Introduction
At the beginning of the 1990s, when the concept of Pharmaceutical Care (PhC) laid its foundations and took its first steps, few authors, even the most optimistic ones, thought that in the intervening decades PhC would contribute so much not only to patients, but to the pharmaceutical profession itself1. However, in every sense, the context has undergone radical changes worldwide. The pharmacological arsenal is much more complex and specialized, there is a new healthcare and regulatory framework, and even a different social framework. Currently, patients are far more active in their treatment, leading to a softening in paternalistic attitudes on the part of professionals toward them. Furthermore, new technologies today play such a relevant role that it would be a serious error to omit them from PhC activity.
In recent years, several authors have agreed that Hepler and Strand's classic definition of PhC has already “hit a ceiling” and needs transforming rather than changing, marking the way to reenvisioning the definition of this activity such that it is much more in line with the times and the needs of the patients2-5. There is also an obvious need for our participation in improving therapeutic outcomes. Thus, we have to meet several challenges, such as complex treatments for chronic diseases that require active patients trained in self-care outside the protected and controlled environment of the hospital setting. In addition, we have to avoid loss of effectiveness due to poor adherence or persistence and prevent iatrogenic events due to avoidable interactions in polypharmacy regimes. Finally, new issues have to be taken into account, such as aging, immunosenescence, fragility, deprescription, or the high economic impact of certain medications requiring careful management in order to optimize outcomes6,7.
Over this period, the advancement of the pharmaceutical profession, in all its aspects, has meant that some professional environments have adapted to healthcare challenges according to their own capacities. In some cases, the regulations that are in force at any one time and the political environment have led to worrying variations in healthcare. At the very least, this situation has to be considered a weakness of our professional model, which, therefore, does not guarantee our contribution to obtaining the best health outcomes in patients.
Blackburn et al.8 proposed that the classic definition of PhC should be redefined to refocus on high-priority patients, differentiate between patients, and include other characteristics beyond their pharmacotherapy. Based on this viewpoint, other authors and societies have also advocated redefining their role9.
Although it seems obvious that we need to rethink healthcare activity, what is less clear is the strategy to follow to face this challenge and be able to provide suitable responses. However, at the international level, little has been done to address this issue in more depth.
Thus, in Spain in 2014, the Spanish Society of Hospital Pharmacy (SEFH) implemented the MAPEX project (“Strategic map for outpatient care”). This initiative arose in the setting of PhC for patients attending outpatient clinics of hospital pharmacy services. Fundamentally, it was a response to a need to transform PhC activity in the face of an alarming professional and healthcare situation, which was due to increasing numbers of patients needing treatment and that was not matched by increases in structural or professional resources. In the beginning, the MAPEX project had a very clear consensual vision: “that of being the bridge that links the patient to their health outcomes and to the healthcare system with maximum efficiency”. In Spain, with the help and participation of other healthcare professionals, more than 200 hospitals and a large number of pharmacists have already collaborated in creating and developing a range of specific initiatives for patients in oncohematologic, neurodegenerative, immune-mediated, and viral disease settings10. From the very beginning, it was clear that the actions to be conducted required working at the micro level (local settings), meso level (political bodies or regulatory decisions), and macro level (identifying and acting on health trends that would affect this professional activity in the near future). In addition, the instruments, processes, and outcomes within this new work model are aimed at placing the patient at the centre of our activity. The new work model should include the following key elements: an orientation toward individual and population needs, efficiency, technical quality, involvement, co-responsibility, accessibility, and professional coordination. Thus, within the MAPEX project, the new PhC model was based on three fundamental pillars -Capacity-Motivation-Opportunity- and was thus called the CMO model11.
Finally, in addition to the relevance of multidisciplinary work, there is evidence of the increasingly important need for coordination between different healthcare levels and a multidimensional approach to the relationships with patients13.
Based on the three pillars of the CMO model, the objective of this document is to provide an updated definition of PhC and the optimal activities required to fulfil this definition while guaranteeing the highest levels of quality and excellence. In addition, we clearly define and differentiate each of the three pillars on which this updated definition is based.
Methods
A working group was formed comprising members of the SEFH and pharmacists from different healthcare fields (specialties, community, and primary care) belonging to various pharmaceutical and medical scientific societies.
A literature search of PubMed was conducted of the available scientific evidence on PhC models as well as PhC activities with the greatest impact and ease of implementation regardless of the level of care where such activity is conducted. The following equivalent Spanish and English keywords were used in combination with each other: Atención Farmacéutica/Pharmaceutical care, Farmacia/Pharmacy, Farmacia Hospitalaria/Hospital Pharmacy, entrevista motivacional/motivational interview, tecnologías para la salud/healthcare technologies, resultados en salud/ healthcare outcomes. The search was conducted from January 2010 to April 2019.
Subsequently, a working definition was developed and the initiatives chosen as key elements were collected and included in each pillar of the proposed model.
After creating an initial list of activities, the draft document was reviewed, assessed, and agreed on by all participants. In order to incorporate all appropriate suggestions and contributions, the final draft document was sent to the different scientific, pharmaceutical, and medical societies as well as patient associations with which the SEFH has a collaboration agreement. Finally, a document was prepared, which included the definition and the selected activities, and approved by the entire working group. The document was presented at the aCadeMiO PhC scientific conference on May 31, 201914.
Results
The consensus definition of PhC was as follows: “Any professional activity by which the pharmacist is linked to the patient (and/or caregiver) and other healthcare professionals, to attend to the patient according to their needs, setting out strategies to align and achieve the shortand medium-/ long-term objectives of pharmacotherapy and incorporating new technologies and the means available to continuously interact with the patients in order to improve their health outcomes”.
Furthermore, “Capacity” was defined as follows: “The provision of PhC to the patient taking into account their individual needs” “Motivation” was defined as follows: “The ability to align the short-term and medium-/long-term objectives for each patient in collaboration with the other professionals who attend them, planning the actions and interventions needed to achieve them”. Finally, “Opportunity” was defined as follows: “Being available to the patient when needed and responding to their needs in real time or in a timely way through the use of new technologies”.
Table 1, Table 2, Table 3 show the activities and key elements for the development of PhC according to each of the three pillars, respectively.
Table 1. Key elements for the development of pharmaceutical care relating to the pillar “capacity”
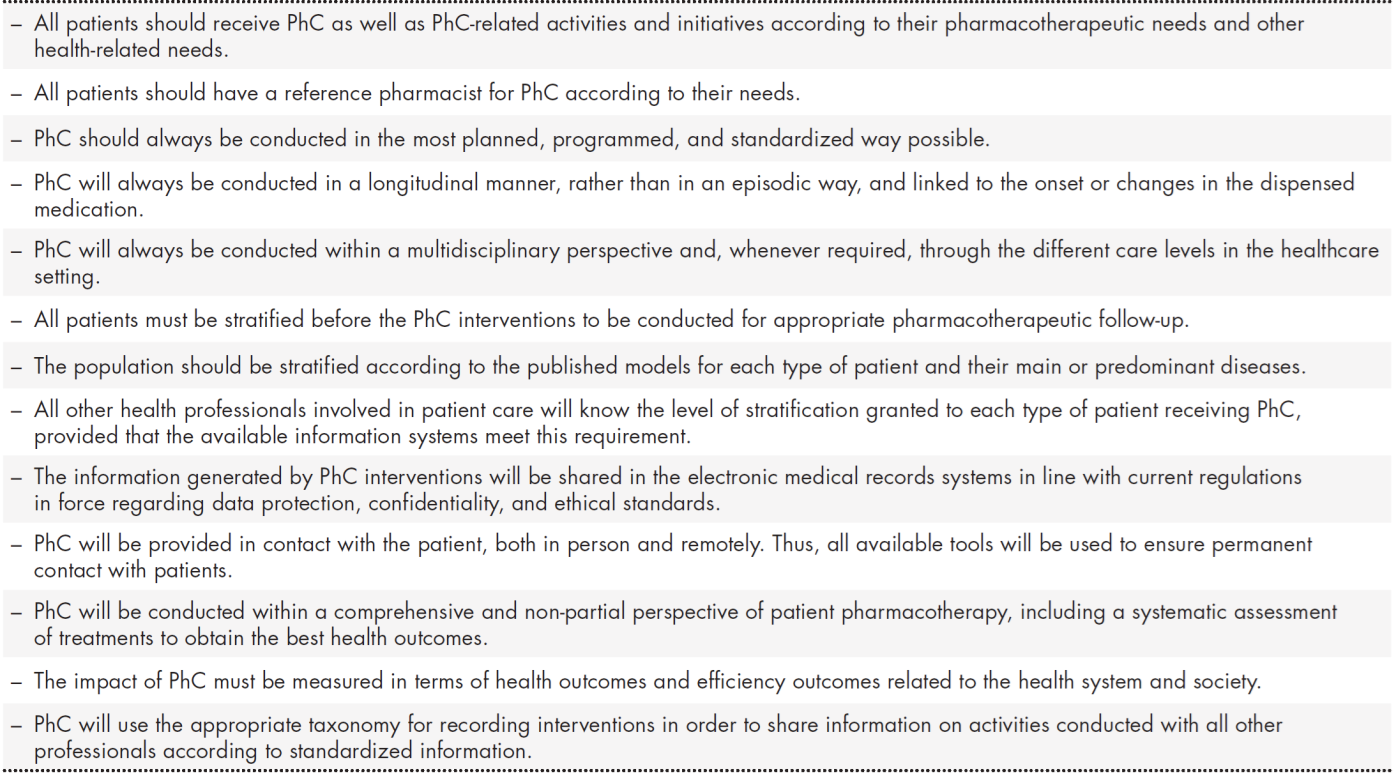
PhC: Pharmaceutical Care.
Table 2. Key elements for the development of pharmaceutical care relating to the pillar “motivation”

PhC: Pharmaceutical Care.
Discussion
The working model that we have followed up to the present has relied heavily on the concept of the primacy of medication while neglecting the uniqueness of each patient. This perspective implicitly centred our focus on the search for individual and transversally focused interventions. Currently, we cannot ignore the fact that patients are individuals and have different needs (this aspect is first pillar of the CMO model) and that there are other factors (educational, cognitive-functional state, demographic, health resource use, etc.) that must be taken into account to provide more value to those patients who have more requirements.
Thus, the need has arisen to stratify or segment our population such that we can organize and prioritize resources. In this way, we are moving from a medication-cantered model to a patient-cantered model. This concept is understood in this document as “Capacity”. Stratification models based on this approach are available along with their specifically defined scores and interventions for chronic, HIV, HCV, pediatric, oncohematologic, and immune-mediated disease patients15-17.
The outcomes of working under this new perspective will be seen in coming years when it is fully incorporated into standard professional pharmaceutical practice. In fact, some authors have already published the results of working within the CMO model18,19. In this line, the clinical practice model of the American Society of Health-System Pharmacists promoted the use of a pharmacotherapeutic complexity index when selecting patients for more intensive PhC20. Tools such as the “Medication Regimen Complexity Index” are essential in any stratification model and facilitate the changeover from a more traditional approach to polypharmacy to a more qualitative and targeted one. Such an approach capable of including pharmacotherapeutic complexity is still little known to other members of multidisciplinary teams in general21.
In contrast to the traditional model, another differentiating aspect is that the working approach is no longer considered as transversally focused intervention, but as longitudinal intervention. Thus, it urges us to relinquish the medication-cantered approach and move to a patient-cantered perspective and its pharmacotherapy-related objectives. Based on this new perspective and the available evidence, the clinical interview, which is commonly used in more traditional models, should give way to the motivational interview. This working tool will allow us to intervene not only on those patients who do not reach their pharmacotherapeutic objectives, but also on those who do so in order to preserve the internal strengths identified during the interviews and ensure they will last over time. In the future, our activity must include the development of communication and interpersonal skills and competencies to help patients achieve short-and medium-long term pharmacotherapeutic objectives, thereby improving therapeutic adherence over time19,22. Moreover, even such a traditional aspect as adherence must be redefined to include new concepts such as primary and secondary adherence. We should go even further: by establishing the level of patient involvement in their pharmacotherapeutic needs, we could identify those patients who make best use of all healthcare resources rather than those who are simply adherent to medication(23,24=.
Pharmaceutical care is not only performed face-to-face, but is also conducted outside the healthcare settings (i.e. in the patient's environment). We have to move away from the idea that PhC is only conducted when the patient is physically present, and in the healthcare centre. We should provide PhC from the healthcare centre in an “ongoing” manner rather than in an “episodic” manner, and not just according to our needs, but above all according to the patient's needs. The possibility of making decisions in “real time” or in a “timely manner” will undoubtedly allow us to be much more efficient and influential. In the near future, the scope of action with the greatest potential is probably the development of projects that improve the so-called concept of “opportunity”. To this end, it is essential to use resources that empower and improve self-care among patients, particularly those included in the baseline levels of the stratification models, and that include information, communication, and learning technologies, knowledge, and key tools, such as telepharmacy25.
This new consensus and approach to PhC will allow us to advance
within the multidisciplinary working approach toward the multidimensional setting of the patient. It is understood that this definition is completely applicable to any healthcare environment and country in the world and will be a way to deal with some of the most important future challenges, such as shared decision making between professionals and patients26.
What clearly emerges from this document is that the establishment of a planned, integrated, and shared service that functions through the different healthcare levels will lead to exponential improvements in desired health outcomes and benefits27. Going deeper, this model has even improved the measurement of new patient-cantered concepts, such as the pharmacotherapeutic experience and improvements to the healthcare experience28.
Like any disruptive innovation, we are conscious that it will not be easy to disseminate this new way of working. In strategic terms, education must begin at all levels, but especially during degree studies and specialist training. One of the first concepts to be taught would be the approach to classifying the pharmaceutical interventions conducted in each patient, because this would represent a key step in interpreting and explaining them in an unambiguous way29.
Given the new professional challenges to be faced, this new way of working with patients will clearly give us the ability to provide the optimal response and to encourage our patients and ourselves to be more motivated, efficient, and timely during pharmatherapeutic interventions30.











 text in
text in 



