Introduction
Even though medications are used to prevent, diagnose and treat diseases, their use can produce health problems, called drug-related problems (DRPs): “any undesirable event experienced by a patient that involves, or is suspected to involve, drug therapy, and that interferes or could potentially interfere with achieving the desired goals for the patient”1. A DRP can be the cause of treatment failure, and can even trigger new medical problems, more complex than the disease that was being initially treated2.
Pharmacotherapy-associated morbidity represents a serious public health problem, because it leads to a high demand of healthcare ser-vices, and this entails major healthcare expenses, determined by an increase in hospital stay; it is one of the main causes of death in developed countries3, above diabetes and pneumonia.
In the American health system, 0.8 US$ per dollar spent on medications are used to repair the damage caused by a medication4. Medication-related errors cause at least 1 death per day, and damages to approximately 1.3 million persons per year5.
In Colombia, according to the Pharmacovigilance Report by the National Institute for Drugs and Food Vigilance (Instituto Nacional de Vigilancia de Medicamentos y Alimentos, INVIMA), 12,066 DRP reports were processed during the first two months of 20176.
Based on this, and considering that the essential basis for the concept of pharmaceutical care assigns new responsibilities to Pharmacists regarding patients, and having as final clinical objective the prevention of morbidity and mortality caused by medications, through a pharmaceutical practice targeted to ensuring an adequate pharmacotherapy, which is safe and effective for all patients5, the objective of this study was to determine the prevalence of hospital admissions associated with DRPs in the Emergency Unit of the Hospital Universitario San Vicente Fundación (HUSVF) and to conduct any relevant Pharmaceutical Interventions (PIs).
Methods
An observational descriptive cross-sectional study, associated with the treatment of patients who attended the Emergency Unit of the HUSVF due to DRPs between February and April, 2017. DRPs were classified according to the Third Consensus of Granada on DRPs1, and its adaptation according to the Pharmacovigilance Protocol of the institution7.
There was a daily review of the clinical records of all patients admitted to the Emergency Unit of the HUSVF on the day before, including patients of all age groups. The tool used for data collection was a database designed in Office Excel®, where the epidemiological data from the clinical records were recorded. There was an analysis of the pharmacotherapeutic profile of those patients who were hospitalized. The patient or their relatives were interviewed, in order to obtain more information about their health problem.
According to the information obtained, PIs were conducted in order to achieve the desired therapeutic objective, thus reducing any undesirable effects and increasing the benefits of the medication administered. The most relevant PIs were recorded in the clinical record of the patient.
PIs were adjusted to the institutional program, and were targeted to the healthcare staff, the patient, or the relevant EPS (Health Promotion Company), in order to prevent any future DRPs. They were classified as follows:
Clinical Interventions: Adequate dose, relevance of the use of the medication, drug-drug interactions, administration schedule, and adequate recommendations for patients regarding administration.
Technical Interventions: Incompatibilities in “Y”.
Administrative Interventions: Actions targeted to the administrative management of the medication with the EPS.
The education for patients and relatives regarding the adequate use of medications was not taken into account as a type of intervention, because it would be difficult to measure it quantitatively as a variable within the study; besides, there would not be enough time to include the patient load. However, during the interviews with patients in order to achieve other types of interventions, they were always orientated about their adequate use. The healthcare staff also provided education, in addition to the patient education groups available in the hospital for specific conditions.
Data processing was conducted through the SPSS statistical package, version 24.0.
This project was approved by the Ethics Committee of the HUSVF.
Results
There was a review of 21,424 clinical records between 14thFebruary, and 30thApril, 2017, of patients admitted through the Emergency Unit of the HUSVF; of these, 822 patients had a DRP as cause for admission, with a 3.8% prevalence. The mean hospital stay of these patients was 4.6 days; 719 (87.5%) of patients had < 10 days of stay, and the most frequent range was 0-1 days with 374 patients (45.5%).
Their sociodemographical and clinical characteristics appear inTable 1.
Table 1. Sociodemographical and clinical characteristics of patients admitted at the Emergency Unit of the HUSVF due to a DRP between February and April, 2017

Table 2is a classification of DRPs according to the adaptation of the Third Consensus of Granada. The category with the highest frequency reported was need, with 346 admissions (42.1%); followed by the efficacy category, with 311 admissions (37.8%). And within the safety category, adverse reactions to medications (ARMs) stood out with 98 admissions (11.9%). There were 12 undesired drug interactions, representing 1.5% of the total DRPs.
Table 2. Drug-related problems and their causes that led to admission at the Emergency Unit of the HUSVF between February and April, 2017
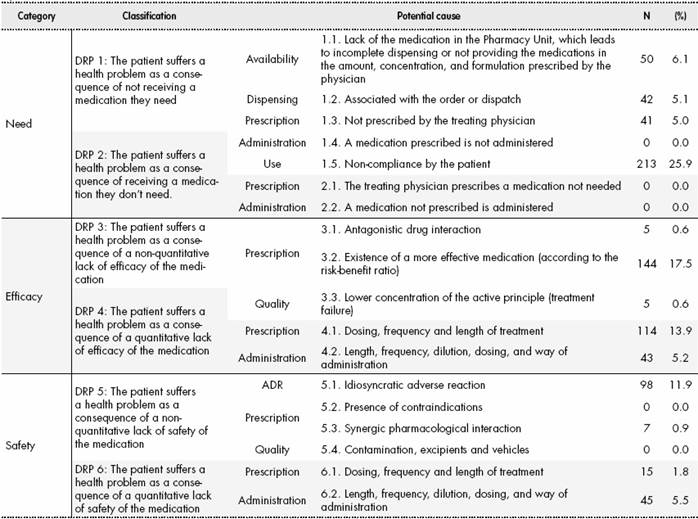
ADR: adverse reactions to medications; DRP: drug-related problems.
The pharmacological group with the highest proportion of association with DRPs was psychotropic drugs, with 137 cases (16.7%), followed by drugs for hypertension, with 105 cases (12.8%). Of the total DRP cases, the neurological system was the most affected, with 208 cases (25.3%), and 198 of these could have been prevented; followed by the cardiovascular system, with 132 cases (16.0%), of which 723 cases (87.7%) could have been prevented.
Of the 822 patients included in the study, a pharmacotherapeutic profile was conducted to those 138 (16.8%) that were hospitalized; the remaining 684 (83.2%) were excluded from the PI analysis, and 288 of these patients excluded received education by the nursing staff about the DRP that led them to the Emergency Unit. At least one PI was conducted for 137 patients with a pharmacotherapeutic profile. In total, 150 PIs were conducted: 68 were clinical (45.3%), 1 was technical (0.7%) and 81 were administrative (54%). It was impossible to conduct one administrative PI because the patient because the patient did not have EPS to report the case to.
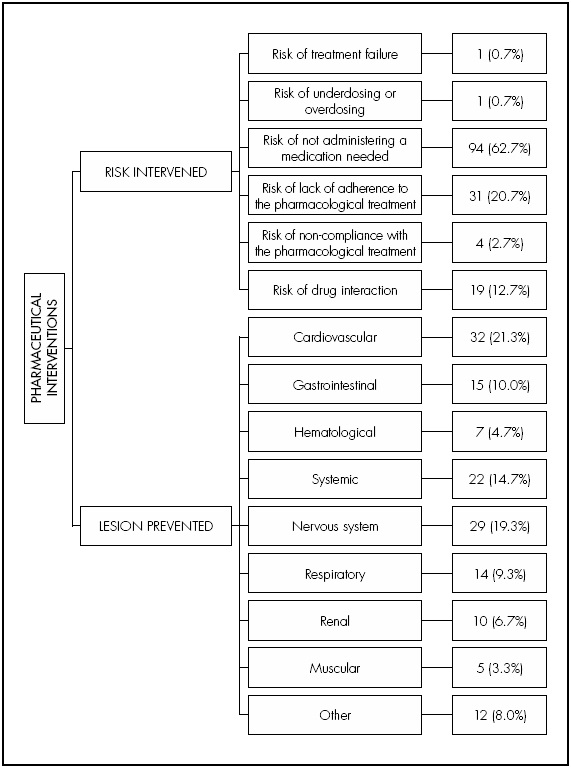
There was a 95.3% proportion of PI acceptance.Figure 1shows the risks object of interventions in all patients with PI, as well as the lesion prevented in those cases were the PI was accepted.
Discussion
Some studies have been conducted in recent years, with the aim to assess the prevalence of DRPs in patients admitted through the Emergency Units; these studies have reported a prevalence between 1.0% and 33.1%9 10-11; in the present study, the prevalence was 3.8%. Anyway, these data are difficult to compare, because the time of the studies, their methodology and the way to classify DRPs are different in each center; however, it is evident that these are problems that require an intervention, as they have a direct and negative impact on public health.
Moreover, 822 DRPs were found, that is to say, 274 DRPs/month, compared with other studies with 71 DRPs/month11, 43 DRPs/month and 404.9 DRPs/month12, but over longer periods of time, which demonstrated the efficacy in the identification of the problem under study.
The highest percentage of DRPs appeared in women, and this is consistent in different studies; this fact can be associated with a higher intrinsic sensitivity to adverse reactions in this gender9,11,13,14.
When analyzing the frequency of DRPs according to age, the higher percentage was found in the age range between 18 and 59-year old (46.5%), and the group with the lowest percentage was represented by persons between 0 and 1 years of age (1.9%). Some articles have reported a higher frequency of DRPs in patients > 60-year- old15; in this study we have observed a high percentage of 32.2%, but it is not the group with the highest incidence, and this shows that age is not a determining factor for the presence of DRPs.
Some authors suggest that polymedication is one of the causes for the presence of DRPs16,17; in this study, we found that the highest percentage of patients were only with 1 medication, which showed that risk is not associated to the number of medications that a patient might be taking, but to the effect associated to each of them.
In some studies, the DRP classification with the highest incidence was efficacy18,19, while in our study, the DRP with the highest percentage was need; the reason for this was that the EPS did not provide patients with the medications required for treating their conditions, or it did not supply their complete treatment.
The percentage of undesired drug interactions was 1.5% of the total DRPs; some articles reported 33.0%20; the concern about this piece of data is that all interactions can be prevented, and this demonstrates once again that drug interactions present a high risk for patients, and that in most cases they are not taken into account in clinical practice.
The neurological system was the most affected; this was not reported as one of the most affected systems in the bibliography reviewed. The cardiovascular system was the second most affected, and this is consistent with the reports from another study18; therefore, it is highly important that those persons on treatment with these medications undergo a more frequent medical monitoring.
The percentage of avoidable DPRs was above the one reported by some studies, determining as avoidable up to 73.0%19. This result is very important, because it shows that this figure can be reduced by improving the weak points associated with medications, such as dispensing and treatment adherence.
The percentage of accepted interventions in our study was 95.3%, similar to those recorded in the majority of studies (84.0-99.0%)(19 -21); it is worth highlighting that other studies reported an acceptance rate of 41.7%12and 2.8%22. The acceptance of PIs has an impact on patient health, because there is a reduction in the risk of adverse effects, and this helps to improve the adherence to pharmacological treatment.
They most relevant type of intervention was the one classified as administrative, with 54.0%; this was caused by patients not receiving their medications by the Pharmacy Unit, or delays in their authorization by their respective EPS, a situation consistent with the crisis in the health sector currently occurring in this country. Clinical interventions should also be pointed out, associated with administration time, which targeted the nursing staff (20.7%), and the relevance of this in terms of patient care.
The risk prevented with pharmaceutical interventions by 62.7% was the unnecessary administration of a drug, followed by the risk of Lack of adherence to pharmacological treatment, with 20.7%; this result was not found in the studies reviewed, and we consider it to be highly important, because cross-sectional-type actions can be generated to reduce this risk in health centers.
The hospital stay for the majority of patients was < 10 days, and the most frequent was 0-1 days (45.5%); this is very similar to the 7 days of hospital stay reported by other articles23, which represents high costs for the public health setting; and a great proportion of these could have been prevented by conducting a pharmacotherapeutic follow-up of patients.
When analyzing DRP severity, 14 of the 822 patients included in the study had a fatal outcome, and DRPs were a factor contributing to the death of these patients. This result was not analyzed in the studies with which this study was compared, and it is highly relevant, because it shows that a bad use of medications leads to fatal outcomes.
The conclusion is that the lack of consideration and analysis of DRPs could lead to a failure of the therapeutic approach, and therefore to the failure in the search for an improvement in health and quality of life. There are different strategies for implementing patient safety from the perspective of medication. The pharmacist plays an essential role in patient healthcare, helping with the prevention and adequate use of medications. There is an increasing need to integrate this professional group into multifactorial healthcare, in order to contribute directly not only to a scientific and rational use of medications, but also in terms of working as part of this team for the comprehensive health of patients. The PI program has demonstrated to offer an invaluable contribution to the public health system, by improving drug safety in treatments, and reducing costs and problems in public health.











 text in
text in