Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista de la Sociedad Española del Dolor
versión impresa ISSN 1134-8046
Rev. Soc. Esp. Dolor vol.26 no.3 Madrid may./jun. 2019 Epub 23-Mar-2020
https://dx.doi.org/10.20986/resed.2019.3702/2018
ORIGINALS
Pulsed radiofrequency of the dorsal root ganglion for chronic lumbosacral radicular syndrome refractory to epidural steroid injections
1Profesor Agregado. Universidad de la República, Montevideo, Uruguay.
2Profesor Adjunto. Departamento y Cátedra de Anestesiología. Hospital de Clínicas. Facultad de Medicina. Universidad de la República, Montevideo, Uruguay.
3Asistente. Departamento y Cátedra de Anestesiología. Hospital de Clínicas. Facultad de Medicina. Universidad de la República, Montevideo, Uruguay.
Introduction:
Approximately 20 % of patients with chronic lumbosacral radicular syndrome do not respond to epidural steroid injections. Pulsed radiofrequency of the dorsal root ganglion (DRG) is proposed as an alternative treatment.
Objetive:
To evaluate the analgesic effect of pulsed radiofrequency of the DRG in patients with chronic lumbosacral radicular syndrome, refractory to epidural steroid injections.
Patients and method:
31 patients with chronic lumbosacral radicular syndrome that failed to at least two epidural steroid injections, received pulsed radiofrequency of the DRG, utilizing two cycles of 120 seconds, 45 V and 42 °C. Evaluation was carried out a month later. Brief Pain Inventory was applied before procedure and one month later. A reduction of 2 points in the verbal numerical scale (VNS) assessed with the question 6 of the Brief Pain Inventory, was considered a satisfactory analgesic response. Intensity and Interference Scores were calculated.
Results:
The VNS score decreased from 7.7 ± 2,2 to 5.9 ± 3 (p < 0.01). Intensity and Interference Scores were reduced from 7.1 ± 1.5 to 5.9 ± 2.1 (p < 0.01) and 7.1 ± 1.9 to 6.0 ± 2.3 (p < 0.02) respectively. In 12 patients (40 %) a satisfactory analgesic response was observed. In these patients the VNS decreased from 8.0 ± 1.5 to 3.8 ± 2.6. Intensity and Interference Scores were reduced from 7.4 ± 1.3 to 3.9 ± 1.5 (p < 0.0001) y 7.7 ± 1.9 to 4.9 ± 2,7 (p = 0.002) respectively.
Conclusions:
DRG pulsed radiofrequency produce a mild but statistically significant reduction in VNS and pain interference, in patients with chronic lumbosacral radicular syndrome. However, in 40 % of the patients a satisfactory analgesic effect was observed. In some of them this changes persist after 3 months of the procedures.
Key words: Lumbosacral radicular pain; pulsed radiofrecuency; dorsal root ganglion
INTRODUCTION
The lumbosacral radicular syndrome is characterized by a lumbar pain irradiated to one or more lumbar or sacral dermatomes, commonly called lumbosciatic pain. The pathophysiological basis of this type of pain is irritation due to inflammation or compression of the nerve roots involved 1. The causes of this pain are varied, being disc herniations and disc protrusions more frequent in patients under 50 years old, whereas degenerative changes in lumbar spine, such as foraminal stenosis, are the more frequent causes in patients over 50 years old 1,2,3. When non-invasive treatment based on different pharmacological regimens and physiotherapy fails to achieve satisfactory pain relief or adequate functional recovery, interventional techniques should be considered 3,4. Among them, epidural steroid injection is one of the most frequently indicated techniques, based on a supposed inflammatory process present in the disc-radicular conflict 3,4,5. However, approximately 20% of patients with lumbosacral radicular syndrome present unsatisfactory responses to this treatment 6. The reasons for these results can be diverse, including the chronic nature of radicular pain with little involvement of inflammation, with a predominant role of neuropathic phenomena. In these cases, spine surgery is often offered as a therapeutic approach 6. However, this option is often limited by age and/or physical condition of the patient, or even by the patient's own preferences about the treatments offered. An alternative to the surgical option for the treatment of lumbosacral radicular syndrome, when it is not indicated or is preferable to avoid it, is the application of pulsed radiofrequency on the dorsal root ganglia (DRG) of the roots involved 6. There are several reports about the use of this treatment applied to chronic radicular pain, both cervical and lumbar, with little response to other treatment modalities 6,7,8,9,10. According to the available evidence, the pain relief and the improvement in the functional repercussion of pain range between 50% and 60%, not being reported to date complications with the use of the technique in this modality 6,7,8,9,10. In our setting, experience with this procedure is scarce and has not been reported.
The aim of our study is to assess the analgesic effect of pulsed radiofrequency of the DRG in patients with chronic lumbosacral radicular syndrome refractory to epidural steroid injections, using the Brief Pain Inventory as a tool for evaluation of the outcomes.
The profile of side effects and complications of the technique were also recorded.
MATERIAL AND METHOD
This is a prospective, quasi-experimental study to evaluate the effect of pulsed radiofrequency of the DRG at the lumbar level in a selected population with unilateral chronic lumbosacral radicular syndrome refractory to epidural steroid injections, due to disc herniations, lumbar disc protrusions or canal stenosis, in which spinal surgery was previously discarded.
The Brief Pain Inventory was used as a tool to assess the pain of the selected patients. This self-administered questionnaire allows patients to quantify the intensity of their pain and the degree to which pain interferes with emotional and functional aspects. In addition, the questionnaire consists of additional items evaluating the subjective level of relief that the treatment provides, the location of the pain and its description. The questionnaire is based on questions related to the intensity of the pain and how it affects the person's life in different aspects, scoring from 0 to 10. The analysis of both dimensions allows to obtain the Intensity and Interference Indices. The Intensity Index arises from averaging the responses related to pain intensity, while the Interference Index results from the average of responses related to the functional and affective consequences of pain 11,12,13.
Question number 6 of the questionnaire refers to the intensity of the pain at the time the questionnaire was applied. It can be equivalent to the application of the Verbal Numerical Scale (VNS), frequently used as a tool for evaluating outcomes. The questionnaire was applied prior to the procedure, considering the procedure as a baseline situation, and the questionnaire was repeated for the control one month after the procedure was performed. In those patients in whom a change of at least two points was recorded in the VNS in the first control, new controls were performed three months after the procedure was performed. A new pulsed radiofrequency procedure was repeated in those patients who did not present any changes in the VNS in the first control. The effects of this second procedure were not included in this study.
Inclusion criteria: lumbosacral radicular syndrome of six or more months of evolution, with a nuclear magnetic resonance with evidence of disc herniation, disc protrusion or stenosis of the canal, that have received at least two epidural steroid injections with an unsatisfactory response. In all cases, epidural steroid injections were performed previously, via the parasagittal interlaminar approach in the first instance; followed by a second injection by the transforaminal route one month after the first injection. These injections were performed using radiological assistance. A decrease below two points in the VNS (question 6 of the questionnaire) was established as an unsatisfactory response to epidural steroids one month after the last injection procedure 14. After the failure of these injections, the surgical option was discarded by the neurosurgeons or trauma surgeons at the hospital.
The exclusion criteria were the following: patients under 18 years old and over 80 years old, pregnant women, lower back pain without radicular radiation, bilateral lumbar radicular pain, pain less than six months of evolution, cancer, vertebral crushing, type I diabetes, presence of pacemaker or implantable cardiac defibrillators.
The study was approved by the Ethics Committee of the Hospital de Clínicas. All patients signed the informed consent before performing the procedure.
The procedure was performed in the surgical room in ventral decubitus position. A peripheral venous catheter and standard monitoring were placed. The C-shaped arch was used for the location of the DRGs through the anteroposterior, oblique and profile approaches (Figure 1and Figure 2). A Cosman G4 radiofrequency generator was used. Radiofrequency cannulae number 22 or 20, 10 or 15 cm length respectively, were used, based on the patient's size, with 1 cm of active tip. The radiofrequency cannula was placed on the anterior-superior side or roof of the selected neuroforamens (Figure 1). In the case of S1, the cannula was placed in the first sacral foramen and the radiofrequency of the nerve root was performed, instead of approaching the dorsal root ganglion through the sacrum, because this is considered excessively invasive. The needle was deepened to an imaginary line located in the middle of the thickness of the sacrum (Figure 2).

Fig. 1. Radiological profile view showing a cannula of the anterosuperior angle or roof of the neuroforamen of L5 and S1, approximate topography of the dorsal root ganglion. In S1, the cannula placed through the first sacral hole is observed up to approximately an imaginary line passing through half the thickness of the sacral bone for the purpose of performing pulsed radiofrequency to the nerve root.

Fig. 2. Anteroposterior radiological image of a radiofrequency cannula placed in neuroforamen L5-S1 and S1 after contrast injection.
The corresponding DRG was identified by sensory stimulation, which should be positive between 0.3 and 0.6 mV, and the motor response to the stimulation should be negative at voltages not less than twice those used to obtain the sensory response. Pulsed radiofrequency was performed for 120 seconds, at 45 V and 42 degrees of temperature, after the injection of 1 ml of physiological saline for impedance reduction. After this, a new pulse was repeated with the same characteristics as the previous one. The procedure was performed at previously selected levels. One month after the procedure, the patients were monitored in the outpatient clinic of our hospital. The variables used to measure the effectiveness of the intervention were: Verbal Numerical Scale from 0 to 10 (VNS, question 6 of the questionnaire). A decrease of 2 points on the VNS was defined as a positive response. The number of patients with positive response and the variation of the average of the scores in the VNS were determined before and after the procedure. The Intensity and Interference Indices were averaged before and after the procedure. Finally, the perception of improvement with the treatment was recorded, provided by the Brief Pain Inventory (BPI), expressed by the patient as a percentage (0% did not improve, 100% full improvement). Those patients with positive responses were evaluated again with the BPI three months after the procedure was performed. Patients who did not respond to the procedure were offered a repeat procedure, being excluded from further evaluations in this study. Data were expressed as mean and its standard deviation is shown. To evaluate statistically the differences between the data before and after the treatment, the t test for dependent samples was used. The graphs and statistical analysis were performed using the Graphpad Prism Version 7.0 program. A p value less than 0.05 was considered statistically significant.
RESULTS
Between December 2015 and December 2017, 46 patients treated in the Service of Treatment of Chronic Pain with Lumbosacral Radicular Syndrome, who had been treated with epidural steroid injections with an unsatisfactory outcome were included. A total of 31 out of these 46 patients completed the assessment after one month, 12 presented satisfactory outcomes and, 8 out of the 12 patients completed the assessment again after three months. The remaining four patients with satisfactory outcomes did not return to the second control. One case was discarded because it presented a predominant facet pain in the subsequent evaluation.
Pulsed radiofrequency of L4 and L5 was performed in 18 out of the 30 patients evaluated (23 women and 7 men), of L5 in only 10 patients, and of L5 and S1 in 2 patients. All patients showed disc protrusions in nuclear magnetic resonance, with variable degrees of involvement of the lumbar canal and in one case there was previous spinal surgery. There were no cases of herniated discs. The mean time of pain evolution was 42 months.
The score in the VNS prior to the procedure was reduced from 7.7 ± 2.2 to 5.9 ± 3 (p <0.01, t test for paired samples), taking into account the entire sample (n = 30), which implies a variation of 23% (Table I, Figure 3). The Intensity Index decreased from 7.1 ± 1.5 to 5.9 ± 2.1 (p <0.01), which implies a change of 16%, while the Interference Index decreased by 15% (7.1 ± 1.9 to 6.0 ± 2.3) (p <0.02) (Table I, Figure 4and Figure 5). When evaluating the patients who responded favorably using VNS, 12 out of 30 patients showed a decrease of at least 2 points on that scale, representing 40% of the sample. If we analyze these patients separately, we can observe that the initial values of VNS decreased from 8.0 ± 1.5 to 3.8 ± 2.6 after the procedure, which implies a reduction of 53% (Table II, Figure 6).
Tabla I. Verbal numerical scale (VNS), Intensity and Interference Indices at baseline and at one month of treatment in all the patients (n = 30). Values are represented as mean and standard deviation.


Fig. 3. Values in the Verbal Numerical Scale (VNS) obtained in question 6 of the Brief Pain Inventory (BPI) at baseline and one month after the performance of the pulsed radiofrequency of the DRG in the whole sample (n = 30). A statistically significant (p < 0.01, t test for paired samples) decrease of 23 % after one month compared to baseline values is shown.

Fig. 4. Values of the Intensity Index obtained from the Brief Pain Inventory (BPI) at baseline and one month after performing the pulsed radiofrequency of the DRG in the whole sample (n = 30). A statistically significant (p < 0.01, t test for paired samples) decrease of 16 % after one month compared with the baseline values is shown.

Fig. 5. Values of the Interference Index obtained from the Brief Pain Inventory (BPI) at baseline and one month after performing the pulsed radiofrequency of the DRG in the whole sample (n = 30). A statistically significant (p < 0.01, t test for paired samples) decrease of 15 % after one month compared with the baseline values is shown.
Tabla II. Verbal Numerical Scale, Intensity and Interference Indices at baseline and one month after the treatment in patients with satisfactory response to the pulsed radiofrequency (PRF) (n = 12). The assessment in 8 patients after three months is included. Values are expressed as mean and standard deviation


Fig. 6. Values of the Verbal Numerical Scale (VNS) obtained from the Brief Pain Inventory (BPI) at baseline and one month after performing the pulsed radiofrequency of the DRG in those patients with satisfactory outcome as described in the text (n = 12, 40 %). A decrease of 53 % after one month compared to baseline values is shown. Eight of these patients were assessed also after three months, maintaining the improvement found at one month after the procedure. In both assessments, the differences were statistically significant (p < 0.01, t test for paired samples).
Ten out of these 12 patients showed a variation of three points or more in VNS (more than 50% variation), whereas only 2 patients had a variation of two points on the scale (30% variation). In this group of patients, the Intensity and Interference Indexes were reduced by 47% and 36%, respectively, from 7.4 ± 1.3 to 3.9 ± 1.5 (p <0.0001) for the Intensity Index and from 7.7 ± 1.9 to 4.9 ± 2.7 (p = 0.002) for the Interference Index (Table II, Figure 7and Figure 8). The 30 patients included reported an average of subjective improvement of 59%. No complications of the procedures were recorded in these cases.
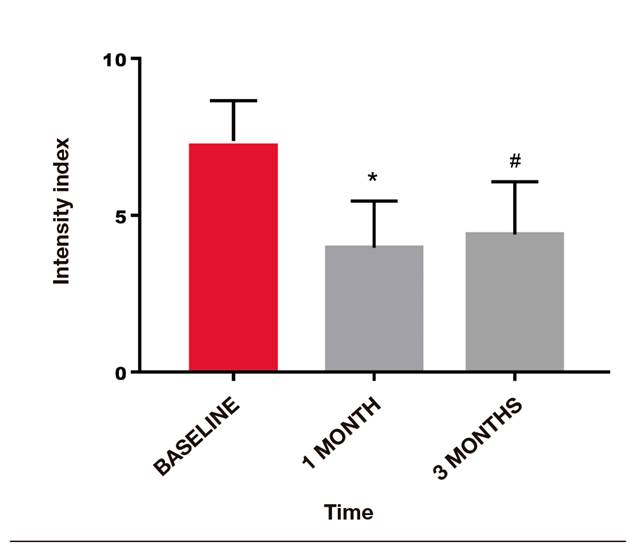
Fig. 7. Values of the Intensity Index obtained from the Brief Pain Inventory (BPI) at baseline and one month after performing the pulsed radiofrequency of the DRG in those patients with satisfactory outcome as described in the text (n = 12, 40 %). A decrease of 47 % after one month compared to baseline values is shown. Eight of these patients were also assessed after three months, maintaining the improvement found at one month. For both assessments, differences were statistically significant (p < 0.01 and p < 0.05, t test for paired samples).

Fig. 8. Values of the Interference Index obtained from the Brief Pain Inventory (BPI) at baseline and one month after performing the pulsed radiofrequency of the DRG in those patients with satisfactory outcome as described in the text (n = 12, 40 %). A decrease of 36 % after one month compared to baseline values is shown. Eight of these patients were also assessed after three months, maintaining the improvement found at one month. For both assessments, differences were statistically significant (p < 0.01 and p < 0.05, t test for paired samples).
In eight patients with a satisfactory outcome after one month, a three-month evaluation of the procedures was conducted. In these, the VNS remained at low values, 3.8 ± 3.3 (p = 0.007), something similar happened with the Intensity and Interference Indexes, being 4.3 ± 1.6 and 5.4 ± 2.5, respectively (p = 0.001 and p = 0.02, when compared with the baseline values (Figure 6, Figure 7and Figure 8).
The group of patients with satisfactory analgesic responses did not present significant differences with the group of patients with poor response to treatment in factors such as age, sex, time to pain onset or lumbar levels treated.
DISCUSSION
Considering the group of patients as a whole, the application of a pulsed radiofrequency procedure produces a statistically significant decrease, although clinically moderate, in the intensity and interference of pain in the daily activities of the patients one month after the treatment was performed. Considering the VNS in this group as reference, a decrease of 1.8 points was found after treatment. Farrar et al. examined 10 clinical studies with a total of 2724 patients with diabetic polyneuropathy, postherpetic neuralgia, low back pain, fibromyalgia and osteoarthritis, using the VNS before and after a given treatment and a 7-point scale in which the overall perception of the change was assessed and that ranged from "much better" to "much worse". Decreases of 2 points or of 30% in pain were associated with "quite better" 15.
Numerous studies have examined the magnitude of the changes in the Brief Pain Inventory associated with different treatments, and the results have shown improvements of 1 to 3 points, depending on the treatment and the underlying pathology. The available information suggests that a change of 1 point in the interference score would be a reasonable objective for studies designed to identify clinically important minimum changes 13. In our group of patients, the Interference Index was reduced by 1.1 points.
If we only consider those patients with satisfactory outcomes as previously defined (decrease of 2 points in VNS), the results of this study show a satisfactory reduction in 40% of patients (12 out of 30 patients), who changed from presenting a severe pain (VNS = 8.0) to a mild to moderate pain (VNS = 3.8). This group of patients also benefited from a 36% reduction in the Interference Index, which translates into an improvement in the quality of life of the patients by reducing the degree to which pain interferes with their daily activities. Ten out of the 12 patients who improved in our sample had an improvement of 50% or more, and the remaining 2 patients showed an improvement of 30%. In 8 of these patients, the improvement was extended to three months after the first procedure.
We consider these responses as acceptable, taking into account that for interventional procedures on the spine a minimum satisfactory outcome is considered, a change of at least 30% compared to the initial assessment after the completion of these procedures 14,15. We also highlight that the improvement of 50% or more in most of the patients who responded move away the placebo effect from the results, an effect that cannot be ruled out in quasi-experimental models, such as in the present study.
If we compare our results with those found in other studies, the percentage of success observed is lower. In 65 patients with lumbar radicular syndrome in whom pulsed radiofrequency was performed in the DRG, Van Boxem found a positive analgesic response in 55.4% of the patients. The authors consider 2 points decrease in a scale from 0 to 10 as a positive response at six weeks after of the procedure 10.
In another study conducted by these authors, 29% of patients who received pulsed radiofrequency as part of the treatment of their radicular pain improved their scores on a scale from 0 to 100, although with a requirement of 50% change as satisfactory response criterion 7).
In another study, published by Trinidad et al., 26 patients with radicular pain on the waiting list for spinal surgery received pulsed radiofrequency of the DRG. When evaluating patients after one year, 19 patients did not require surgery, due to the improvement obtained with the interventional procedure. In these patients, an average decrease of 2.95 points was found in the numerical scale. We point out that 6 minutes of pulsed radiofrequency were used in this study 16.
The main difference between the present study and the other studies reported is that epidural steroid injections were not previously performed in those studies as part of the treatment. In our case, patients in whom both the pharmacological strategies and the usual interventional strategies (epidural steroid injections via the interlaminar and transforaminal routes) had failed and in which the spinal surgery was not indicated for different reasons, remaining then few options available for the treatment of pain, were included.
Establishing the reasons that explain why a group of patients in our sample responded favorably to the treatment and another group did not (a total of 18 patients) is difficult. Our study does not allow to establish an association between variables such as duration of pain or radiological diagnosis and favorable responses. Despite no studies in the literature showing this association were found, a relationship has been described between low scores in the Catastrophizing Pain Scale and high scores in diagnostic scales of neuropathic pain such as DN4 and the Leeds Assessment of Neuropathic Symptoms and Signs (LANSS) with successful responses after pulsed radiofrequency application in the DRGs 10,17. Van Boxem et al., meanwhile, finds in a recent study that age over 55 years, a low degree of functional impairment and a positive response to a previous diagnostic block are associated with a higher percentage of positive responses to the performance of pulsed radiofrequency of DRG in patients with lumbosacral radicular syndrome 18. However, these authors did not find that high scores on the DN4 scale were related to better responses to pulsed radiofrequency in the DRG. In contrast, Lee et al. found a negative cost-benefit difference of the diagnostic blocks performed prior to the pulsed radiofrequency in the DRG, for this reason the authors do not recommend them 19. In a retrospective study, Kim et al. found that the presence of associated musculoskeletal pain and a good response to epidural steroid injections can be considered predictive factors of satisfactory responses to pulsed radiofrequency of the DRG 20.
It seems clear that new studies are needed, with a greater number of cases, to determine aspects related to the selection of candidate patients for the procedure to achieve higher percentages of success.
There were no complications in the treated patients and although the sample is small, it can be inferred that it is a safe technique, since none of the available studies reported complications 6,7,8,9,10,16,21.
There is controversy about the duration of radiofrequency and its relationship with the outcome of the procedure. In the present study, 4 minutes were used, but there are other authors who propose longer sessions 16. Protocols in which the injection of a mixture of steroids and local anesthetics is associated with pulsed radiofrequency in the same procedure have also been described, proposing the association when steroid injections are effective but of short duration 21. An increase in the exposure time up to 8 minutes can be associated with better rates of success, and a comparative study applying 4 minutes versus 8 minutes is currently being developed in our service.
One weakness of our study is the absence of a control group. However, the scientific value and the ethical aspects of proposing a placebo control group are discussed 22. Establishing a control group where the procedure is simulated (Sham group) is questioned from the ethical point of view because the puncture at the level of the conjugation hole can involve a risk. The formation of a group of these characteristics was proposed by Van Boxem et al. in Belgium and its implementation was rejected by an ethics committee, forcing researchers to conduct a prospective follow-up study 10. Establishing a control group with an alternative procedure as a treatment, such as epidural steroid injections, presents similar issues, since the selected patients had previous failure to this alternative.
Another criticism that can be made is the low number of patients who were finally treated and those who could be evaluated after three months. In a study conducted by Van Boxem with a similar design, a total of 60 patients were evaluated, twice as many as those treated in the present study 10. The fact that only one third of the patients had a clinically important effect (greater than 50% improvement) encouraged us to interrupt the present study and to conduct a comparative and randomized study to test the effect of using 8 minutes of pulsed radiofrequency, using as a control group the standard treatment for 4 minutes, study currently in progress. The telephone follow-up in this case was proposed as a mechanism to reduce the loss of controls, in particular at 3 months, which was observed in the present study.
The mechanism of pain relief in the case of pulsed radiofrequency is still under discussion. In this technique, the application of heat does not produce neural injury, but it generates a magnetic field around the exposed neural structure, producing disruption of the membranes, interfering with the generation of action potentials and neuronal ectopic discharges 8. Higuchi et al. showed that the pulsed radiofrequency application of the DRG of mice increases the expression of the c-Fos gene at that level, a finding similar to that observed by Van Zundert et al. 23,24. The clinical relationship between c-Fos expression and pain relief has not yet been determined, but it is an indicator that the technique acts on nociceptive transmission. Other proposed mechanisms of pulsed radiofrequency action in neuropathic and radicular pain models include interference with the release of pro-inflammatory substances at the level of disc-radicular conflict, attenuation of the central sensitization mechanism at the level of the medullary dorsal horn, and enhancement of the descending mechanisms of analgesia through the release of noradrenaline and serotonin 25,26,27,28,29).
Finally, in terms of how to evaluate the results, this is, as far as we know, the first report using the BPI as a tool to study the analgesic effects of pulsed radiofrequency of the DRG. This is a useful tool for this purpose, which contains aspects related to the intensity of pain and its interference on important aspects of the active and emotional life of patients in a single form, which is why we consider it a complete way of evaluation of outcomes. The BPI is used regularly in our service and we have communicated in a previous publication the experience in its use to evaluate the results of the interventional techniques in the treatment of low back pain 12.
CONCLUSIONS
The application of pulsed radiofrequency on the DRG in a group of patients with chronic lumbosacral radicular syndrome, refractory to epidural steroid injections, resulted in a satisfactory analgesic response in 40% of cases. These data are lower than those found in other previously published studies on the subject, although it should be noted that these patients were refractory to both interventional and non-interventional treatments. Therefore, we consider that this is a valid technique for the treatment of refractory lumbosacral radicular syndrome and we believe that an increase in the time of exposure to twice can improve the success rates.
The BPI was presented as a useful and complete tool for the evaluation of the outcomes. No complications of the technique were found in the group of patients studied.
REFERENCES
1. Van Boxem K, Cheng J, Patjin J, van Kleef M, Lataster A, Mekhail N, et al. Lumbosacral Radicular Pain. Pain Pract 2010;10(4):339-58. DOI: 10.1111/j.1533-2500.2010.00370.x. [ Links ]
2. Borenstein D. Low Back Pain. In: Pain Management, Steven D, Waldman MD. Chapter 82. Volume 2. Philadelphia: Ed Saunders, Elsevier; 2007. p. 749-78 [ Links ]
3. Manchikanti L, Abdi S, Alturi S, et al. An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: guidance and recommendations. Pain Physician 2013;16(Suppl 2):S49-S283. [ Links ]
4. American Society of Anesthesiologists Task Force on Chronic Pain Management; American Society of Regional Anesthesia and Pain Medicine. Practice Guidelines for Chronic Pain Management. An updated report by the American Society of Anesthesiologist Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiol 2010;112(4):810-55. DOI: 10.1097/ALN.0b013e3181c43103. [ Links ]
5. DePalma MJ, Slipman CW. Evidence-informed management of chronic low back pain with epidural steroid injections. Spine J 2008;8(1):45-55. DOI: 10.1016/j.spinee.2007.09.009. [ Links ]
6. Abejón D, García del Valle S, Fuentes ML, Gómez- Arnau JI, Reig E, van Zundert J. Pulsed radiofrequency in lumbar radicular pain: clinical effects in various etiological groups. Pain Pract 2007;7(1):21-6. DOI: 10.1111/j.1533-2500.2007.00105.x. [ Links ]
7. Van Boxem K, van Bilsen J, de Meij N, Herrler A, Kessels A, Van Zundert J, et al. Pulsed radiofrequency treatment adjacent to the lumbar dorsal root ganglion for the management of lumbosacral radicular syndrome: a clinical audit. Pain Med 2011;12(9):1322-30. DOI: 10.1111/j.1526-4637.2011.01202.x. [ Links ]
8. Sluijter ME, Cosman E, Rittman I. The effects of pulsed radiofrequency field applied to the dorsal root ganglion-a preliminary report. Pain Clin 1998;11(2):109-17. [ Links ]
9. Van Zundert J, Patijn J, Kessels A, Lamé I, Van Suijlekom H, van Kleef M. Pulsed radiofrequency adjacent to the cervical dorsal root ganglion in chronic cervical radicular pain: A double blind sham controlled randomized clinical trial. Pain 2007;127(1-2):173-82. DOI: 10.1016/j.pain.2006.09.002. [ Links ]
10. Van Boxem K, de Meij N, Kessels A, Van Zundert J, van Kleef M. Pulsed radiofrequency for chronic intractable lumbosacral radicular pain: a six month cohort study. Pain Med 2015;16(6):1155-62. DOI: 10.1111/pme.12670. [ Links ]
11. Keller S, Bann C, Dodd Sh, Schein J, Mendoza T, Cleeland Ch. Validity of the Brief pain Inventory for use in documenting the outcomes of patients with non-cancer pain. Clin J Pain 2004;20(5):309-18. [ Links ]
12. Surbano M, Antunez M, Coutinho I, Machado V, Castroman P. Uso del Brief Pain Inventory (BPI) para la evaluación de las técnicas intervencionistas en el tratamiento de la lumbalgia. Revista El Dolor 2014;(62):10-4. [ Links ]
13. Cleeland CS. Pain assessment: global use of the pain inventory. An Acad Med 1994;23(2):129-38. [ Links ]
14. Gatchel RJ, Mayer TG, Choi YH, Chou CR. Validation of a consensus-based minimal clinically important difference (MCID) threshold using an objective functional external anchor. Spine J 2013;13(8):889-93. DOI: 10.1016/j.spinee.2013.02.015. [ Links ]
15. Dworking R, Turk D, Wyrwich K, Beaton D, Cleeland CS, Farrar JT, et al. Interpreting the Clinical Importance of Treatment Outcomes in Chronic Pain Clinical Trials: IMMPACT Recommendations. J Pain 2008;9(2):105-21. DOI: 10.1016/j.jpain.2007.09.005. [ Links ]
16. Trinidad JM, Carnota AI, Failde I, Torres LM. Clinical Study Radiofrequency for the Treatment of Lumbar Radicular Pain: Impact on Surgical Indications. Pain Res Treat 2015;2015:392856. DOI: 10.1155/2015/392856. [ Links ]
17. Samwel H, Salppendel R, Crul BJP, Voerman VF. Psychological predictors of the effectiveness of radiofrequency lesioning of the cervical spinal dorsal ganglion (RF-DRG). Eur J Pain 2000;4(2):149-55. DOI: 10.1053/eujp.2000.0165. [ Links ]
18. Van Boxem K, de Meij N, Patijn J, Wilmink J, van Kleef M, Van Zundert J, et al. Predictive factors for successful outcome of pulsed radiofrequency treatment in patients with intractable lumbosacral radicular pain. Pain Med 2016;17(7):1233-40. DOI: 10.1093/pm/pnv052. [ Links ]
19. Lee CC, Chen CJ, Chou CC, Wang HY, Chung WY, Peng GS, et al. Lumbar Dorsal Root Ganglion as a prognostic tool before pulsed radiofrequency: a randomized, prospective, and comparative study on cost-effectiveness. World Neurosurg 2018;112:e157-e164. DOI: 10.1016/j.wneu.2017.12.183. [ Links ]
20. Kim SJ, Park SJ, Yoon KB, Kim SH. Predictors of the analgesic efficacy of pulsed radiofrequency treatment in patients with chronic lumbosacral radicular pain: a retrospective observational study. J Pain Res 2018;11:1223-30. DOI: 10.2147/JPR.S164414. [ Links ]
21. Koh W, Choi SS, Karm MH, Suh JH, Leem JG, Lee JD, et al. Treatment of chronic lumbosacral radicular pain using adjuvant pulsed radiofrequency: a randomized controlled study. Pain Med 2015;16(3):432-41. DOI: 10.1111/pme.12624. [ Links ]
22. Manchikanti L, Cash KA, Pampati V, Falco FJE. Transforaminal epidural injections in chronic lumbar disc herniation: a randomized, double-blind, active-control trial. Pain Physician 2014;17(4):489-501. [ Links ]
23. Higuchi Y, Nashold BS Jr, Sluijter M, Cosman E, Pearlstein RD. Exposure of the dorsal root ganglion in rats to pulsed radiofrequency currents activates dorsal horn lamina I and II neurons. Neurosurgery 2002;50(4):850-5. [ Links ]
24. Van Zundert J, de Louw AJ, Joosten EA, Kessels AG, Honig W, Dederen PJ, et al. Pulsed and continuous radiofrequency current adjacent to the cervical dorsal root ganglion of the rat induces late cellular activity in the dorsal horn. Anesthesiology 2005;102(1):125-31. [ Links ]
25. Park HW, Ahn SH, Kim SJ, Seo JM, Cho YW, Jang SH, et al. Changes in spinal cord expression of fractalkine and its receptor in a rat model of disc herniation by autologous nucleus pulposus. Spine 2011;36(12):753-60. [ Links ]
26. Kim SJ, Kim WR, Kim HS, Park HW, Cho YW, Jang SH, et al. Abnormal spontaneous activities on needle electromyography and their relation with pain behavior and nerve fiber pathology in a rat model of lumbar disc herniation. Spine 2011;36(24):1562-7. DOI: 10.1097/BRS.0b013e318210aa10. [ Links ]
27. Erdine S, Bilir A, Cosman ER, Cosman ER Jr. Ultrastructural changes in axons following exposure to pulsed radiofrequency fields. Pain Practice 2009;9(6):407-17. DOI: 10.1111/j.1533-2500.2009.00317.x. [ Links ]
28. Hamann W, Abou-Sherif S, Thompson S, Hall S. Pulsed radiofrequency applied to dorsal root ganglia causes a selective increase in ATF3 in small neurons. Eur J Pain 2006;10(2):171-6. DOI: 10.1016/j.ejpain.2005.03.001. [ Links ]
29. Hagiwara S, Iwasaka H, Takeshima N, Noguchi T. Mechanisms of analgesic action of pulsed radiofrequency on adjuvant-induced pain in the rat: Roles of descending adrenergic and serotonergic systems. Eur J Pain 2009;13(3):249-52. DOI: 10.1016/j.ejpain.2008.04.013. [ Links ]
Received: August 07, 2018; Accepted: November 27, 2018











 texto en
texto en 


