Introduction
A direct consequence of accelerating aging is the greater prevalence of chronic disease, which involves the increased use of medications and highly complex treatments1. Elderly people are at greater risk of adverse drug reactions due to polypharmacy and the physiological changes associated with aging2.
Among the institutionalized elderly there is a high prevalence of cognitive and functional impairment, which, together with structural and organizational issues in the nursing homes, increases the risk of medication errors (ME) and, therefore, the risk of adverse events3-6.
Medical errors can occur from the time of prescription to the time of administration and can have severe consequences in terms of morbidity and mortality in patients and in the use of resources. The majority of these errors are preventable7,8. Administration errors are more difficult to prevent because they arise in the last stage of the medication use process. Therefore, barriers to prevent them should be implemented before the administration stage9.
A safe medication use process and its rational use are needed to prevent adverse drug events in frail populations. Thus, it is relevant to identify and analyse such events and prevent and identify MEs10. The reporting and analysis of MEs and the subsequent implementation of new strategies in the medication use circuit could improve patient outcomes, particularly in nursing homes. In these settings, drug administration is complex5 and is not always performed by qualified nursing staff.
The medications dispensing stage has inherent risks, and dispensing errors (DE) are unavoidable11. DE are frequently identified before they reach the patient, but they sometimes reach the patient causing harm and even death. It is important to study DEs and analyse risk reduction strategies to improve the quality and safety of patient care11.
Pharmaceutical care and medication dispensing in nursing homes are characterized by great diversity. Dispensing could be performed by a Hospital Pharmacy Service, a nursing home Pharmacy Service, or an actual Community Pharmacy in the local area. The task of dispensing should meet minimum standards regardless of the stakeholder involved, be individualized for the patient, be correctly identified, and use a system that makes the caregivers’ work easier while minimizing MEs12.
Automated Dispensing Systems (ADS) increase the efficiency of medication dispensing, and most studies have found that they decrease the number of MEs5,11. Having an associated barcode and being linked to the healthcare centre information system can substantially reduce ME rates13,14. In this regard, pharmacists should choose the best ADS to ensure safety15 based on their knowledge of the medication circuit used and the population served.
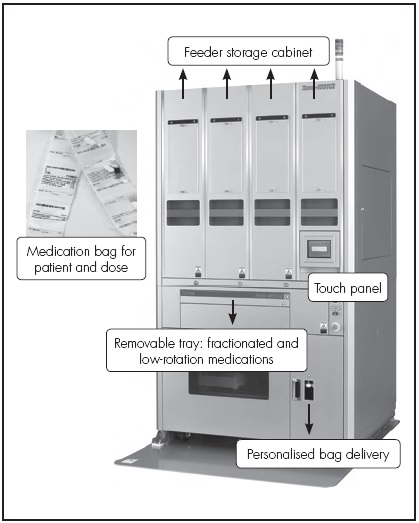
Given that ADS are uncommon in Spanish nursing homes, the present study provides information on the contribution to safety of using the Xana 4001U2 Tosho® Automated Tablet Dispensing and Packaging System (ATDPS) in nursing homes.
Specifically, the objective of this study work was to analyse the incidence and severity of voluntarily reported DEs during medication dispensing in nursing homes using a manual dispensing system of weekly pill boxes compared with the use of an ATDPS.
Methods
A pre-post observational retrospective study that compared DEs in a pre-ATDPS vs ATDPS in 7 geriatric nursing homes. Two other nursing homes to whitch we provide pharmaceutical care service were excluded, because one of them served a non-geriatric population with disabilities, and the other had recently opened.
Scope: The study was conducted in a Hospital Pharmacy Service that provided pharmaceutical care to 9 nursing homes, most of which served geriatric patients. The pharmaceutical care provided included validation of all electronic medical prescription orders, specialized review of complex treatments, dispensation of all medications per patient, follow-up of reported MEs and discussing them with the centre’s team, and training according to specific needs.
Pre-ATDPS Dispensation: The Pharmacy Service dispensed medications in weekly pillboxes that were correctly identified but not prepared by dose, such that nurses could later organize the doses according to a time schedule. This process served as a way to check that the dispensed medicine was correct.
ATDPS Dispensation: The ATDPS was implemented in the pharmacy service in August 2014. We choose a Xana 4001U2 Tosho® ATDPS (Figure 1), which is an automated dispensing cabinet with storage capability using a barcode system, with 400 feeders specifically calibrated for capsules or tablets out of their original packaging. Fractionated or low-rotation tablets are not stored, but are incorporated using a removable tray at the time of dispensing. This system uses an interface between the centre’s electronic prescription software and the ATDPS software to dispense and repackage medication at the required dose and number of doses per patient using polyester film bags (Figure 1). In our Service, the bags are always printed on and, in this study, contained the following information: barcode, patient’s name, location (nursing home and dining room), date and specific time of dose, name of the medications in the bag, their doses, and the total number of tablets/capsules. Given the characteristics of the study population under care, the letter “T” was printed on the bags of patients who needed their medication to be crushed (“triturada” in Spanish) to help administration. This information was obtained using the nursing assessment included in the Electronic Medical Record (EMR).
As a complement to the ATDPS, the Pharmacy Service has an Automated Medicine Detection Machine (AMDM) (Global Factories®, The Hague, The Netherlands) (Figure 2) that verifies the contents of the bags previously created on the ATDPS by reading the barcode and taking a photograph of each bag. Any alarms generated by the AMDM are manually reviewed and, if needed, corrected before the pharmacist validates the dispensing medication. In this way, 100% of the doses dispensed by the ATDPS are checked in the Pharmacy Service.
Any other pharmaceutical form (i.e. liquid, effervescent, buccal, sublingual, inhalers, thermolabile, transdermal, cytotoxic, and injectable products) were dispensed outside the automated system and sent without checking the preparation. Thus, there were two parallel dispensing and administration systems, which we called “blister packaging” and “non-blister packaging”. Dispensing was conducted each week.
Reporting medical errors: In our organization, any health professional can voluntarily report MEs using the EMR. The acting physician follows up the error and is in charge of solving and closing the reported incident. The pharmacist classifies the MEs according to the updated version of the classification system created by the Ruiz-Jarabo 2000 working group. This system classifies MEs by type and location and by severity, ranging from “A = a situation that can potentially lead to an error” to “I = Fatal Error”16. In this classification system, therapeutic nonadherence is included as an ME.
Variables analysed: This study compared information on the nursing home residents in 2013 (pre-ATDPS) with that of the residents in 2015 (ATDPS). The following variables were analysed: sociodemographic variables (age and sex); functional capacity (Barthel index)17; cognitive function measured using the 35-point version of the Mini Mental State Examination (MMSE-35) adapted by Lobo et al.18 and the Global Deterioration Scale/ Functional Assessment Staging (GDS-FAST)19; and pharmacological variables (number of medications, autonomy in the handling of medicines, and need for crushed medication). These variables affected pharmacotherapy and the type of ME. All reported MEs were analysed, except for nonadherence. DE were analysed in greater depth. The frequency of each ME was calculated by dividing the number of reported errors by the number of residents served (expressed as a rate), and by dividing the number of errors by the number of dispensations (expressed as a rate). When the ME was a DE, it was labelled as “an opportunity for DE”.
Statistical analysis: At the descriptive level, sociodemographic, functional capacity, cognitive functioning, and pharmacological variables were analysed according to their frequency, mean, and standard deviation. Differences between the pre-ATDPS and ATDPS groups by age, functional capacity, and cognitive functioning were analysed using the Student t-test for independent samples. The data was analysed using the SPSS v20.0 statistical software package.
Results
In 2013, the Pharmacy Service prepared weekly pill boxes (1,964,685 doses) for 7 nursing homes. These boxes were not checked. In 2015, the Pharmacy Service prepared 742,895 bags (2,222,580 doses), which comprised 63% of the medications dispensed to the same 7 nursing homes.
Table 1 shows the demographic data, functional capacity, and cognitive and pharmacological functioning of the study population for each study period. The results show that during both study periods the residents were similar in age and functionality (P > 0.05), whereas statistically significant differences were found in cognitive functioning between residents who could be measured with the MMSE-35 (P < 0.01). The mean score on the MMSE-35 was higher in the ATDPS group than in the pre-ATDPS group. The typical profile of a person admitted to the nursing home was an elderly person, more commonly a woman, with significant functional impairment (Barthel index) and/or cognitive impairment (MMSE-35) and polypharmacy. A significant number of residents could not be assessed using the MMSE-35, mainly because of severe cognitive deficits (i.e. MMSE-35 scores between 0 and 10), but also because of refusal or behavioural disorders. Therefore, if all the nonassessable residents had been included, the mean MMSE-35 score would have been considerably lower. In total, 15% of the residents had severe or very severe Alzheimer’s disease according to the GDS-FAST scale.
Table 1 Description of the Residential Population Before and After Implementation of the ATDPS

SD, standard deviation; MMSE-35, 35-point version of the Mini Mental State Examination adapted by Lobo et al; GDS-FAST, Global Deterioration Scale-Functional Assessment Staging (Reisberg et al, 1985)
Table 2 shows the MEs reported in each period, with a detailed breakdown of DEs. In 2013 (pre-ATDPS), 408 DEs (1.1 DE/d) were reported. In total, 43 errors reached the patient, 5 of which caused harm. In 2015 (ATDPS), 36 DEs were reported. Of these, 22 involved non-blister packages (non-automated dispensing) (61%) and only 4 involved automated dispensation (11%). In total, 6 errors reached the patients, and of these only 1 required follow-up, although the error did not cause harm. The opportunity for DE was 0.02% in 2013 and 0.0016% in 2015.
Table 2 Analysis of reported errors pre-ATDPS and ATDPS

Error severity C, error reached the patient with no harm; error severity D, error reached the patient with no harm, with follow-up; Error severity E, error reached the patient, caused temporary harm, required intervention; RRR, relative risk reduction; ARR, absolute risk reduction; DE, dispensing errors.
The data show that automation led to a relative reduction of 91% in reported DEs; that is, for every 1000 doses dispensed, there were 0.19 fewer DEs in 2015 (automated system) than in 2013 (pill boxes).
Discussion
The aim of this study was to compare the incidence and severity of reported DEs in the process of dispensing to nursing homes using manual vs mainly automated dispensing. The results indicate that the introduction of an ATDPS significantly decreased (i.e. a relative decrease of 91%) the number of reported DEs, and also decreased the number and severity of DEs that reached the patient. Taking into account that the residents of these nursing homes are at a high risk of medication-related problems, the reduction of DEs and the prevention of DEs reaching patients are relevant to improving safety in the use of medicine in these settings.
During the 2 study periods, the study populations had similar characteristics regarding the number of residents receiving care, sociodemographic data, physical function, and medication use. Therefore, the types of MEs reported are comparable. Significant differences were found in the mean MMSE-35 scores of the assessable residents in the 2 periods, although these differences may not have any relevant clinical impact.
The high number of reported errors should be viewed within the context of a high number of dispensed doses and the complexity of the medication use process. The results show that there was a slight increase in the reporting of all errors in the ATDPS period compared with the pre-ATDPS period. This increase was probably due to the continuous training conducted by the Pharmacy Service, which stressed the importance of reporting errors and the promotion of a non-punitive culture as a tool for improvement. The significant decrease in DEs was due to the incorporation of automated dispensing technology. Another study conducted in nursing homes5 found that, despite the use of an ATDPS, there was a high rate of medication administration errors, which were attributed to the complexity of the process. A cross-sectional study with 256 residents from 55 nursing homes in the UK found that the average number of errors per resident was 1.920. This figure is somewhat higher than the figures observed in the pre-ATDPS period (1.1) and in the ATDPS period (1.38). In the present study, the greatest decrease in errors was associated with automated dispensation (blister-packaged medications) vs manual dispensation (non-blister packaged medications). Thus, automated dispensation had a direct effect on the results.
The error classification created by the Ruiz-Jarabo 2000 working group16 includes therapeutic nonadherence as an ME. However, given that the main aim of this study was to compare errors due to the use of different dispensing systems and the overall medication use process, these nonadherence errors were excluded from data analysis. When a study patient with cognitive impairment refused medication (e.g. by spitting it out or being aggressive), the behaviour was classified as nonadherence. Nonadherence or refusal was very common in the nursing homes (i.e. around 40% of reported incidents).
A review of the literature on the incidence, type, and causes of Des11 showed that the incidence of DEs in community and hospital pharmacies ranged from 0.01% to 2.7% per number of dispensed doses. In our study, the percentage of reported DEs per resident under manual dispensing (0.02% DEs per dispensed dose) was similar to that found in the abovementioned study, but it was lower under automated dispensing (0.0016%).
There is widespread use of monitored dosage systems (MDS) for dispensing medication in nursing homes, although there is no clear evidence to conclude that this system reduces administration errors. The British National Health Service found a number of disadvantages to the use of MDS in care homes21,22. Our results showed that an ATDPS increased safety in dispensation to nursing homes. Before the ATDPS was implemented, a project was conducted to analyse the medication use process in the nursing homes, the hospital, and the type of population served. This aspect was taken into account when selecting the technology. For example, a large number of nursing home residents need crushed medication. The ATDPS system can crush the contents of the bag with little manipulation of the content.
A study conducted in a hospital pharmacy showed that the use of bar code technology in the medicine dispensing process reduced DEs by 85%. Furthermore, the percentage of potentially severe adverse drug events (ADEs) due to DEs was reduced by 63%23. In our study, the implementation of an ATDPS and the use of barcodes to guarantee safety and traceability reduced DEs by 91%, and reduced the number of errors reaching the patient and the most severe errors.
It has been shown that Pharmacy Services play a role in the safety of the medication use process in hospitals, not only by detecting prescription errors24, but also by dispensing medication in such a way that its subsequent administration reaches the highest levels of safety. However, few studies have assessed the relevance of Pharmacy Services in nursing homes, in which the indicators of healthcare quality and automation may be different from those assessed in the hospital setting. Falls, pressure sores, infection, and MEs are among the safety indicators used in nursing homes25. Therefore, pharmacists working in this setting need to know how each nursing home functions, both in general and in detail, in order to adapt the dispensation process to its individual characteristics, thus guaranteeing the highest level of safety20.
There is widespread experience of ADS in hospitals and their contribution to patient safety26. However, evidence is scarce on their improving quality and safety in the process of dispensing medicines to nursing homes. At the time of publication of this study, there is no published data on the level of implementation of dispensing technologies in nursing homes in Spain. The only exception is a communication presented at the Spanish Society of Hospital Pharmacy (SEFH) Conference in 2017 by the SEFH CRONOS and TECNO working groups, which reported that only 3.7% of the Pharmacy Services in Spain that dispensed medications to nursing homes used some kind of ADS. Thus, this study is a novel contribution to the literature.
However, this study has limitations. For example, the study mainly addressed a single stage of the medication use process (i.e. the dispensation stage). Furthermore, the study only analysed voluntarily reported MEs rather than directly observed MEs, which would have involved the health professionals and would probably have led to an underestimation of MEs.
Future research should address the most suitable dispensing systems for nursing homes, and analyse in depth the effect of these systems on stages of the medication use process other than the dispensing stage. In our institution, an anticipated improvement in the safety of medication administration are the print barcodes on the dispensing bags, but the Administration does not use them..
Pharmaceutical care to nursing homes should be standardised to achieve equality regardless of ownership of the home or its size.
In conclusion, the implementation of an ATDPS significantly improved safety in dispensing and the subsequent administration of solid medicines to nursing homes. The voluntary reporting of MEs allowed us to compare safety in 2 different dispensing systems in nursing homes.
Contribution to the scientific literature
There are few publications on the automated dispensing of medicines in nursing homes. Given that institutionalized patients are both frail and polymedicated, it is essential to ensure that dispensation is both safe and adapted to the needs of the residents and the institutions.
The results of this study show that an Automated Tablet Dispensing and Packaging System can contribute to the safe dispensing of medicines in nursing homes, in which the institutionalized population is particularly vulnerable to medication errors.
These results derive from the careful selection of an automated system which, in addition to being safe, is adapted to the needs of nursing homes and the medication use process.











 text in
text in