Introduction
At the present time, HIV infection is considered a chronic disease due to the extraordinary decrease in mortality produced after the introduction of highly active antiretroviral therapy (ART) and the subsequent appearance of innovative and more potent drugs with better dosage regimens. The increasing in the survival rate has led to a parallel aging of the HIV+ population1.
Additionally, as in the general population, the increasing in age leads to the appearance of concomitant diseases, of which those related to cardiovascular risk2. Analysis of populations such as cohort D:A:D3 indicate prevalence in the HIV+ setting of approximately 33% of patients with hypertriglyceridemia, 22% hypercholesterolemia, 8% arterial hypertension and 3% diabetes mellitus, among other comorbidities.
Logically, the appearance of concomitant diseases leads to an increasing in the use of medications. Marzolini et al. show that that from the age of 50 onwards patients receive an increasing amount of concomitant treatments4. The increasing in concomitant medication could even affect the adherence to antiretroviral treatment, a key aspect in the control of the pathology5,6.
Thus, polytherapy in people who live with HIV (PLWH) is becoming more frequent7. It is worth to mention that there is a study which analyses data from a Canadian cohort (1990 to 2010), the results shows that the total number of daily drugs decreased over time due to the simplification in antiretroviral therapy regimens. However, in 2010, 22% of patients took ≥ 10 drugs, 51% of them were antiretroviral drugs. In this same study, patients > 45 years of age took a daily average of 3 pills more than younger patients. On the other hand, the Swiss cohort notes that in PLWH > 65 years, 14% took ≥ 4 drugs every day not related to HIV. Because it is sometimes possible that not all medications are recorded, it is possible that the prevalence of polytherapy is underestimated. This can be contributed by self-medication, a frequent process among PLWH.
Although no polytherapy cut-off point is optimal for predicting adverse events, the latest accepted definition includes ≥ 6 drugs8 which seems reasonable to identify patients at risk and who need a medication review. In recent years, the concept of “excessive polytherapy” has been introduced, this concept refers to the use of ≥ 10 drugs. In this context, the next therapeutic change will be the control of polytherapy in these patients.
Although the need for multiple treatments may be due to the need to address the different comorbidities, polytherapy is associated with a potential risk of drug interactions and adverse events, a lack of adherence to treatment, an increased risk of hospitalizations and death. Many of these adverse events could be potentially preventable8-10.
Traditionally, the focus on the measurement of polytherapy has been quantitative, based on the number of prescribed drugs. However, in recent years a much more qualitative analysis is being carried out, since the same number of drugs may differ, among others, in the administration guidelines, pharmaceutical forms, preparation, administration, etc. The University of Denver has developed the Medication Regimen Complexity Index (MRCI). There are an increased number of published papers, both in the field of HIV and other chronic diseases in which the usefulness of MRCI is determined by the follow-up of patients and their relation to different health outcomes11-13. Additionally, the MRCI value for ART continues to decrease gradually, although this is not the case for the concomitantly prescribed medication (CPM)14.
As in other chronic pathologies, the values, preferences, beliefs and attitudes in relation to pharmacotherapy can condition the taking of medications by patients and, consequently, the adherence and therapeutic success of them15. Therefore, it is necessary to know this aspect in order to optimize the usual follow-up of this type of patients and maximize the benefits of the assistance and prescribed pharmacotherapy. It is essential to know the perceptions about the pharmacotherapy that patients have.
The management of PLWH, especially elderly ones, about its pharmacotherapy complexity is of growing concern, as shown by the increasing number of articles addressing this problem in recent years. However, we need to deepen our understanding of the new concepts and to confirm the results based on them, given that the definitions used, particularly those of polytherapy and medication regimen complexity.
Currently, there is no study, including a patients-centered perspective that has evaluated the difference between the pharmacotherapeutic complexity perceived by patients and the one calculated through the MRCI.
Thus, the aim of our study is to determine the difference between the pharmacotherapeutic complexity index by MRCI and it’s perceived by patients (PPC) through a visual analogue scale (VAS) in PLWH with ART. The secondary aim is to analyze the relationship between clinical and pharmacotherapeutical variables and the pharmacotherapeutic complexity index by MRCI and by VAS.
Methods
Prospective, single-center and observational study conducted from the 1st of October of 2017 until the 31st of January of 2018. Patients were eligible for inclusion if they were PLWH, were over 18 years of age on ART drugs for at least 6 months. They were followed up by the pharmaceutical care consultation of viral diseases hospital pharmacy service. Patients who participated in clinical trials, not signed consent form or missed pharmaceutical follow-up program for any reason were excluded.
Data collected from the electronic medical record included: demographic data (sex and age); clinical endpoints: plasma viral load (copies/millilitre (mL); considered detectable if it was greater than 20 copies/mL) and CD4+ T-cell count (cells/microlitre) and number of comorbidities.
Regarding pharmacotherapeutic endpoints: HCV and/or HBV confections; type of ART therapy (classified as (a) two nucleoside reverse transcriptase inhibitors (NRTI) plus a non-nucleoside reverse transcriptase inhibitor (NNRTI), (b) two NRTI plus a protease inhibitor (PI), (c) two NRTIs plus an integrase strand transfer inhibitor (INSTI) and (d) others16); number of concomitant medications (only was considered if it was prescribed with a minimum duration of 60 days); polymedicated (defined as a treatment with five or more drugs, including ART17); adherence to ART and concomitant treatment and complexity index by MRCI18 and a VAS19.
Adherence to ART was measured with the Simplified Medication Adherence Questionnaire (SMAQ)20 and hospital dispensing records21. Adherence to concomitant medication was measure with the Morisky-Green questionnaire (MMAS)22 and electronic pharmacy dispensing records. For both types of treatment, the multi-interval adherence index will be used for the last 6 months of treatment.
Patients will be considered adherent if adherence through dispensing records is > 95% and is considered adherent through the SMAQ questionnaire and the MMAS score.
We obtained the number of comorbidities and comedications for other chronic diseases (non-HIV drugs) from review of the medical history and electronic health prescriptions program of Andalusia Public Health System. The remaining variables were obtained by consulting analytics, microbiology reports, and from review of the medical history of each patient.
Based on the complexity index, the MRCI was calculated using a web tool of Colorado University available in http://www.ucdenver.edu/academics/colleges/pharmacy/Research/researchareas/Pages/MRCTool. aspx18 based on an adaptation of the score created by Martin et al.23 This validated tool includes 65 items grouped into three subgroups: dose forms, dosing frequencies, and additional instructions relevant to drug administration. Calculated value was performed through. Based on a previous study24 patients were classified, by consensus definition, in low MRCI or high MRCI, according to the median of the MRCI ART, MRCI total, MRCI concomitant medication. This score has previously been validated23,24 and is applicable to children and adults with HIV.
To evaluate the perceived complexity, patients on ART who came to pharmacy departments for a drug refill were asked to assign a mark on a VAS ranging from 0 (minimum) to 10 (maximum) according to their perceived complexity of their ART and concomitant treatment. The PPC value was categorized as low or high following the median of the VAS.
The ART drugs were obtained from a pharmacy-dispensing outpatients program (Dominion-Farmatools©). The rest of the treatment was collected from an electronic health prescriptions program of Andalusia Public Health System. The remaining end-points were obtained from analytics, microbiology reports, and from the review of the medical chart of each patient.
Statistical analysis
For this study, we carried out a descriptive analysis. Quantitative variables were summarized with medians and interquartile ranges (IQR = quartiles 25 and 75). Qualitative variables were characterized with frequencies and percentages.
The sample size was calculated from the bilateral test of two proportions, estimating a confidence level of 95% and a power of 80%. In our study, we categorized the Complexity Index measured by the MRCI in High/ Low according to the weighted medians, thus, 50% of the patients would obtain a high CI. All this considered a sample size of 169 patients. Taking into account losses of approximately 15%, the total was 199 patients.
To study the associations between qualitative variables, the Chi-square test or the non-asymptotic methods of the Monte Carlo test and the exact test are applied. To make comparisons of means of quantitative parameters, the indexes under study, between two subgroups of patients, the Student’s t test for independent samples or the nonparametric Mann-Whitney U test was applied.
Finally, we performed a concordance analysis between the complexity index and the patients’ perceived complexity. To do this, we calculated the kappa of Cohen index. Data were analysed using IBM SPSS Statistics version 22.0 software.
The study was approved by the Ethics Committee of the Seville-Sur. All patients received an information sheet explaining the study and were asked to sign a consent form. All data were anonymized and stored on a password-protected computer.
Results
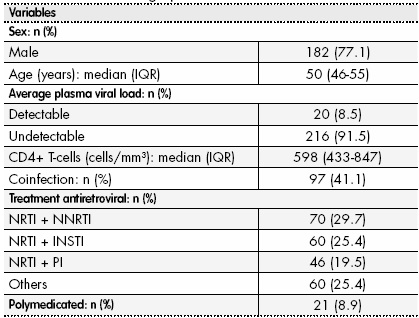
We assessed 236 patients, 77.1% were male. The baseline demographic and clinic characteristics of the patients are shown in Table 1.
Based on the concomitant treatment, the median of comorbidities per patient was 1.0 (IQR: 1.0-2.0) although the percentage of patients with comedication was 52.1%. In relation to the type of comorbidities, 41.1% of patients were diagnosed with viral liver diseases, followed by 28.8% dyslipidemias, 24.6% with pathologies of the central nervous system, 16.1% cardiovascular disease, 12.3% hypertension, 8.5% diabetes and 20.3% other comorbidities.
The percentage of patients with adequate adherence level to the ART and the concomitant medications were 71.6% and 59.3% respectively.
In relations with the main variables, there was a discrete concordance between the complexity index total and concomitant by MRCI and the patients’ perceived complexity (VAS) however there was not a concordance between the complexity index of ART by MRCI and the patients’ perceived complexity (Table 2).
Table 2. Concordance between complexity index by MRCI and VAS scale

ART: Antiretroviral Therapy; CI: Complexity Index; IQR: Interquartile Range; MRCI: Medication Regimen Complexity Index; VAS: Visual Analogue Scale.
The non-adherence of total medication was associated with higher complexity index. The non-adherence in patients with the high MRCI index was 44.92% (p < 0.001) and with high VAS scale was 35.17% (p = 0.003). Furthermore, there were also statistically significant differences between coinfected patients with higher complexity index (MRCI 69.07%; p = 0.004), and VAS scale (61.85%; p = 0.029). Last, the higher number of comorbidities was associated with higher complexity index: MRCI (55.93%; p < 0.001) and VAS scale (46.19%; p < 0.001) (Tables 3 and Table 4).
Table 3. Univariate Analysis of Variables Associated to CI by MRCI
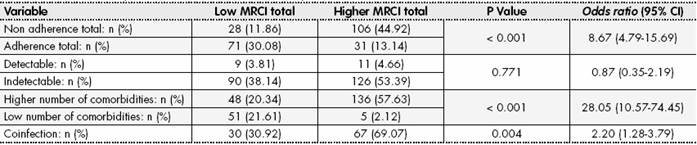
CI: Complexity Index; MRCI: Medication Regimen Complexity Index.
Discussion
In our study, we found that there is a discrete concordance between the complexity index total and concomitant by MRCI and the PPC.
Despite the complexity of ART regimens for PLWH, little is known about the concordance between the complexity measured by MRCI and that perceived by patients with respect to ART and its overall treatment. Several studies have examined the impact of MRCI in PLWH25,26, but none have examined the agreement between the index of complexity measured and perceived by the patient. In addition, it was observed that patients perceived less complexity in their treatments, both ART and concomitant, than what was measured by the MRCI tool. This could be attributable to the support given by health care providers to the patients, making sure that they receive all the necessary information about their ART and addressing any concerns they might have, which reduces their concerns beliefs.
On the other hand, patients presented a greater perceived complexity in the concomitant treatment than in the ART. In this regard, Kamal et al. carried out a study about PLWH on ART for at least 1 year and on at least one concomitant oral medication for at least 6 months followed, observed that the patients had higher necessity and lower concerns scores for their ART in comparison with their concomitant treatment27.
In relation to the other variables associated with the principal variable, we found that non adherence total was an independent associated factor of higher complexity index. Additionally, it was observed that adherence to ART was greater than its concomitant treatment. This can be attributed to the relative unfamiliarity of the patients with their cotreatments, possibly because prescribers provided less information on their in comparison to their ART, and this may have influenced the patients’ evaluation of the prescription and prioritization of their treatment. However it is essential to explore the different beliefs about medicines of comorbid HIV-infected patients which may influence their medication management strategies and decisions to adhere to their prescribed regimens. Several authors have studied the relationship between ART complexity index and its impact on ART adherence28,29. In the study carried out by Stone et al. examined the complexity of antiretroviral regimens. Their results indicated that patients whose regimens included more complex medication were more likely to become non-adherent29.
Manzano-García et al. observed that there is an association between a high index of complexity and non-adherence to the overall treatment of the patient24. Our findings suggest that health care providers should understand the dynamic nature of adherence and that patients may need comprehensive adherence interventions taking the pharmacotherapeutic complexity into consideration.
Furthermore, the coinfection was associated to the higher complexity index. At present, there is limited evidence on patients infected with HCV or HBV and the increasing in overall complexity, however, it is logical to think that when co-infection occurs, the patient increases the number of concomitant medications and this leads to an increase in the complexity index.
Last but not least, we found that the number of comorbidities is an independent factor associated to higher global complexity index. Up to date, all studies have shown that polytherapy is robustly associated with non-adherence, but no study has focused on the HIV population in a large-real practice cohort30. Wimmer et al. studied the relationship between the complexity of concomitant treatment, polytherapy and mortality in comedicated patients, and it was observed that as the complexity of the treatment and polytherapy increased death rates increased28.
The main limitation of our study lies in the unicentric design itself. In any case, this limitation was compensated by the sample size of our study.
It also has other limitations. It is commonly accepted that there is no gold standard for measuring medication adherence. Pharmacy dispensing records are chosen because they are practical and inexpensive. However, this type of method can overestimate adherence. Data from patients with low adherence are reliable, but it is not possible to ensure that patients with perfect dispensation records are taking the medication. To resolve this limitation, ART adherence is measured by a combination of two different methods, those based on dispensing records and those based on adherence questionnaires (MMAS for comedication and SMAQ for ART), as recommended by clinical guidelines16.
Although there are no methods described for assessing perceived complexity in HIV patients, we decided to use a VAS scale due to it provides a simple technique for measuring subjective experience and it is more reliable in low-literacy populations. A common limitation of other published studies is that they only include data on medications of official medical prescriptions; they do not include private health system treatments or alternative medicines. However, this is not seen as a very significant limitation in our study; given the universal coverage of the public health system in Spain, with a small number of patients using alternative medications.
Future lines of research should focus on incorporating a system of measurement of the medication complexity index that is better correlated with the complexity perceived by the patient. In addition, it would be interesting to carry out a study on the pharmacological interventions that should be carried out to improve the complexity of the concomitant treatment of PLWV. Therefore, in future research, we would like to conduct the analysis with larger sample sizes and using more objective measures of adherence such as pharmacy refill records or electronically monitored adherence. It would also be interesting to identify a method to evaluate different patient beliefs about various cotreatments separately as ‘necessity’ beliefs vary from one treatment to another. Lastly, it would be very interesting to analyze if the complexity perceived by patients decreases with respect to the time in treatment or the medication experience.
In conclusion, PPC lower than that calculated through the MRCI tool. The concept of pharmacotherapeutic complexity should include not only the MRCI score but also the VAS value. The findings of this study provide evidence and clarification for both tools should be used to identify PLWH at possible risk of non-adherence. This new concept have to be incorporated and applied to improve pharmacotherapeutic optimization in this population.
Contribution to the scientific literature
This is the first study that analyzes the perception of patients about pharmacotherapeutic complexity.
The results show that, in addition to the theoretical evaluation of pharmacotherapeutic complexity, it is necessary to explore the perspective of the patients.
This tool will allow to identify with greater dynamism that patients are at risk of non-adherence and, therefore, of not geeting objectives in relation to this pharmacotherapy.