Introduction
The management of elderly patients with multiple morbidity is complex and represents one of the most important challenges for the healthcare system. The care of these patients involves great clinical uncertainty. Given that care protocols usually address a single health issue, they are less useful in this setting, and thus tools are needed to facilitate decision-making1. This situation is common in nursing homes for the elderly or in socio-health centres.
Frailty is a multidimensional clinical entity defined as a state of vulnerability to everyday stressors due to limiting compensatory mechanisms that puts the individual at high risk of poor health outcomes2,3. As a continuous variable, a Frailty Index (FI) based on the accumulation of deficits model with different domains can measure the individuals’ degree of vulnerability and therefore their biological age2. In this sense, FIs could be defined as quantified comprehensive geriatric assessment (CGA)2.
The objective of this study was to describe a first approach to the development of an FI based on CGA within the social and health care setting (i.e., nursing homes), and to conduct a first analysis of the potential of this tool to help healthcare professionals make decisions for individualized drug prescription based on the actual status of the patient.
Methods
The development of the Frailty Index for Nursing Homes (Spanish acronym: IF-CSS) was based on data provided by the recently published FRAGIL-VIG study2 and on other similar proposals aimed at defining a prognostic index4. The development process comprised 2 stages: a) The construction of the IF-CSS, which included selecting the variables and determining their weights; and b) A preliminary analysis, which comprised the administration of the IF-CSS to patients at 2 nursing homes.
Constructing the IF-CSS
Each variable selected had to fulfil the following criteria: it was included in the CGA; it was associated with age and health problems; it should cover a range of domains; it should not saturate too early; and it should not be too prevalent or too rare5.
The variables and deficits were grouped into 4 domains (functional, cognitive/emotional, geriatric syndromes, and disease). The score assigned to each domain aimed at establishing weights similar to those assigned in current validated FIs2,3,5.
The IF-CSS value was obtained by dividing the number of accumulated deficits by the total potential accumulated deficits using a score that ranged from 0 (absence of deficits) to 1 (presence of all deficits)6. Individuals were considered to be frail if they had an IF score greater than 0.2. The submaximal limit was set at 0.7. This limit is a usual characteristic of most FIs and indicates that a person cannot cope with further deficits7.
Analysis of the IF-CSS
The performance of the IF-CSS was assessed in 2 nursing homes serving a total of 296 patients. All patients who had been administered a CGA in the previous 6 months were included. The IF-CSS scores were retrospectively obtained by using the variable scores from the previous CGA.
Results
Constructing the IF-CSS
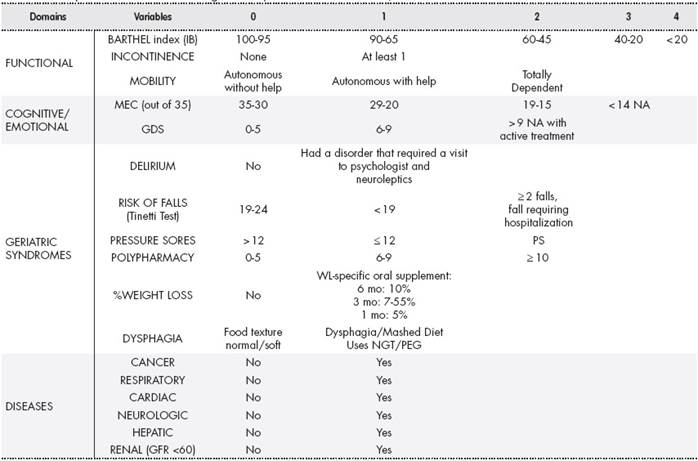
Table 1 shows the IF-CSS items. The 17 selected variables included 27 deficits. The weights assigned to each domain were as follows: functional, 26%; cognitive/emotional, 19%; geriatric syndromes, 33%; and disease, 22%.
Analysis of the IF-CSS
A total of 269 patients were included (average age: 82.9 years; SD: 8.8); 76% were women.
In the functional domain, the BARTHEL index (BI) showed that 49% had severe dependence (BI ≤ 45) and 32% had total dependence (BI ≤ 20). In total, 76% had at least 1 type of incontinence, and 45% needed a wheel-chair or were bedridden.
In the cognitive/emotional domain, the Mini-Mental State Examination (MMSE) showed that 79% had some degree of cognitive impairment (MMSE < 30), and of these patients 45% had severe cognitive impairment (MMSE ≤ 14; n = 95). The Yesavage Geriatric Depression Scale (GDS) could not be administered to 32% of the patients due to their cognitive deterioration; 29% of these patients were receiving antidepressant treatment.
In the geriatric syndrome domain, 23% of patients had experienced an episode of delirium and 22% had experienced a fall. In total, 39% of the patients (n = 106) were at risk of pressure sores (Norton score ≤ 12) and 14 patients had at least 1 pressure sore. The average number of medications taken per patient was 9 (SD 3), with 36% taking 10 or more medications. In total, 5% of patients had experienced a weight loss of more than 10% in the previous 6 months, 14% were receiving oral nutritional supplements, and 29% had dysphagia or received a mashed diet.
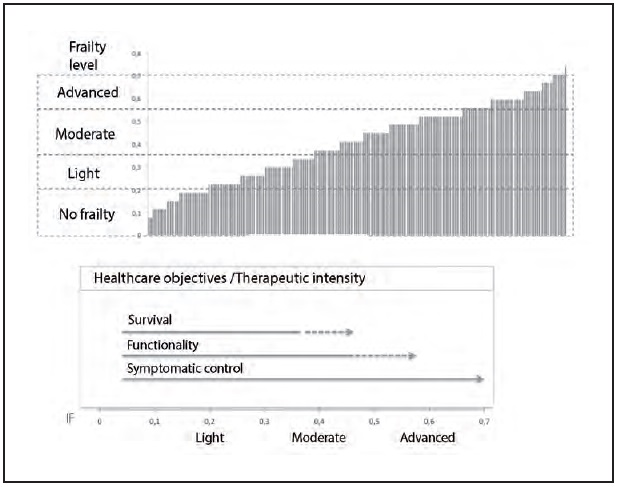
The most common diseases were neurological (64%) and cardiac (43%). Figure 1 shows the distribution of observed values for the IF-CSS index in the study population and the typical values used as cut-off points to determine the level of frailty.
The IF-CSS used in the study population retained the FI submaximal limit of 0.7. This value was reached by 8 patients, and only 1 patient exceeded it (0.37%) with a score of 0.74. In total, 14% (n = 39) of the patients had a score of less than 0.2, and therefore 86% of the patients were considered to be frail. In total, 60% had either moderate frailty (n = 95; IF-CSS: 0.35-0.55) or advanced frailty (n = 67; IF-CSS > 0.55) (Figure 1). Given that all the variables are included in the CGA, the index can be calculated in 2 to 3 minutes.
Discussion
As a continuous variable, the FI is a useful tool to assess overall patient status. It could therefore be useful in individualizing pharmacological treatment by determining the level of therapeutic intensity to be implemented.
The literature recommends the inclusion of 30 to 40 deficits in these kinds of indices to maintain their predictive capacity. However, in this first approach, we only included 27 deficits grouped into 17 variables commonly included in the CGA administered in nursing homes to facilitate the implementation of the index in caregiving practice. One of the objectives was that the index should be quick and simple to administer.
The IF-CSS fulfilled the criteria established for the selection of the variables and preserved the weight of each domain in the final result. The geriatric syndrome domain had the greatest weight and was slightly greater than that described in other FI proposals. This aspect may be because such deficits are followed-up with increased frequency in nursing homes due to their impact on the patient’s quality of life and the level of care required. Most of the variables included were measured using indices by assigning a value according to the score obtained. Dichotomous scoring (0-1) was applied to variables with less diversity. For example, it is simple to determine if a patient has dysphagia or not (i.e., a dichotomous variable), but variables such as cognitive or functional impairment require a greater number of deficits to obtain a more accurate score. This approach to scoring also allowed us to balance the weight of each domain and to maintain the percentages proposed by other authors2,3,5. In the emotional domain (i.e., the GDS scale), the use of antidepressant treatment (Table 1) was assigned a positive score to avoid assigning a negative score for the absence of depression due to the treatment itself or due to its not being assessable in patients with advanced cognitive impairment.
The final selection of variables differed from that of other proposals. For example, we did not include functional capacity as measured by the instrumental activities of daily living (IADL), because the vast majority of people in nursing homes are fully dependent at this level. Neither was the social domain included, because it is understood that the social needs of institutionalized patients are almost completely covered by the center, and thus there would be few differences between patients.
Despite this study being a first approach, the results show that the IF-CSS has discriminative capacity regarding the level of frailty. As an example of its potential usefulness, the results of the IF-CSS suggest a therapeutic approach addressing functional maintenance in the 35% of patients with moderate frailty, or a more conservative approach mainly addressing symptomatic or palliative control in the 25% of patients with advanced frailty.
This first approach is being developed in two directions. On the one hand, we are going to assess the inclusion of some of the deficits which were excluded in this first proposal. These deficits are included in the CGA and we consider that they can have an impact on patient vulnerability. Thus, we will include: a) the variable family support for the institutionalized person (i.e. within the social domain); b) the variable moderate-severe pain as a symptom of severity; and c) the variable hospital admission in the previous 6 months. On the other hand, we will attempt to validate the predictive capacity of the FI for mortality. This will be achieved by incorporating the IF-CSS into the CGA routine administered every 6 months to patients in nursing homes in which pharmaceutical care forms part of the work of the interdisciplinary team.
Contribution to the scientific literature
This study describes a first approach to the use of a frailty index as a basic tool to diagnose patient frailty in the setting of nursing homes.
The frailty index could be a very useful tool to facilitate decision making when individualizing pharmacological treatment in complex chronic patients.











 texto en
texto en