Anxiety disorders are one of the most prevalent conditions among mental disorders in individuals over 65 years old. The studies regarding anxiety disorders in the elderly in Western countries included in the meta-analysis by Volkert et al. (2013) show variable results regarding prevalence, ranging between 2.3% and 8.9%. The most prevalent disorders were specific phobias (current prevalence = 4.52%; lifetime prevalence = 6.66%). Similarly, Cisneros and Ausín (2018) found great variability in the results of 36 studies analyzed over the last 20 years, finding data ranging from 3.6% (Alonso et al., 2004) to 17.2% (Andreas et al., 2017). Older women are at a higher risk of suffering from an anxiety disorder over the past year than men, and there is a negative correlation between age and the prevalence of that anxiety disorder (Canuto et al., 2017). In regard to the prevalence of specific phobia disorder (SPD) among people over 65 years old, a recent study shows a 12-month prevalence of approximately 12% (Ausín et al., 2020). These authors found that women were more than twice as likely to suffer from a specific phobia disorder than men; furthermore, its prevalence decreased with age in both genders. This study reveals the differences among the rates of different types of phobias by gender and age, pointing out that people over 65 years old mostly fear the stimuli related to the natural environment, followed by animals, blood/injection/injuries, and specific situations. In terms of gender differences in types of specific phobia, this study reveals that women are up to seven times more likely to suffer from an animal-specific phobia than men and twice as likely to suffer from one related to the natural environment than men. In addition to this, anxiety disorders worsen the quality of life and level of functioning of people over 65 years old (Ausín et al., 2020; Canuto et al., 2017; Grassi et al., 2020). Concerning SPD, results are found in the same line, where it decreases the level of functioning and negatively affects the quality of life of people over 65 years old (Ausín et al., 2020).
Even though approximately 12% of the older population has SPD, which is a major health problem in this population, current systems of diagnosis (Diagnostic and Statistical Manual of Mental Disorders – DSM-5; International Statistical Classification of Diseases and Related Health Problems – ICD-11) do not indicate differentiated symptoms for SPD in those over 65 or any gender differences, suggesting a series of common diagnostic criteria with the same importance, which perhaps in the elderly population may not represent the full extent of the disorder. Palmer et al. (1997) note that a common problem in the literature is the application of DSM-IV-like criteria developed from studies of younger adults to geriatric samples without regard for the occurrence of atypical symptoms, high occurrence of depressive and medical co-morbidity, and influence of ageing-related psychosocial changes in the clinical picture. Furthermore, clinicians are often forced to make treatment decisions for their elderly patients based on uncontrolled clinical observations or questionable extrapolation of treatment data in younger adults. An open-minded approach unhinged by ‘conventional wisdom’ is warranted. However, different studies report different symptomatology of SPD according to age and gender. For example, Fredrikson et al. (1996) studied the characteristics of SPD in people between the ages of 8 and 70 and found that, overall, 21.2% women and 10.9% men met the criteria for any single specific phobia. Animal phobia had a prevalence of 12.1% in women and 3.3% in men. Point prevalence of situational phobia was 17.4% in women and 8.5% in men. Women, as compared to men, gave higher fear ratings for all objects and situations. Inanimate object fears and phobias were more common in older than younger individuals. Animal fears were more intense in younger than in older individuals. Fear of flying increased, and fear of injections decreased as a function of age in women but not in men. Thus, specific fears and phobias are heterogeneous concerning sex and age distribution. The review carried out by Coelho et al. (2010) regarding specific phobia in older adults can be added to these findings. These authors extract 4 conclusions from their review. First, age-related sensory impairments are common and interfere both with information processing and communication. Second, cohort effects might result in underreporting, through the inability to communicate or recognize anxiety symptoms, misattributing them to physical conditions. Third, medical illnesses create symptoms that might cause, interfere with, or mimic anxiety. Fourth, diagnostic criteria and screening instruments were usually developed using younger samples and are therefore not adapted to the functional and behavioral characteristics of older ones.
These categorical diagnostic classifications presume that symptoms of mental disorders are reflective of underlying diseases and have the potential to obscure important differences between specific symptoms, as well as relationships among symptoms. An alternative approach to these categorical classifications is the perspective of symptom networks in psychopathology proposed by Borsboom (2017). This approach questions the fact that diagnostic criteria within the same mental disorder are independent of each other. Borsboom and Cramer (2013) point out that network analysis allows the identification of “central” symptoms, strongly connected to the other symptoms in the network. The central nodes are the most dangerous because then the probability of that symptom causing the development of other symptoms is high. Networks consist of nodes and edges. Nodes represent the objects of study, and edges represent the connections between them. In psychopathology networks, nodes represent symptoms, and edges represent associations between symptoms (McNally, 2016). Nodes are usually visualized as circles and edges are lines that connect these nodes, and they can represent any conceivable sort of relationship (e.g., [partial] correlations, odds ratios) (Borsboom & Cramer, 2013). To build a network, one first identifies the elements that will function as nodes, e.g., symptoms of major depressive disorder. Second, one determines what kind of relationship is represented by the edges. For example, the relationship can be defined as being a symptom of the same disorder in DSM-5. In this case, any two symptoms that satisfy this relationship are connected. These relationships are coded in an adjacency matrix with all symptoms shown in rows and columns. This matrix is subsequently used as an input for visualizing the network (Borsboom & Cramer, 2013).
To our knowledge, only a few studies have employed network analysis of SPD symptoms (Borsboom & Cramer, 2013; Kendler et al., 2020), and no symptom network analysis studies were found for SPD in the over 65 population.
In terms of symptom networks in SPD in the general population, these authors find a high correlation between avoiding a phobic situation/object and feeling distress over having a specific phobia. Borsboom and Cramer (2013) point out that it is possible that these two symptoms are not directly related but that their association is caused by a third symptom of specific phobia: exposure to the phobic situation/object provokes intense fear, as a result of which a patient avoids that phobic situation/object and feels distressed about the whole situation.
We hypothesize that it is possible to construct different networks based on gender and age in SPD in people over 65. The current study is based on national data from the study on health and well-being of people between 65 and 84 years old in Europe (MentDis_ICF65+ Study), which is a contemporary, nationally representative study of older adults. This study has two aims: (1) to construct SPD networks based on DSM-IV-TR criterion symptoms and (2) to estimate the network structure among SPD symptoms and analyze age and gender-related differences in a sample of people over 65 years old in the Region of Madrid (Spain).
Method
Design
The sample was obtained from the MentDis_ICF65+ Study (Andreas et al., 2013), regarding the health and well-being of people between 65 and 84 years old in Europe. This longitudinal study was conducted across six European cities. The sample was randomly selected from the population over 65 but under 84 years old in Madrid. The 21 districts of Madrid were included, and a random sample of the rural areas was taken.
Participants
A total of 555 people who met the inclusion criteria were interviewed.
Since previous epidemiological studies included few men in the 75-84 age group, it was decided to stratify the sample by age and sex, so that combinations would be well balanced.
This ensured around 130 persons per group, which would allow data analyses to be carried out.
The inclusion criteria of the sample were as follows: between 65 and 84 years of age, Living in Madrid, and able to provide informed consent to participate in the study. The exclusion criteria for the sample were as follows: presenting a severe cognitive impairment after evaluation using a Mini-Mental State Examination (Mini-mental; Folstein et al.,1975) cut-off point of > 18 and having a language barrier preventing an interview.
The study was conducted following the Declaration of Helsinki and the protocol was approved by the Deontological Commission of the Faculty of Psychology of the Complutense University of Madrid, with reference No. 2203201, and the European Commission.
Variables and Instruments
Sociodemographic variables: questions developed ad hoc allowed data collection on age, gender identity, marital status, and educational level.
Evaluation of specific phobia disorder. To evaluate and diagnose SPD, the Composite International Diagnostic Interview for people over 65 years old (CIDI65+) was applied (Wittchen et al., 2014). This standardized diagnostic interview was used to collect the lifetime, 12-month, and current prevalence data of mental disorders among elderly people. Thus, the CIDI65+ yields diagnoses based on the criteria of the DSM-IV-TR classification system (American Psychiatric Association [APA, 2000]). To develop the CIDI65+, the computer-assisted version of the CIDI was used, consisting of standardized questions on symptoms, supplemented by self-assessment checklists included in a required response booklet.
MentDis_ICF65+ version of CIDI65+. It was developed by the study group under the leadership of Wittchen (Wittchen et al., 2014). The process started with introductory training of all project partners to critically review and identify how the format, structure, and content of CIDI can be improved for use by older people. The general principle in the modification process was to maintain the overall content, structure, and standards of the original CIDI as far as possible and to ensure the integrity of all variables used for the diagnostic computer algorithms. Findings seem to suggest that the major modifications implemented, like shortening of questions by breaking them down into subsets, commitment and sensitivity modules consisting of visual aids and dimensional scales to give respondents more time to reconsider and to remember, implementation of optional synonyms for core symptoms, reduction of skip rules and extensions of dimensional measures are feasible, resulting in mostly good reliability estimates in the range of previous reliability findings reported for considerably younger samples (Wittchen et al., 2014). The test-retest reliability of this interview is acceptable for the anxiety disorder (k = .62, range = .30-.78; Wittchen et al., 2014). There are five DSM-5 symptoms (American Psychiatric Association [APA, 2014]) for SPD, and in the DSM-IV-TR there is one: 1) the phobic situation is avoided or endured with intense anxiety or distress (AVOI); 2) marked distress about having the phobia or avoidance/anxious anticipation/distress in the feared situation significantly interferes with the person's life (DISTRESS); 3) exposure to the feared situation almost invariably provokes anxiety, which may take the form of a situationally bound or predisposed panic attack (EXPO); 4) marked and persistent fear that is excessive and unreasonable, cued by the presence or anticipation of a specific object or situation (FEAR); and 5) the person recognizes that this fear is excessive or unreasonable (RECG). The types of specific phobia contemplated by the DSM-IV-TR and the DSM-5 are the same. Differences are found regarding the order of the 7 diagnostic criteria, but the modifications are minimal in their content, although the wording is not exact. The DSM-5 broadens the criterion that fear or anxiety or avoidance typically lasts six or more months, also in people over 18 years old.
Analyses
The frequencies and percentages of the items in the CIDI65+ interview were calculated as descriptive statistics. A test for two proportions (Z-test) was calculated to compare the proportions of each symptom in each variable under study, gender (female, male), and age (65-74 and 75-84 age group).
The analyses have been performed with R statistical software (v.3.5.6) using several packages. The network was estimated using the InsingFit package created by van Borkulo (van Borkulo et al., 2015), which implements a procedure called eLasso. This procedure is an extension of the Lasso procedure that is widely used for continuous data and that imposes a L1 penalty on the estimation of the inverse covariance matrix. ELasso has been shown to work best when the data are binary without generating excessive computational overhead. The eLasso procedure is based on an adaptation to a binary space {0,1} of the Ising model which is widely used in physical sciences and that depends on two parameters βjk (interaction between variables j and k) and τj (threshold of the variable to take the value 1). These parameters β and τ are estimated with logistic regressions in which for each variable both coefficients are calculated as a function of all the other variables in the network. These τ and β coefficients are finally used to represent the nodes and edges of the network. To guarantee the sparsity of the network, a L1 penalty is imposed on these estimated coefficients. This contraction is controlled by a penalty parameter that is chosen, not arbitrarily in this model but based on the extended Bayesian information criterion (EBIC), which has been shown (van Borkulo et al., 2015) to have good metric properties (converges with increasing sample size and has a low false-positive rate). The visualization of networks was carried out with the qgraph package (Epskamp et al., 2012) (gamma = .25). The centrality of each symptom is represented in a table with its raw values and a graph with the standardized values for the statistics of strength, closeness, and betweenness, which are calculated as z-scores.
Estimates of the networks were made independently according to gender (male vs. female) and age (65-74 vs. 75-84). The estimation procedure was the same for all, but to facilitate the visual comparability of the results, the nodes of each group were forced to coincide positively using the layout found for the network with all subjects.
The stability of the network obtained for all subjects was estimated with the botnet package by calculating the stability of the correlations between the edges against the loss of subjects using bootstrapping subsamples. The stability index CS (cor = .70) used by Epskamp et al. (2018) reports the percentage of subsamples that have found a correlation between the original edge and those of the samples equal to or higher than .70 and shows reasonable stability for values equal to or higher than .20.
Results
Characteristics of the Sample
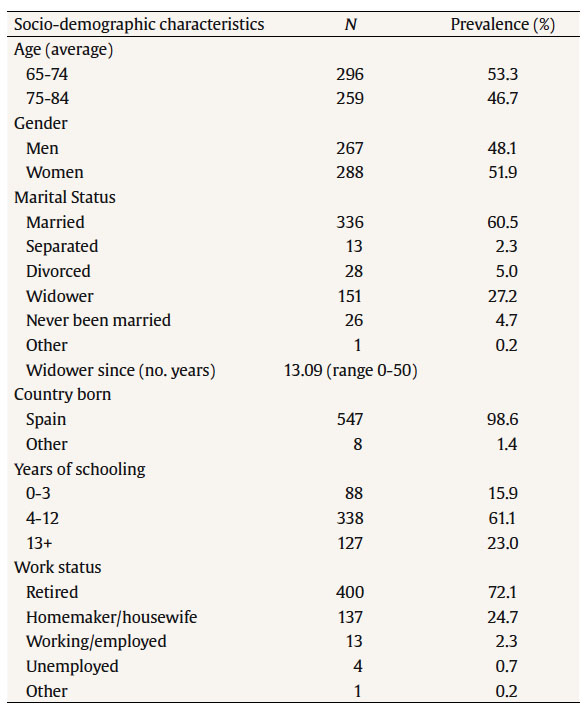
The sample included 555 men and women between 65 and 84 years of age. The mean age was 73.5. Table 1 shows the sociodemographic characteristics of the sample, with the distribution of men and women being consistent with census reports (48% men and 52% women; Instituto Nacional de Estadística [INE, 2020]).
Symptomatology and Differences in Age and Gender
Descriptive statistics with frequencies and percentages of occurrence of each of the phobia types and its symptoms for gender (female, male) and age groups (65-74, 75-84 years) are found in Table 2.
Table 2. Frequencies and Percentages of Symptoms for Gender and Age Variables in Phobia Types

*p < .05,
**p < .01,
***p < .001.
The gender variable presents a greater presence of symptoms in women than in men. For animal phobia, the Z-test showed significant differences for all symptoms, with an average frequency for women of 34.6%, while in men it is only 12.8%; the symptom of greater occurrence for both groups was FEAR (38% and 13% for women and men, respectively) and the least was RECG (19% and 3%). In blood-injection-injury (BII) phobia, no significant differences were found between the two groups, showing very similar percentages in all symptoms. In natural environment phobia, significant differences were detected only for FEAR (30% and 22%) and RECG (14% and 7%) symptoms, being similar for the rest of them. In the situational type, differences were detected for all frequencies except for the RECG symptom. Finally, considering simultaneously all types of phobias (Any Type Phobia) the average frequency of occurrence of a symptom for women was 45.6% while for men it was 29.2%. Significant differences were found in all symptoms, with FEAR being the most frequent for both groups and RECG the least frequent.
In the age variable, the differences in the percentages between the 65-74 and 75-84 age groups are smaller; however, significant differences are found for all the symptoms of the animal type and most of the natural environment type (except RECG). No differences are found for any of the blood-injection-injury type symptoms and for the situational type only the FEAR symptom shows differences. Considering all types of phobias together (Any Type), greater symptomatology can be seen for the younger group, 65-74, with an average percentage of 43.4% compared to 30% for the older group, 75-84.
Gender-based Networks
To facilitate the interpretation of the results, for each phobia type, a single network with all subjects was estimated and its layout was used for all the calculated subgroup networks. The stability statistics were calculated using these networks.
The networks for all types of phobias and their centrality graphs (strength, closeness, and betweenness) calculated for the female (left) and male (right) groups can be seen in Figure 1.

Figure 1. Symptom Networks of Each Type of Phobia by Gender Groups: Female (left) and Male (right). Each node represents an item, and each link represents a relation between each pair of items (bolder lines indicate stronger relations). Centrality indices are represented with blue (female) and red (male)

Figure 1 (cont.). Symptom Networks of Each Type of Phobia by Gender Groups: Female (left) and Male (right). Each node represents an item, and each link represents a relation between each pair of items (bolder lines indicate stronger relations). Centrality indices are represented with blue (female) and red (male)
For all types of phobias, a very similar distribution of centrality can be seen, with FEAR being the most central symptom while the others are peripheral. The exception is the situational type, where the centrality is more distributed, with DIST for women and FEAR for men being the most central symptoms. In the case of the animal type, although the networks are very similar, there is a greater interrelationship between AVOI and EXPO in men, being practically non-existent in women. In the blood-injury-injection type network, the edge RECG-DIST is practically non-existent for men, with the DIST-EXPO and RECG-FEAR relationships appearing frequently. For the natural environment type, both networks are quite similar with the almost total overlapping of the centrality graphics, the most significant difference being in the relationship between EXPO and FEAR, which is strong for the women's group and non-existent in the men's group. For the situational type, the network is completely different from the other phobias. For the women's group, the most central node is DIST interrelating directly with EXPO, FEAR and AVOI while in the case of men the sparsity of the network is greater and can be summarized in the relationship between FEAR and EXPO. Considering all types of phobias together (Any Type), the same star pattern can be seen, with FEAR being the most central symptom. The main difference between the groups is a greater intensity of the FEAR-RECG edge for women and FEAR-AVOI for men.
Age-based Networks
The networks for all types of phobias, and their centrality graphs (strength, closeness, and betweenness) calculated for the 65-74 (left) and 75-84 (right) age groups, can be seen in Figure 2.

Figure 2. Symptom Networks of Each Type of Phobia by Age Groups: 65-74 (left) and 75-84 (right). Each node represents an item, and each link represents a relation between each pair of items (bolder lines indicate stronger relations). Centrality indices are represented with blue (65-74) and red (75-84)

Figure 2 (cont.). Symptom Networks of Each Type of Phobia by Age Groups: 65-74 (left) and 75-84 (right). Each node represents an item, and each link represents a relation between each pair of items (bolder lines indicate stronger relations). Centrality indices are represented with blue (65-74) and red (75-84)
In the graphs, it can be seen how for both age groups the similarity of the interrelations between the symptoms is great, with FEAR as the central symptom. For the animal type, the edge and centrality parameters are almost identical and apply to blood and natural types. Similar to the comparison for gender, the situational type presents a different pattern in which FEAR is not the most central symptom. The most central symptom for the younger group was DIST, while for the older group it was FEAR. It also highlights that the AVOI-FEAR edge is practically non-existent for the 65-74 age group, while it is one of the relevant relationships for the 75-84 age group. Considering all the symptoms together (Any Type), the networks for both groups practically overlap.
Network Stability
The stability of the networks calculated according to the index proposed by Epskamp, CS (cor = .70), for the values of edges intercepts and strength can be found in Table 3. Most of the indices are higher than .20, obtaining in general very acceptable values for network stability with an index average of .40.
Discussion
It was assumed that it was possible to construct different networks based on gender and age in the SPD in people over 65. The results partially confirm our assumption that it is possible to do this, revealing differences in the strength, betweenness and closeness and in the different networks according to gender but not according to age. Although networks of women and men were structurally similar, there are gender differences according to each specific type of phobia, especially in the situational phobia type. The gender variable presents a greater presence of symptoms in women than in men for animal type, natural environment type, situational type, and in all types of phobias (Any Type Phobia) simultaneously. In contrast, no differences were found in the percentages of symptoms according to gender in the blood-injury-injection phobia. For all types of specific phobia, the most frequent symptom for both groups was FEAR (marked and persistent fear that is excessive and unreasonable, cued by the presence or anticipation of a specific object or situation) and the least was RECG (the person recognizes that this fear is excessive or unreasonable). Perhaps the greater presence of SPD symptoms in women than in men could be explained by the cultural aspects and the traditional gender roles assigned to women that encourage a greater societal permissiveness and the ability to express their fears and emotions (Castellanos et al., 2020). Women express their emotions more than men and are more likely to turn to mental health services when they have an anxiety problem (Volkert et al., 2018). However, another possible explanation has to do with the fact that women demonstrate more internalizing coping styles than men.
Concerning the networks developed in terms of gender, for all types of phobias, a very similar distribution of centrality can be seen, with FEAR (marked and persistent fear that is excessive and unreasonable, cued by the presence or anticipation of a specific object or situation) being the most central symptom while the others are peripheral. The main difference between men and women over 65 with SPD occurs in the situational type, where centrality is more distributed, with DIST (marked distress about having the phobia or avoidance/anxious anticipation/distress in the feared situation interferes significantly with the person's life) for women and FEAR (marked and persistent fear that is excessive and unreasonable, cued by the presence or anticipation of a specific object or situation) for men the most central symptoms. For the situational type, the network is completely different from the other phobias. For the women's group, the most central node is DIST (marked distress about having the phobia or avoidance/anxious anticipation/distress in the feared situation interferes significantly with a person's life) interrelating directly with EXPO (exposure to the feared situation almost invariably provokes anxiety, which may take the form of a situationally bound or predisposed panic attack), FEAR (marked and persistent fear that is excessive and unreasonable, cued by the presence or anticipation of a specific object or situation), and AVOI (the phobic situation is avoided or endured with intense anxiety or distress), while in the case of men the sparsity of the network is greater, and can be summarized in the relationship between FEAR (marked and persistent fear that is excessive and unreasonable, cued by the presence or anticipation of a specific object or situation) and EXPO (exposure to the feared situation almost invariably provokes anxiety, which may take the form of a situationally bound or predisposed panic attack). These results are consistent with the results found by Borsboom and Cramer (2013), according to which there is a high correlation between avoiding a phobic situation/object and feeling distress over having a specific phobia. These authors note that it is possible that these two symptoms are not directly related but that their association is caused by a third symptom of specific phobia (exposure to the phobic situation/object provokes intense fear, as a result of which a patient (1) avoids that situation/object and (2) feels distressed about the whole situation. Also, no difference in networks based on gender in SPD was found in a recent study conducted with adults (Kendler et al., 2020), where networks of women and men were structurally similar.
These gender differences can be critical in making a more comprehensive evaluation of the SPD as well as an early and more accurate diagnosis, as this information is not provided through traditional categorical classifications. In this sense, one repercussion in clinical practice relates to the intervention of the situational type phobia. In women, it would presumably be more effective to carry out interventions that prioritize the symptomatology of DIST (with the use of cognitive techniques when there are catastrophic interpretations about the symptoms suffered, and the use of psychophysiological techniques, mindfulness or acceptance and commitment therapy, that reduce the distress about having the phobia), that interrelate directly with EXPO, FEAR, and AVOI, while in men perhaps more useful interventions would focus on addressing EXPO symptomatology (with the use of behavioral exposure techniques, that reduce anxiety through habituation mechanisms).
Concerning age, for both age groups (65-74 and 75-84) there is significant similarity of the interrelations between symptoms, with FEAR (marked and persistent fear that is excessive and unreasonable, cued by the presence or anticipation of a specific object or situation) as the central symptom.
For the animal type, the edge and centrality parameters are almost identical and the same applies to BBI and natural environment types. Nevertheless, the situational type presents a different pattern in which FEAR (marked and persistent fear that is excessive and unreasonable, cued by the presence or anticipation of a specific object or situation) is not the most central symptom, which is DIST (marked distress about having the phobia or avoidance/anxious anticipation/distress in the feared situation interferes significantly with the person's life) for the younger group and FEAR for the older group. It also highlights that the AVOI-FEAR edge is practically non-existent for the 65-74 age group while it is one of the relevant relationships for the 75-84 age group. Considering all the symptoms together (Any Type), the networks for both groups practically overlap. The change in network centrality over time is consistent with longitudinal studies, where it has been found that the centrality of a network can vary over time in major depression disorder (Madhoo & Levine, 2016), though there is no previous data on changes in SPD symptom networks with age. The stability in SPD symptom networks over time, and therefore between the two age groups, could be explained by the stability of the disorder itself. In this regard, Ausín et al. (2020) find that the mean duration of the phobia was approximately 20 years, and that people would adapt to living with this SPD by trying to minimize the interference of these symptoms in their everyday life.
The results obtained in the different networks developed show that the symptomatology of SPD behaves differently in women and men, but not in different age groups in people over 65. Along this line, Price et al. (2018) point out that mental health care should be personalized, looking for the predominant or central symptoms and problems in each patient, as occurs in the clinical formulation of cases. Clinical formulation is essentially a hypothesis about the causes, precipitants, and influences that maintain the psychological and behavioral problems and interpretations of each person (Eells, 2015). It is assumed that the usefulness of clinical formulation goes beyond the global explanation of the case and extends to the organization of complex and sometimes contradictory information, guidance for the planning and direction of treatment, coordination of the intervention team, communication between therapist and client and between professionals, its use as a basis for the assessment of change, as a support for the therapist's understanding of the patient, and, finally, as a re-organizing element of the patient's experience, narratives and identity (Muñoz et al., 2019).
Following the growing need to adopt a dimensional approach to mental disorders, the Hierarchical Taxonomy of Psychopathology (HiTOP) emerges as a dimensional system that constructs psychopathological syndromes and their components/subtypes according to the observed covariation of symptoms, grouping together related symptoms and thus reducing heterogeneity. It also combines co-existing syndromes into spectra, thus mapping comorbidity (Conway et al., 2019; Forbes et al., 2016; Kotov et al., 2017).
On the other hand, McNally (2016) notes that, even though no single method in the field of psychopathology is likely to provide answers to all the questions about the origins and treatment of psychological disorders, network analysis holds promise as both a scientific and practical approach to conceptualizing and guiding treatment of these conditions. Despite the important repercussions at a clinical level that adopting a dimensional perspective of psychopathology can have, Contreras et al. (2019) highlight that the clinical utility of network analysis is still uncertain as there are important limitations on the type of data included, the analytic procedures, and the psychometric and clinical validity of the results. For these authors, it would be premature to defend the fact that central variables found in specific studies should automatically become new intervention targets.
One of the main limitations of the study that we found was related to the representativeness of the sample. In the present study, exclusion criteria were applied for various technical reasons, barring people with a severe cognitive deficit or who could not be interviewed due to some sort of cognitive deficit or nursing home residents, the homeless, non-Spanish speakers, or people over 85 years old. The sample size and sampling method do not allow us to generalize with regard to the entire elderly population of the Region of Madrid, but it does provide a broad view of the situation. On the other hand, the results are based on DSM-IV-TR criteria for SPD and using DSM-5 diagnoses could have led to different results. Since the basic characteristics have remained the same, one would not expect very different prevalence estimates.
Conclusions
The results obtained in the present study seem to support the network analysis perspective, giving greater weight to the centrality of the symptoms in a given disorder as well as the mutual dynamics between them, by showing different network analyses in people over 65 years old according to gender, which reveal the particular SPD characteristics for each group.
The results obtained in the different networks developed show that the symptomatology of SPD behaves differently in women and men, but not in different age groups in people over 65. Although networks of women and men were structurally similar, there are gender differences according to each specific type of phobia, in particular in the situational type. These gender differences can be critical in making a more comprehensive evaluation of SPD as well as an early and more accurate diagnosis.
The network analysis has allowed a more in-depth observation of the characteristics of SPD in elderly people, a population group in which this disorder is often undertreated. These results may be especially interesting for their clinical implications. They may help provide a more accurate diagnosis and lead to more effective interventions that address the most important, different, and characteristic symptoms and mutual relationships according to gender variables.
In summary, these results highlight the importance of considering gender when studying SPD in people over 65 years old, which will facilitate the personalization of treatments offered to this population in healthcare services. However, future research would be needed to develop rigorous analytical methods that allow us to explore the reliability of the networks. In addition, it is important to conduct studies that analyze symptom networks in SPD in different populations, taking into account the gender perspective.