Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Anales del Sistema Sanitario de Navarra
versión impresa ISSN 1137-6627
Anales Sis San Navarra vol.37 no.3 Pamplona sep./dic. 2014
https://dx.doi.org/10.4321/S1137-66272014000300005
ARTÍCULOS ORIGINALES
Parity implications for anthropometrical variables, lifestyle behaviors and dietary habits in pregnant women
Influencia de la paridad sobre variables antropométricas, estilos de vida y hábitos alimentarios en mujeres embarazadas
L. Goñi1,2, M. Cuervo1,2,3, S. Santiago1,2, I. Zazpe1 and J.A. Martínez1,2,3
1. Department of Nutrition, Food Sciences and Physiology. University of Navarra. Pamplona. Spain.
2. Centre for Nutrition Research. Faculty of Pharmacy. University of Navarra. Pamplona. Spain.
3. CIBER Fisiopatología Obesidad y Nutrición (CIBERobn). Instituto de Salud Carlos III. Spain.
This study was supported by the spanish pharmacists council and the University of Navarra.
ABSTRACT
Background: Maintaining an adequate health status and appropriate lifestyles during pregnancy is of great importance to prevent adverse outcomes for both mother and baby. The present study aimed to assess the nutritional status, socio-demographic features, lifestyle behaviors and dietary habits of pregnant women in Spain, and to identify the influence of parity on these profiles.
Methods: This cross-sectional study included pregnant women from regions all over Spain. The information was collected through a 40 item questionnaire, previously validated, by community health professionals.
Results: The 5,087 pregnant women analyzed had an average age of 31.9 years with an adequate nutritional status. The distribution of the sample was 56% nulliparous and 44% multiparous. The nulliparous reported a better self-perceived health status and nutritional balance, and a lower incidence of gestational diabetes mellitus. However, the multiparous showed healthier lifestyle habits (lower rates of smoking and alcohol consumption) and more physically active patterns. Regarding diet, nulliparous pregnant women consumed more dairy products, fresh fruit and nuts, and less bread, rice/pasta/potatoes, meat, sausage and buns/pastries than multiparous pregnant women.
Conclusions: Differences between analyzed patterns were observed in anthropometrical variables, lifestyle behaviors and dietary habits, which may require different nutritional messages to nulliparous as compared to multiparous from a public health point of view.
Key words: Pregnancy. Parity. Nutritional status. Lifestyle behaviours. Food habits.
RESUMEN
Fundamento: Durante el embarazo, el mantenimiento de un adecuado estado de salud y estilos de vida, es de gran importancia para prevenir resultados adversos tanto para la madre como para el bebé. El presente estudio tuvo como objetivos evaluar el estado nutricional, características sociodemográficas, estilos de vida y hábitos alimentarios de mujeres embarazadas en España, e identificar la influencia de la paridad sobre estos perfiles.
Material y método: Este estudio transversal incluyó mujeres embarazadas de todas las comunidades autónomas de España. La información se recogió a través de un cuestionario de 40 preguntas, previamente validado, por profesionales de la salud comunitarios.
Resultados: Las 5.087 mujeres embarazadas presentaron una edad media de 31,9 años y un adecuado estado nutricional. De la muestra un 56% fueron nulíparas y un 44% multíparas. Las mujeres nulíparas declararon mejor autopercepción de su estado de salud y estado nutricional, y menor incidencia de diabetes mellitus gestacional. Sin embargo, las mujeres multíparas mostraron estilos de vida más saludables (tasas de consumo de tabaco y alcohol más bajas) y un patrón de actividad física más activo. En cuanto a la dieta, las nulíparas consumieron más lácteos, fruta fresca y frutos secos, y menos pan, arroz/pasta/patatas, carne, embutidos y bollos/pasteles que las multíparas.
Conclusiones: Se observaron diferencias entre los grupos analizados en cuanto a variables antropométricas, estilos de vida y hábitos alimentarios, que pueden requerir distintos mensajes nutricionales para mujeres nulíparas y multíparas, desde un punto de vista de Salud Pública.
Palabras clave: Embarazo. Paridad. Estado nutricional. Estilos de vida. Hábitos alimentarios.
Introduction
Gestational state leads to anatomical, physiological and biochemical adaptive changes in order to ensure growth and development of the fetus. Thus, energy and most nutrient requirements are increased, so the nutritional status of the mother may be in risk1.
Energy undernutrition and micronutrient deficiencies have been related to adverse outcomes for both, mother and baby. Vitamin A, vitamin D, folic acid, vitamin B12 and other antioxidant vitamins are important for reproduction and later normal development of the fetus and the neonate. Moreover, some minerals of crucial interest during pregnancy are calcium, iron and iodine which are involved in maintaining the adequate nutritional status of the mother and the offspring2. On the other hand, maternal overweight and obesity are considered health risk factors for mother and fetus. Overweight women are more susceptible to suffer during pregnancy hypertensive events, pre-eclampsia, thromboembolic disorders, gestational diabetes mellitus (GDM), labour induction and caesarean delivery3,4. Furthermore, fetal problems include congenital malformations, macrosomia, stillbirth, shoulder dystocia and predisposition for adulthood diseases such as obesity, diabetes mellitus (DM), metabolic syndrome and cardiovascular disease3.
Drug-toxicant exposure has been shown to cause marked damage for mother and newborn. Thus, intrauterine growth restriction and low birth weight are the most common effects of maternal smoking, but there are other factors associated such as spontaneous miscarriages, effects on the placenta, structural malformations, stillbirth, sudden infant death syndrome, neurobehavioral effects and metabolic disorders including obesity, elevated blood pressure and DM. Fetal alcohol spectrum disorders is an umbrella term, which include birth defects caused by consumption of alcohol during gestation, including intrauterine growth restriction and developmental delay, among others5. Also, illicit drug exposure in pregnancy is associated with maternal and fetal morbidity5.
In the same way, regular physical activity has beneficial effects for both of them (mother and fetus). The main maternal benefits are the improvement of cardiovascular function, reduction of the incidence of metabolic diseases (GDM or pre-eclampsia) and regulation on the weight gain during pregnancy6. Regarding to the fetus, it has been reported that lower fat mass, greater stress tolerance and neurobehavioral maturation are some of the benefits associated to adequate physical activity during pregnancy6.
According to the afore mentioned pathophysiological conditions and lifestyle behaviors, previous studies suggest that parity can have an impact on them7,8. However, few studies have been performed in other behaviors of interest during pregnancy. Therefore, the two main aims of the present study were to assess the nutritional status, sociodemographic features, lifestyle behaviors and dietary habits of Spanish pregnant women and to identify the influence of parity on these profiles in order to provide specific messages for these two groups of pregnant women.
Material and Methods
Subject recruitment
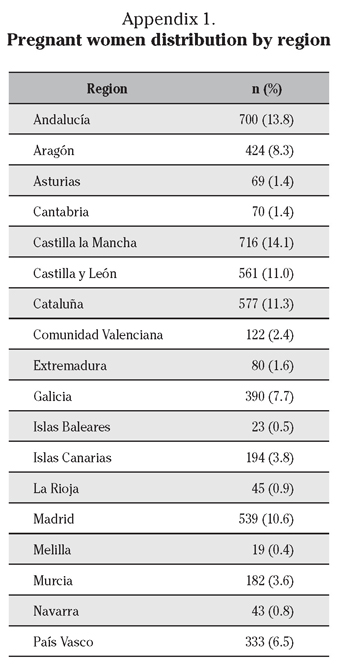
The current cross-sectional study was conducted between November 2009 and March 2010. The study population consisted of 5,087 pregnant women from regions all over Spain who participated in a national plan of nutritional education (Appendix 1). This program was performed in order to bring information, to preconceptional, pregnant and lactating women, about the importance of how lifestyles and dietary habits could influence the development and health of their children9. Participants were recruited by community pharmacists and were specifically asked if they would be willing to take part anonymously in the study. After ensuring that participants had understood the information, only those who voluntarily accepted were enrolled. Voluntary completion of the questionnaire was considered to imply verbal informed consent. The survey, which involved an observational questionnaire but not intervention, was conducted with the approval of the Spanish Council of Pharmacist and the board of the Institute of Food Sciences and Nutrition of the University of Navarra, according to the guidelines laid down in the Declaration of Helsinki for anonymous surveys10.
Previously, community pharmacists were recruited through the Spanish Pharmacists Council to collect data. In order to obtain consistent results to be compared among participants, all of the interviewers received a training session by videoconference or face to face, and the «application guide», an extensive document with basic information about the survey, which contained instructions to formulate and answer each question9. Later, each of the community pharmacists was evaluated throughout a knowledge assessment questionnaire, to test if they had understood the content of the questionnaire in a similar way. This information was also available for all pharmacists involved in the study in a website.
The nutritional survey
The nutritional questionnaire validated for nutritional status, physical activity profile and dietary habits of pregnant women (Appendix 2); included a total of 40 questions distributed into 6 sections: general information, obstetric data, breastfeeding intention (type and duration), unhealthy lifestyle habits, pathophysiological state and dietary habits11.
The section general information included anthropometrical measurements, data about self-perception of health status and nutritional balance, educational level and physical activity. The anthropometrical measurements were taken by community pharmacists (weight, height and middupper arm circumferece -MUAC-), whereas preconceptional weight was self-declared.Body mass index (BMI) was calculated dividing weight by the square of height. MUAC was measured between the acromion process of the humerus and the olecranon process of the ulna, with the arm relaxed alongside the body, using a flexible and inextensible measuring tape. Anthropometrical and physical activity data collection has been already validated elsewhere11. The validity of anthropometrical measurements was assessed by testing the accuracy of measurements collected by community pharmacists and comparing them to measurements collected by trained research staff11. The physical activity questionnaire, that collects the number of hours spent in lying, sitting and moving activities since women were pregnant, had demonstrated validity against other physical activity questionnaire previously validated11.
Obstetric data comprised the type of pregnancy (single or multiple pregnancy), gestational age, parity and previous miscarriages. Information about smoking, alcohol consumption and illicit drugs at the time of the interview was collected in the section concerning unhealthy lifestyle habits. Regarding to the section pathophysiological state, women were asked about suffering a severe disease, presence of GDM (with confirmed medical diagnosed) and follow a special diet (low calorie, low fat, low carbohydrates or low sodium diets, and any type of vegetarian diets).
Diet information was collected by a validated Food Frequency Questionnaire (FFQ) in which basic foods were classified into twelve food groups, where 4 responses were possible: daily, weekly, monthly or never11. Pregnant women were asked to report their food habits during pregnancy. The validity of this questionnaire was assessed against the validated FFQ of the SUN project (Seguimiento Universidad de Navarra project)11. The «application guide» included information on the typical serving size for each basic food9. In order to estimate if both groups fulfilled with the nutritional recommendations for Spanish pregnant women, bread and rice/pasta/potatoes were grouped as cereal products12; and nuts, pulses, fish, eggs and meat were grouped as protein products. Qualitative information about the consumption of supplements, fortified or functional foods was obtained using different categories.
Data collection
The questionnaire information was collected by face to face interviews by community pharmacists using a platform located in a website created for this study in order to save the information collected. The questionnaire was completed before the nutrition education. In fact, the nutrition education was based in the main errors identified throughout the questionnaire. Data were refined, processed and analyzed in an anonymous and confidential way. On the 5,711 questionnaires that were received from pregnant women, 624 (10.9%) were excluded because of missing values on important variables. The final sample for the analysis was 5,087. It should be noted that the number of cases differed for some of the variables as described (Fig. 1).
Statistical analyses
Means and standard desviations (SD) were used as descriptive statistics for age, weight, height, BMI, MUAC, physical activity and food habits. Student t tests were performed to compare means for these variables between nulliparous and multiparous women. General linear models of analysis of covariance (ANCOVA) were used to test the differences in quantitative variables by parity status with age, current BMI and gestational age as covariates. Frequencies and χ2 tests were used to compare different proportions of health, toxic habits and other food variables between both groups.
The statistical Package for Social Sciences (SPSS), version 15.0 for WindowsXP was used in the analyses. All p values presented are two-tailed and differences were considered significant at p<0.05.
Results
A total of 5,087 pregnant women were analyzed, who were distributed as 56% nulliparas and 44% multiparas. Age, gestational age and anthropometrical measurements (preconceptional weight, current weight, weight gain, height, preconceptional BMI, current BMI and MUAC) were studied (Table 1). The average maternal age of the sample was 31.9 ± 4.6 years, being lower the age at first maternity. Those nulliparous women presented lower values for preconceptional weight, current weight, preconceptional BMI, current BMI and MUAC after adjusted for age and gestational age. Statistical differences were also observed for the week of gestation, being nulliparous mothers whose showed low gestational age.
Obstetric data, health status and other related nutritional issues were also collected (Table 2). Nulliparous mothers showed better self-perceived health status and nutritional balance, presenting as well as less frequency of GDM. As expected, the frequency of previous miscarriage was higher among multiparas. Also, statistical differences were found for educational level between both conceptional conditions (nulliparas versus multiparas).
Smoking and alcohol consumption were more frequent among nulliparous women.However, this was not observed for declared illicit drugs (Table 3). Regarding to physical activity, some differences were noted, being physical activity patterns in multiparous women more active after adjusted for age, current BMI and gestational age (Table 3).
Interestingly, for food consumption statistical differences were observed in model 4 (adjusted forage, current BMI and gestational age) between the two groups (nulliparas versus multiparas) concerning dairy products, fresh fruit, bread, rice/pasta/potatoes, nuts, meat, sausage and buns/pastries (Table 4). The adherence to the recommended number of servings for the Spanish pregnant women was also analyzed. Both groups, consumed fewer servings of dairy products (2.26 servings/day), salads/vegetables (1.26 servings/day) and cereal products (2.39 servings/day) than the minimum recommendations: 3, 2 and 4 servings/day respectively (data not showed). On the other hand, statistical differences were found for the intake of olive oil and sweeteners (Table 5). Nevertheless, these differences were not detected regarding fortified food and nutritional supplements consumption except supplements of iron (Table 5).
Discussion
The results of this epidemiological research from 5,087 pregnant women showed differences between nulliparous and multiparous mothers regarding to nutritional status, sociodemographic features, lifestyle behaviors and dietary habits.
After adjusted for age and gestational age, the current differences on anthropometrical variables between the two different profiles of Spanish pregnant women were observed. The mean value of preconceptional body weight and BMI variables were in the normal range in both groups13,14. However, higher preconceptional body weight and BMI were found in multiparous women. This finding could be associated with the body weight retention in the postpartum period, which has been reported between 0.5 and 3.8 kg15. Moreover, multiparous women presented higher values of current weight and BMI than nulliparous women, although there were not found statistical differences between groups regarding to weight gain during pregnancy. In this sense, pre-pregnancy BMI, parity and weight gain during pregnancy have been identified as contributors of the increase of the prevalence of overweight and obesity among women3.
Besides the weight and BMI, MUAC is another anthropometrical measurement ofinterest during pregnancy, mainly because of its relationship with low birth weight (<2,500g) but also with disproportionate low intrauterine growth, preterm birth/labor, birth asphyxia and small for gestational age16. A recent systematic review showed that, regarding to low birth weight, most of the studies used MUAC cutoffs ranging from 22 to 24 cm16. However, we can not compare our results with these studies since they did not include European populations.
Educational level and other socioeconomic features have an impact on maternal and child health17. A high level of education implies a better access and understanding of the information about the benefits of following healthy habits during pregnancy17. In our research, there were a lower percentage of multiparas with a university degree than nulliparas. So, it can be speculated that multiparous mothers and their offsprings are more vulnerable to present adverse health effects.
The results of the subjective assessment (self-perception of the global health status and nutritional balance) appear to be in accordance with the results obtained later related to special diet consumption. Multiparas presented worse self-perception in health status and nutritional balance, probably thus they followed more a special diet compared with nulliparas.
In our research, the prevalence of GDM was higher in multiparous women than in nulliparous once. In one hand, a previous research found that women with GDM in their first pregnancy were at increased risk for developing GDM in their subsequent pregnancies7. This study also observed that the risk of GDM is higher in subsequent pregnancies. On the other hand, has been reported that women who gain more BMI units between their first and second pregnancy showed a higher risk of developing GDM in their second pregnancy18. In accordance with these evidences, we noted that multiparous women presented higher prepregnancy and current BMI than nulliparous women. Moreover, parity plays a key role in the development of GDM. So, it may be suggested that the high prevalence of GDM in multiparas could be due to the parity and the higher prepregnancy and current BMI of this group of pregnant women.
Regarding to lifestyle habits, there were several differences between the two profiles analyzed, being multiparous women the group that presented healthier behaviors. In our research contrasting with previous investigations in Spanish pregnant women, multiparous mothers smoked less than nulliparous19,20. Also, alcohol and illicit drugs consumption was lower among multiparous women, although concerning illicit drugs not statistical differences were observed. The results about these three lifestyle habits may be related, given that the research of Erickson et al21 supported that heavy smokers have an increased risk of being identified for alcohol and illicit drug use.
In a different way, after adjusted for age, current BMI and gestational age, we observed that nulliparous women were more sedentary than those multiparous. Our findings about the hours lying or sleeping are in accordance with the research of Borodulin et al in which nulliparous women reported longer sleep duration and better sleep quality22. Moreover, a recent study of 1,259 pregnant women found that multiparous mothers had higher odds of participating in strenuous physical activity and they also reported a lower decrease in physical activity level during pregnancy than nulliparous mothers8.
To our knowledge, there are few studies that analyzed the differences in the type of food intake by parity23-26. In general, in our population (after adjusted for age, current BMI and gestational age) nulliparas followed a healthier diet than multiparas, which is consistent with other findings reported on a healthy conscious diet (characterized by a high consumption of vegetables, fruits, cereals, fish and pulses) is negatively associated with increased parity23. Moreover, a caloric diet pattern has been positively associated with parity24. In this context, nulliparous mothers consumed healthier food groups as fruits25, dairy products, nuts and olive oil, but also more caloric sweeteners. On the other hand, multiparas women consumed more energy-dense and rich in unhealthy fat food groups than nulliparas, as meat, sausages26, and buns/pastries, but also more rice/pasta/potatoes and bread. Although the differences among diet intake were statistically significant, we could not consider them clinically relevant from a dietary point of view.
When the dietary consumption was compared with the recommendations for Spanish pregnant women, it was observed a lower intake of dairy products, salads/vegetables and cereal products than it is recommended12. Different studies have been carried out to determine the adherence to the dietary recommendations in pregnant women. Similarly to our results Ferrer et al showed that cereals, vegetables and pulses consumption was below the portions recommended, among Spanish pregnant women24. Additionally, Wilkinson et al reported that the consumption of vegetables and also fruits was below the daily portions recommend in Australian pregnant women27. In contrast, Ortiz-Andrellucchi et al found in a Spanish population that pregnant women consumed more vegetables, fruit, milk and meat products than the recommendations, but less cereals28. However, these data can not be strictly compared with each other because each country (or group of countries) has their own recommendations, even there is more than one organism that stablishs different dietary references within the same country, as in Spain1.
Finally, concerning supplementation there were not statistically significant differences in any type of supplement except in iron, being multiparous mothers those who consumed more. This outcome may be explained because anaemic pregnant women are administered more iron supplements. However, few studies concluded that parity is associated with anaemia, although Bencaiova et al reported that it is a risk factor of decreasing of iron stores29.
The present study has some limitations. The main one is the origin of the recruitment of the volunteers (pharmacies), which may have resulted in a not totallyrepresentative sample. However, the large sample size should support the validity of our investigation as well as the low margin of error in this population. And the fact that this enrollment protocol has been previously applied in prior studies30. Another limitation is the gestational age variability between groups; nevertheless we adjusted all of our analysis for this variable, and also for age and current BMI. In order to implement the nutritional questionnaire, community pharmacists received a training session by videoconference or face to face. Although the interviewers received the information by two different ways, all of them received the same application guide to give consistency to the survey. Moreover, we recognize that the statistical differences in the intake of some groups of food by parity are small. Nonetheless, these findings provide an overview of the trends in the consumption of certain type of foods, among Spanish pregnant women. In spite of these limitations; the strength of our study is that we used a FFQ and physical activity questionnaire both validated specially for the target population group11. Furthermore, the main anthropometric measurements have also been validated11.
In summary, differences associated to parity were observed in nutritional status, sociodemographic features, lifestyle behaviors, and dietary habits. Multiparous women presented healthier lifestyle behaviors and a more active physical activity pattern than nulliparous. However, nulliparous women consumed more foods rich in vitamins and minerals (dairy products and fruit), while multiparous intaked more rich energy-dense foods (meat, sausage, buns/pastries). Thus, these findings provide some insights into the design of programs aimed at promoting healthy lifestyles habits during pregnancy according to parity.
Acknowledgements
The authors thank all the pharmacists that participated in the data collection and the women who agreed to participate voluntarily in this study. The authors also wish to thank the CIBERobn/RETICS schedules (Instituto Carlos III) assistance in this study.
References
1. Cuervo M, Baladia E, Goñi L, Corbalán M, Manera M, Basulto J, et al. Propuesta de ingestas dietéticas de referencia (IDR) para la población española. In: Federación Española de Sociedades de Nutrición, Alimentación y Dietética (FESNAD), editor. Ingestas Dietéticas de Referencia (IDR) para la población española. España: EUNSA; 2010:263-341. [ Links ]
2. Hovdenak N, Haram K. Influence of mineral and vitamin supplements on pregnancy outcome. Eur J Obstet Gynecol Reprod Biol 2012; 164:127-32. [ Links ]
3. Melzer K, Schutz Y. Pre-pregnancy and pregnancy predictors of obesity. Int J Obes (Lond) 2010; (Suppl. 2): 44-52. [ Links ]
4. Huarte Ciganda M, Modroño A, Larrañaga C. Management of hypertension in pregnancy. An Sist Sanit Navar 2009;32 (Suppl 1): 91-103. [ Links ]
5. Wendell AD. Overview and epidemiology of substance abuse in pregnancy. Clin Obstet Gynecol 2013; 56: 91-96. [ Links ]
6. Melzer K, Schutz Y, Boulvain M, Kayser B. Physical activity and pregnancy: Cardiovascular adaptations, recommendations and pregnancy outcomes. Sports Med 2010;40:493-507. [ Links ]
7. Getahun D, Fassett MJ, Jacobsen SJ. Gestational diabetes: Risk of recurrence in subsequent pregnancies. Am J Obstet Gynecol 2010;203:467. [ Links ]
8. Liu J, Blair SN, Teng Y, Ness AR, Lawlor DA, Riddoch C. Physical activity during pregnancy in a prospective cohort of British women: Results from the Avon Longitudinal Study of Parents and Children. Eur J Epidemiol 2011;26:237-247. [ Links ]
9. IV plan de educación nutricional en el periodo pre-concepcional, embarazo y lactancia (Internet). Available from: http://www.portalfarma.com/Profesionales/campanaspf/categorias/Paginas/Alimentacion/planeducacionplenufar4.aspx. (Accessed 30/03/2014). [ Links ]
10. World Medical Association. World medical association declaration of helsinki: Ethical principles for medical research involving human subjects. JAMA 2013;310:2191-2194. [ Links ]
11. Goni L, Martínez JA, Santiago S, Cuervo M. Validation of a questionnaire to assess the nutritional status and lifestyles in stages of preconception, pregnancy and lactation. Rev Esp Nutr Comunitaria 2013; 19:105-113. [ Links ]
12. Dapcich V, Salvador G, Ribas L, Pérez C, Aranceta J, Serra L. Guía de la alimentación saludable. Madrid; 2004. [ Links ]
13. Ricart W, Gonzalez-Huix F, Conde V. Evaluation of the nutritional status through determination of anthropometric parameters: New charts for the working population of Catalonia. group for the evaluation of body composition in the population of Catalonia. Med Clin (Barc) 1993; 100:681-691. [ Links ]
14. Rubio MA, Salas-Salvadó J, Barbany M, Moreno B, Aranceta J, Bellido D, et al. Consenso SEEDO 2007 para la evaluación del sobrepeso y la obesidad y el establecimiento de criterios de intervención terapéutica. Rev Esp Obes 2007: 1: 7-48. [ Links ]
15. Linne Y, Rossner S. Interrelationships between weight development and weight retention in subsequent pregnancies: The SPAWN study. Acta Obstet Gynecol Scand 2003;82:318-325. [ Links ]
16. Tang AM, Dong K, Deitchler M, Chung M, Maalouf-Manasseh Z, Tumilowicz A, et al. Use of cutoffs for mid-upper arm circumference (MUAC) as an indicator or predictor of nutritional and health-related outcomes in adolescents and adults: A systematic review. Washington, DC, 2013. [ Links ]
17. Larranaga I, Santa-Marina L, Begiristain H, Machon M, Vrijheid M, Casas M, et al. Socio-economic inequalities in health, habits and self-care during pregnancy in Spain. Matern Child Health J 2013; 17: 1315-1324. [ Links ]
18. Ehrlich SF, Hedderson MM, Feng J, Davenport ER, Gunderson EP, Ferrara A. Change in body mass index between pregnancies and the risk of gestational diabetes in a second pregnancy. Obstet Gynecol 2011;117:1323-1330. [ Links ]
19. Palma S, Perez-Iglesias R, Pardo-Crespo R, Llorca J, Mariscal M, Delgado-Rodriguez M. Smoking among pregnant women in Cantabria (Spain): Trend and determinants of smoking cessation. BMC Public Health 2007;7:65. [ Links ]
20. Villalbi JR, Salvador J, Cano-Serral G, Rodriguez-Sanz MC, Borrell C. Maternal smoking, social class and outcomes of pregnancy. Paediatr Perinat Epidemiol 2007;21:441-447. [ Links ]
21. Erickson AC, Arbour LT. Heavy smoking during pregnancy as a marker for other risk factors of adverse birth outcomes: A population-based study in British Columbia, Canada. BMC Public Health 2012;12:102. [ Links ]
22. Borodulin K, Evenson KR, Monda K, Wen F, Herring AH, Dole N. Physical activity and sleep among pregnant women. Paediatr Perinat Epidemiol 2010;24:45-52. [ Links ]
23. Northstone K, Emmett P, Rogers I. Dietary patterns in pregnancy and associations with socio-demographic and lifestyle factors. Eur J Clin Nutr 2008;62:471-479. [ Links ]
24. Ferrer C, García-Esteban R, Méndez M, Romieu I, Torrent M, Sunyer J. Social determinants of dietary patterns during pregnancy. Gac Sanit 2009;23:38-43. [ Links ]
25. Bodnar LM, Siega-Riz AM. A diet quality index for pregnancy detects variation in diet and differences by sociodemographic factors. Public Health Nutr 2002; 5:801-809. [ Links ]
26. Uusitalo L, Uusitalo U, Ovaskainen ML, Niinisto S, Kronberg-Kippila C, Marjamaki L, et al. Sociodemographic and lifestyle characteristics are associated with antioxidant intake and the consumption of their dietary sources during pregnancy. Public Health Nutr 2008;11:1379-1388. [ Links ]
27. Wilkinson SA, McIntyre HD. Evaluation of the «healthy start to pregnancy» early antenatal health promotion workshop: A randomized controlled trial. BMC Pregnancy Childbirth 2012;12: 31. [ Links ]
28. Ortiz-Andrellucchi A, Sanchez-Villegas A, Ramirez-García O, Serra-Majem L. Assessment of nutritional quality in healthy pregnant women of the Canary Islands, Spain. Med Clin (Barc) 2009;133:615-621. [ Links ]
29. Bencaiova G, Burkhardt T, Breymann C. Anemia-prevalence and risk factors in pregnancy. Eur J Intern Med 2012;23:529-533. [ Links ]
30. Cuervo M, García A, Ansorena D, Sánchez-Villegas A, Martínez-González M, Astiasarán I, Martínez JA. Nutritional assessment interpretation on 22,007 Spanish community-dwelling elders through the Mini Nutritional Assessment tes. Public Health Nutr 2009; 12: 82-90. [ Links ]
![]() Correspondence:
Correspondence:
J. Alfredo Martínez
Department of Nutrition, Food Sciences and Physiology
University of Navarra
Irunlarrea, 1
31008 Pamplona.Navarra.Spain
E-mail: jalfmtz@unav.es
Recepción: 16 de abril de 2014
Aceptación provisional: 30 de junio de 2014
Aceptación definitiva: 1 de septiembre de 2014





















