3.4% of those who perceive it as very good. With regard to multi-morbidity, the percentage of loneliness of those persons who do not suffer from any disease is well below the average (4.5%); among those who suffer from more than two diseases, the percentage of people reporting loneliness is 13.6%. The alteration that is associated with the highest percentage of loneliness is impaired vision and a hearing difficulty that prevents them from carrying out their usual tasks; among these, 20.1% feel loneliness, as opposed to only 7.5% of those who do not have such difficulties; of those with a hearing impairment, 17.2% feel loneliness, as opposed to 8.3% of those who hear well. We observe that all associations between loneliness and every type of pain are significant. Of those respondents who feel lonely, 22.6% take pain medication, compared to 10.2% of those who do not feel loneliness. The variable with the higher effect size is non-localized pain (yes/no), 44.1% of the sample of older people feel this type of pain; 15.1% among those who feel this pain feel alone, while the percentage of loneliness of those who do not feel pain is 4.6%.
People who feel lonely have a worse cognitive performance: among those who do not have problems of time orientation, 7.1% feel loneliness, while it rises to 17.4% among those who have three or more cognitive-related failures. Among people who live alone, 19.7% refer to have memory problems and, of these, 14.5% feel lonely, while the percentage of loneliness of those respondents who do not report memory problems is 6.6%.
Predictors of Loneliness: Cognitive Performance and Mental and Physical Health
In the multivariate study we analyzed loneliness in relation to the diverse blocks of variables that have been exposed in Table 2. We carried out a logistic regression (forward conditional method) within each group. The dependent variable was loneliness (Yes/No). The possible predictors were the variables in each block that had been significant in the bivariate study. In Table 3, we show the variables that are significant with their OR and confidence interval and the variables of the same block which are not significant.
Table 3. Predictors of Loneliness. Logistic Regression

Note. OR = odds ratio; CI = confidence interval; R2 = effect size.
In the cognitive performance block (χ2 of the final model = 5.46, p = .02, Nagelkerke's R2 = .05) the only significant variable is “memory problems affect daily life”; this variable had the largest effect size in the bivariate study. Regarding mental health block (χ2 = 270.95, p < .001, R2 = .27), the variable that first enters in the model is general mental health (GHQ-12) with an effect size of R2 = .24, followed by the variable depression which adds .02; it should be noted that the biserial correlation between both of them is r = .45 (p < .001). All mental health variables are significantly correlated between them: anxiety and taking tranquilizers, r = .27; anxiety and taking antidepressants, r = .38; depression and taking antidepressants, r = .58; and anxiety and depression, r = .44; depression and taking tranquilizers, r = .26; for all correlations p < .001. In the block of disease and HRQOL (χ2 = 162.97, p < .001, R2 = .17) this variable has the largest effect size (R2 = .16). The association between quality of life and perception of health status is significant (F = 310.24, p < .001, R2 = .38), as well as having some chronic disease (F = 179.95, p < .001, R2 = .08); the correlation with multiborbidity is significant as well (r = .43, p < .001). Among the pain variables (χ2 = 88.765, p < .001, R2 = .09), the one with the largest predictive effect size is general pain with an R2 = .07; the other two variables that enter in the regression equation, arthritis/osteoarthritis and taking strong pain medications add very little to the prediction. Among the specific diseases (χ2 = 74.273, p < .001, R2 = .08), those with the greatest effect size are those directly involved in the relationship with others, alterations in seeing (R2 = .04) and in hearing, which adds an R2 = .01; among those who have significant difficulties in both directions, 28.3% feel loneliness.
Discussion
We have presented a cross-sectional epidemiological study. We have analyzed factors related to health, both mental and physical, that could be associated with feeling lonely. A first global consideration is that loneliness is a phenomenon that involves many aspects of the life of the elderly and is associated with quality of life, general health, mental health, and physical health. We have tested our first hypothesis: variables related to mental health and quality of life are associated with the feeling of loneliness in the elderly; the second hypothesis is also supported by the fact that effect sizes of mental health and quality of life variables are higher than those of physical health variables.
First data to be highlighted is the percentage of elderly people who feel lonely, which is similar to other studies; Pinquart and Sorensen (2001) in their meta-analysis indicated that figures of loneliness ranged between 5 and 15%; in our country figures of most authors are within these limits with similar socio-epidemiological characteristics (Losada et al., 2012). These percentages have hardly changed over the last 50 years (Dahlberg et al., 2018).
Cognitive Performance and Loneliness
We have analyzed memory complaints and cognitive performance in relation to loneliness. Loneliness, but not living alone, has been associated with lower cognitive performance and even higher prevalence of Alzheimer's disease (Lara et al., 2019) as well as subjective cognitive decline (Montejo et al., 2020). In the bivariate study we have observed that an objective variable associated with loneliness is memory failures (temporal disorientation) and other subjective variables, such as memory complaints, being worse at a cognitive level than other people of the same age, and alterations in daily life due to memory problems; the latter is the only significant one in the multivariate analysis. Therefore, according to our data, memory complaints are predictive of loneliness probably due to its impact on everyday life. In a follow-up study, Donovan et al. (2017) found, on the one hand, that loneliness accelerated cognitive decline regardless of demographics and, on the other hand, that those suffering from cognitive decline are more likely to be lonely. The cause-effect relationship between loneliness, cognitive function, and memory complaints is not clear; it is probably a two-way relationship. Loneliness has been associated with a poor response to stress situations and an increase in cortisol, phenomena linked to a decrease in performance in several cognitive functions (Cacioppo & Hawkley, 2009). At the biological basis, it is the reduction of the dendritic web, alteration in the formation of synapses and cell death, especially in frontal and hippocampal regions, areas related to memory and executive functions (Boss et al., 2015). Besides, loneliness is associated to poor environmental stimuli and, therefore, to less cognitive activity, which can lead in time to repercussions such as alterations in some cognitive areas and, consequently, to disorders in daily life. Finally, depression, which is closely associated with loneliness, could explain the association between loneliness and memory complaints (Conde-Sala et al., 2019). The association between depression and memory complaints in older adults is well documented in the literature (Balash et al., 2013).
Mental Health and Loneliness
Mental health disorders are all associated with loneliness in the bivariate study. In the multivariate study, depression stands out. The frequency of reported depression in our study is within the limits of prevalence of this disease for the Spanish population (Alonso et al., 2004). Our results are in line with most of the authors who link mental health disorders, especially depression, with loneliness (Conde-Sala et al., 2019). Feeling alone was included at the time as one of the symptoms of depression. In an 18-years follow-up study carried out with seniors, de la Torre-Luque et al. (2019) found that loneliness was the strongest predictor of depression and persistence of depression. Cacioppo et al. (2010), also in a longitudinal study, found an association between depression and loneliness regardless of other sociodemographic factors such as living alone, sex, age, etc. For these authors, in most subjects, the various stressors (illness, death, difficulties of various kinds, etc.) would cause loneliness that would, in turn, act as a serious risk factor for depression. However, once depression has been established, loneliness can also be a consequence of it: anhedonia, decreased vitality, low self-esteem, and other depressive symptoms cause the person to withdraw from himself or herself and tend to become lonely. Both conditions share common causes, both psychological and organic. Mitigating loneliness in a depressed person has a twofold purpose: on the one hand, treating depression and, on the other hand, facilitating the opening of the depressed person to his/her closest environment, in this case while fighting loneliness depression is treated.
Physical Health and Loneliness
In the relationship of loneliness and illness variables we observe, according to our data, that it is mainly associated with those that indicate awareness of health (perception of health and HRQOL). Other authors have found similar results (Emerson et al.,, 2018). Various researchers have developed conceptual models through structural equations in which it is observed how physical health and loneliness are mutually determined; some other factors, such as age, personality/mental health, cognition, social support, and contacts specifically via telephone, are predictors of both loneliness and poor physical health (Smith & Victor, 2019). It is also associated with some diseases, especially with difficulties in seeing and hearing, which can lead to social isolation and feelings of loneliness, since they are difficulties involved in the relationship with others and in the integration into the environement (Victor, Scambler et al., 2005). In our results, it is also associated with reported diseases such as cardiovascular disease, hypertension, high cholesterol, heart disease, diabetes, thyroid disease, asthma, and chronic allergy, as well as with multimorbidity and chronic disease. There is an extensive literature that associates loneliness with these diseases and tries to explain how they originate (Christiansen et al., 2016; Hawkley & Cacioppo, 2010). The physiological mechanisms found that may be these associations are fundamentally an alteration of the hypothalamic-pituitary-adrenal axis, with effects on the adrenergic sympathetic activity and increased vascular resistance, changes in immunity and inflammatory activity mediated by the action of glucocorticoids and increased activity of leukocytes and lymphocytes, increased activity of interleukin-6, C-reactive protein and fibrinogen, and increased tumor necrosis factor alpha (Yanguas et al., 2018).
In our results we found that loneliness is associated with all the variables that value pain and, in the multivariate study, pain in general, arthrosis-arthritis pain and taking strong pain medication stand out. People who feel lonely take twice as much strong pain medication as those who do not feel lonely. The association of pain, especially chronic pain, and loneliness can have several origins and is a two-way relationship. Loneliness is a risk factor for chronic pain. Jacobs et al. (2006), in a follow-up study, found that solitude is a predictor of and increases back pain since this type of pain, in large part, would be associated with psychological and social factors. Other researchers (Jaremka et al., 2013) also found that loneliness increases pain, depression, and fatigue in cancer patients, an increase that would be through the reaction to stress and increased cortisol. Our results suggest, as a hypothesis, that people who feel lonely have a more accentuated sensitivity to pain, probably due, on a physiological level, to the alteration of the HPA axis and, on a psychological-behavioral level, to having fewer resources (affective, activities, entertainment, etc., and in general all those provided by relationships with others) to alleviate it. Other authors have studied the hypothesis in the opposite direction: in a longitudinal study, Emerson et al. (2018) found that chronic pain is a risk factor for loneliness, given that the person who feels pain tends to diminish participation and social interactions; these authors indicate that even those older people who, in principle, are not at risk of loneliness (since they live with others, are married, etc.) can suffer it due to pain; for these authors pain predicts loneliness, regardless of mental health factors, and other physical conditions. This last fact would indicate that treating pain adequately can prevent loneliness in the elderly. There are few studies on the physiological mechanism of the association between solitude and physical pain: Eisenberger and Lieberman (2004) carried out an interesting work using functional brain magnetic resonance imaging that relates “social pain” (produced by solitude-exclusion) with “physical pain” and evidencing the activation of the same underlying brain areas (anterior cingulate cortex), as if there were a common alarm system by which social pain increases physical pain and vice versa.
Limitations
The study has the limitations inherent to most studies whose data are obtained by telephone. First, most of the data are self-reported; in adittion, there are individuals who do not want to respond; there are some others who were not at home any of the times they called on them; in these cases the search for a replacement person is also randomized, but this has not been done in the research that concerns us. On the other hand, there are few data and few questions on important issues regarding the characteristics of loneliness, including those related to family and relationships or relevant events that may have been the origin of loneliness. However, it must be taken into account that the objectives/goals of the survey were to describe the factors of a social, economic, health, and lifestyle nature, such as physical exercise, consumption of food, or pets and certain phenomena (employment, noise, use of cell phones, etc.) that affect older adults. It has not been, as we have indicated above, a specific research on loneliness. As a strong point we note that it is a study whose participants have been extracted from the census at random taking into account age, sex, and place of residence, then the sample is representative of the city's population.
Conclusions
Our results indicate that loneliness is a frequent phenomenon in our society and that it needs to be addressed to improve the quality of life of the elderly. Findings of this population study could probably be applied to other cities with similar characteristics in terms of population, level of development, and other similar socio-demographic features. These results also indicate that the majority of the elderly (90%) do not feel alone. Studies such as this show the complexity and the multitude of both physical and psychological variables that are significantly related to loneliness. Furthermore, these relationships are often bi-directional or with a causality that is still not well-defined. Solitude is, therefore, a target to be aimed at from multiple fronts if we want to mitigate it or decrease its frequency. An adequate approach to this complex phenomenon must consider this reality in order to maximize the probability of success or improvement. It is precisely this complexity which, in part, may explain the doubtful effectiveness of numerous interventions aimed at reducing loneliness, as well as the discrepancy (Masi et al., 2011) between the results of researches in this area.