Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Anales del Sistema Sanitario de Navarra
versión impresa ISSN 1137-6627
Anales Sis San Navarra vol.34 no.2 Pamplona ago. 2011
https://dx.doi.org/10.4321/S1137-66272011000200014
Cuboid-navicular tarsal coalition in an athlete
Sinóstosis cubo-escafoidea tarsiana en un atleta
Sr Director:
Tarsal coalitions appear in 2% of the population, although for some the incidence of tarsal coalitions ranges from 0.03% to 0.38%1. Talonavicular and talocalcaneal coalitions are the most common symptomatic coalitions. Their presence in other tarsal joints such as talonavicular, calcaneus cuboid and naviculocuneiform joints is very rare.
Leonard2, in a long series of tarsal coalitions, found that 33% of relatives and 46% of the children of patients with tarsal coalitions also had some type of coalition, with 39% of close relatives having tarsal coalitions. A total of 14% of the relatives had a different kind of tarsal coalition. The male to female ratio ranged from 4:1 to 12:51. Over 50% of the patients with tarsal coalition in one foot are likely to have the same condition in the other foot1.
The most likely aetiology of tarsal coalitions1 in the majority of cases is represented by a genetic mutation which is eventually responsible for a segmentation failure of the primitive mesenchyme.
In a long series of synostosis and tarsal coalitions, Rouvreau et al3 described 57 occurring in the calcaneus navicular bone, 16 in the talocalcaneal bone, 8 in the talonavicular bone, 7 in the calcaneus cuboid bone and 4 in the naviculocuneiform bone, but none in the cuboid-navicular bone. Naviculocuboid coalition represents less than 1% of all tarsal coalitions, with only four cases having been published, although Palladino et al mentions another 17, all as isolated cases of this disorder4. The spontaneous evolution of this type of tarsal coalition is not known.
The objective of this study is to describe a new case of this very rare condition and its coexistence in an adult patient who has practised sport for years, in a practically asymptomatic form.
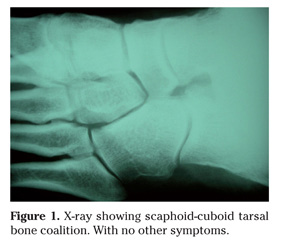
Patient of 45-year-old who came to our hospital due to indirect trauma to the right foot, clinically with grade II sprain of the lateral ligament of the ankle and swelling, pain and tenderness over cuboid, for which an X-ray was performed. The only abnormality was scaphoid-cuboid tarsal bone coalition (Fig. 1), with no other symptoms. The diagnosis of cuboid-navicular synostosis was confirmed by CT scan (Fig. 2).
There was no association with other types of congenital disorders or osteoarthritic degeneration in other tarsal joints. The patient reported no history of repetitive strain or fracture in the ankle, foot or tarsus.
The patient presented local discomfort in the cuboid-navicular area after prolonged effort. These symptoms disappeared after resting from sport for three months.
Physical examination revealed full ankle and subtalar motion. The patient's family was asymptomatic. He had played competition football at various levels for 28 years. In the last five years he ran a marathon and two half-marathons every year, running an average of 40 km/week. He reported having no previous symptoms.
Twelve years later (57 years old), the patient reported having suffered pain in the right tarsus (in the same place) on two occasions which disappeared spontaneously after 1-2 weeks with no treatment. During that time, he participated in sponsored races with 3-4 days of training per week (50-60 kilometres).
At 60 years of age, he continued jogging regularly, participating in popular races, completely symptom-free.
Tarsal coalitions occur due to the absence of differentiation and segmentation of the primitive mesenchyme in the first stages of development. Talonavicular coalition has been reported as a congenital defect of the foot which is discovered by accident in an X-ray and which is frequently associated with symphalangism, clinodactyly, ball-and-socket ankle joint and a big toe shorter than the second toe, with a dominant autonomous hereditary pattern5. It occurs in 2% of the population and is most common in the calcaneoscaphoid bone and talocalcaneal bone. It is very rare in other tarsal locations.
The incidence of peroneal spastic flat foot is not the same as the incidence of tarsal coalition. Not all patients with coalition syndromes have flat feet and not all young people who will ultimately have coalition syndromes have a lack of subtalar motion, particularly in early years, and therefore not all of these patients are symptomatic. Leonard2 found that 76% of the patients were asymptomatic. The mere presence of a coalition is not an indication for surgery.
Tarsal coalitions are characterised in that they do not always cause symptoms and when they do, these are gradual, above all from preadolescence, which is when bone development ends and hence why ossification of the fibrous tarsal layers stops. Intolerance to exercise and prolonged walking as well as frequent ankle sprains often appear. This normally occurs in people with calcaneoscaphoid and talocalcaneal fusion, which are the two most common types. In the most evident cases, patients go to the clinic with a flat foot with clear tension in the peroneal tendons (often called peroneal spastic flat foot), which has also been described in a calcaneus cuboid coalition6,7. They clinically present a subtalar and/or tarsal block and their diagnosis is based on X-ray and CT scan.
On reviewing the literature, we have only found four cases of cuboid-navicular coalition in PubMed in January 20114,6,8,9 and another four in the text by Jahss10 from other authors11-14. In one of the texts published by Feliu8, it was discovered due to the onset of pain symptoms, but the symptoms disappeared with conventional analgesic therapy and no other therapeutic measures were required. This is the same as what happened with the patient we are presenting in this study. Williamson and Torode6 reported that although this type of tarsal coalition is usually asymptomatic, it may become symptomatic, presenting a case of bilateral peroneal spastic flatfoot. Palladino et al4 and Piqueres et al9 each mention a case of a patient with painful feet who also has decreased mobility and deformity of the feet.
Although the spontaneous evolution of this type of tarsal coalition is not clearly known, in view of the published cases and the present case, it appears that it remains asymptomatic except at specific moments which can vary from being asymptomatic to causing peroneal spastic flat foot11.
There is a belief that the existence of a tarsal layer always causes symptoms and intolerance during physical exercise. Calcaneus navicular and talocalcaneal coalitions are generally presented as a type of painful foot15, but other, rarer, types of coalition are usually asymptomatic16. It is likely that this also happens with cuboid-navicular coalition, which explains the excellent tolerance of our patient to intense and prolonged mechanical effort.
This case shows us that although tarsal layers cause a reduction in movement of the tarsus, with the resulting biomechanical alterations, they do not necessarily cause local inflammation with adjacent osteoarthritic degeneration, or an overload of adjacent joints, even with chronic microtrauma from running many kilometres on hard surfaces every year. Treatment should therefore only be initiated in those cases where chronic and/or disabling symptoms are present. It does seem clear that calcaneoscaphoid and above all talocalcaneal coalition often cause pain and disability during effort, probably due to their effects on the biomechanics of the subtalar joint, preventing its proper function. However, cuboid-navicular fusion does not block or affect the biomechanics of the subtalar joint and therefore of the back of the foot. It also preserves the Chopart and Lisfranc joints, so there is no shift of abnormal loads to other adjacent joints. This would explain the absence of chronic symptoms in this type of bone fusion, unlike with other kinds.
In the event that the coalition is symptomatic, treatment with orthotic management may be evaluated17. Cowell18 and Cavallaro and Hadder14 state that cuboid-navicular coalitions may be treated through the re-section and interposition of the extensor digitorum brevis muscle.
The case we present demonstrates that cuboid-navicular coalition is a very rare cause of pain symptoms in an athlete's foot that may not cause prolonged or disabling symptoms or osteoarthritic degeneration of the adjacent joints.
S. García-Mata, A. Hidalgo-Ovejero
Servicio de Cirugía Ortopédica y Traumatología B. Complejo Hospitalario de Navarra. Pamplona.
References
1. Ehrlich MG, Elmer EB. Tarsal coalitions. En: Jahss MH. Disorders of the foot and ankle. Medical and surgical management. 1991, Saunders Company, second edition. Philadelphia. Chapter 38: 921-940. [ Links ]
2. Leonard MA. The inheritance of tarsal coalition and its relationship to spastic flat foot. J Bone Joint Surg 1974; 56-B: 520-526. [ Links ]
3. Rouvreau P, Pouliquen JC, Langlais J, Glorion C, de Cerqueira Daltro G. Sinostosis and tarsal coalitions in children. A study of 68 cases in 47 patients. Rev Chir Orthop 1994; 80: 252-260. [ Links ]
4. Palladino SJ, Schiller L, Jonson JD. Cubonavicular coalition. J Am Podiatr Assoc 1991; 81: 262-266. [ Links ]
5. Doyle SM, Kumar SJ. Symptomatic talonavicular coalition. J Pediatr Orthop 1999; 19: 508-510. [ Links ]
6. Williamson DM, Torode IP. Cubonavicular coalition: an unusual cause of peroneal spastic flat foot. Aust N Z J Surg 1992; 62: 506-507. [ Links ]
7. Pontius J, Hillstrom HJ, Monahan T, Connelly S. Talonavicular coalition. Objective gait analysis. J Am Podiatr Med Assoc 1993; 83: 379-385. [ Links ]
8. Feliu EC. Cubonavicular synostosis. A case report. Acta Orthop Belg 1991; 57: 306-308. [ Links ]
9. Piqueres X, de Zabala S, Torrens C, Marin M. Cubonavicular coalition: a case report and literature review. Clin Orthop 2002; 396: 112-114. [ Links ]
10. Jahss MH. Disorders of the foot and ankle. Medical and surgical management. 1991, Saunders Company, second edition. Philadelphia. Chapter 38: 921-940. [ Links ]
11. Waugh W. Partial cubo-navicular coalition as a cause of peroneal spastic flatfoot. J Bone Joint Surg 1957; 39-b: 520-523. [ Links ]
12. DelSel JM, Grand NE. Cubo-navicular synostosis. A rare tarsal anomaly. J Bone Joint Surg 1959; 41-B: 149. [ Links ]
13. Rankin RA, Baker GI. Rigid flatfoot in the young adult. Clin Orthop 1974; 104: 244-248. [ Links ]
14. Cavallaro DC, Hadder HR. An unusual case of tarsal coalition: a cuboid navicular synostosis. J Am Podiatr Med Assoc 1978; 68: 71-75. [ Links ]
15. Percy EC, Mann DL. Tarsal coalition: a review of the literature and presentation of 13 cases. Foot Ankle 1988; 9: 40-44. [ Links ]
16. Migues A, Slullitel GA, Suárez E, Galán HL. Symptomatic bilateral talonavicular coalition. Clin Orthop 2009; 467: 288-292. [ Links ]
17. David DR, Clark NE, Bier JA. Congenital talonavicular coalition. Review of the literature, case report, orthotic management. J Am Podiatr Assoc 1998; 88: 223-227. [ Links ]
18. Cowell HR. Tarsal coalitions. Review and update. In: Instructional Course Lectures. American Academy of Orthopaedic Surgeons, vol 31, 264-271. St Louis: CV Mosby, 1982. [ Links ]
![]() Correspondence:
Correspondence:
Serafín García-Mata
Complejo Hospitalario de Navarra
Servicio de Cirugía Ortopédica y Traumatología B
C/Irunlarrea, 4
31008, Pamplona-Spain
E-mail: sgarcima@cfnavarra.es
Recepción: 19 de enero de 2011
Aceptación definitiva: 5 de abril de 2011