Introduction
The probabilities of surviving after out-of-hospital cardiac arrest (OHCA) depend on many factors, but high quality resuscitation performed by witnesses or bystanders before ambulance arrival is regarded as the intervention that, regardless of other measures, has the greatest influence on the prognosis of a cardiac arrest (CA)1.
However, the likelihood of finding someone who can carry out basic CPR when the first healthcare resource arrives is not very high. In fact, barely 20 % of Basque citizens consider themselves to be skilled in performing CPR and nearly 40 % would not know how to identify a public-access automatic external defibrillator2. In addition, the causes that may be associated with a person deciding whether to CPR before the arrival of healthcare personnel are many and varied and have been little researched in Spain.
The objectives of this paper focus on comparing the existing epidemiological differences between out-of-hospital cardiac arrests that require resuscitation, depending on whether CPR was initiated by bystanders, and to describe the associated factors in the Basque Country at the start of resuscitation before the arrival of the ambulance.
Methods
A retrospective analytical observational study, limited to the Basque Autonomous Community. The study was approved by the Ethics Committee on Clinical Research of Euskadi.
All the OHCA situations that required resuscitation with assistance from basic and/or advanced life support ambulances of the emergency care system between June 2013 and May 2018 were included. The CAs that occurred in any out-of-hospital health centre (including ambulances) or nursing homes were excluded. No situations of OHCA requiring resuscitation were considered when they dealt with the final phase of a terminal illness or when there were indications that the resuscitation manoeuvres were futile, or there were evident signs of impending death or conditions incompatible with life.
The clinical and demographic information of the cases was extracted from the OHCA database managed by Emergentziak-Osakidetza and constructed from the standardized documentation according to the Utstein style and supplied by the resources of the Emergency Medical System (EMS) and/or recorded in the patient's computerized clinical records.
Information about the patients was gathered (gender: male, female; and age: < 65, ≥ 65 years) along with data about the event location (urban setting: density > 200, non-urban: ≤ 200 inhabitants/km2), site (home, other), date and time of the event (daytime: 8:00-22:00, night time: 22:00-8:00), the presence or absence of witnesses, and whether there was a telephone dispatcher-assistance available for initiating resuscitation. Data on the initial electrocardiographic rhythm detected by the first healthcare resource to arrive (defibrillable or not defibrillable) were also extracted, as well as the final resolution of the case evaluated in terms of mortality and survival upon release, with neurological evaluation according to the Glasgow-Pittsburgh Cerebral Performance Categories scale (exitus in the first 24h, exitus during hospitalization, release without disability or mild disability, release with severe or very severe disability) as well as the timeframe of the response intervals. A dependent variable is considered to be any attempt to resuscitate by witnesses or bystanders before the healthcare resource arrives.
The characteristics of the sample were described by means of absolute frequencies and percentages for the qualitative variables, and median (Me) and interquartile range (IQR) for the quantitative variables. The medians were compared with the Mann Whitney U test, and the association between the qualitative variables was determined with the Chi-square test. The magnitude of the association between different exposure factors and the dependent variable was estimated by the odds ratio (OR) and the confidence intervals at 95 % (95 %CI) provided by the multivariate logistics regression model which included those qualitative variables that showed statistical significance in the bivariate analysis. Statistical analyses were performed using SPSS 25. A p-value < 0.05 was considered statistically significant.
Results
In the study period, 4,204 requests for OHCA were attended by the EMS, of which 697 were rejected for resuscitation due to the CPR not being regarded as indicated. After ruling out the events with exclusion criteria, the study was conducted on a total of 3,278 cases of CA requiring resuscitation, where 1,250 (38.1 %) received aid from first responders before the arrival of the ambulance. In 85 % of the events, resuscitation manoeuvres were carried out by a bystander and the remaining 15 % by police or public workers on duty. In 2,471 (75.4 %) cases, the CA was witnessed, and CPR commenced before the arrival of the healthcare team in 44.5 % of cases. The flow chart of inclusion of cases in the study is shown in Figure 1.
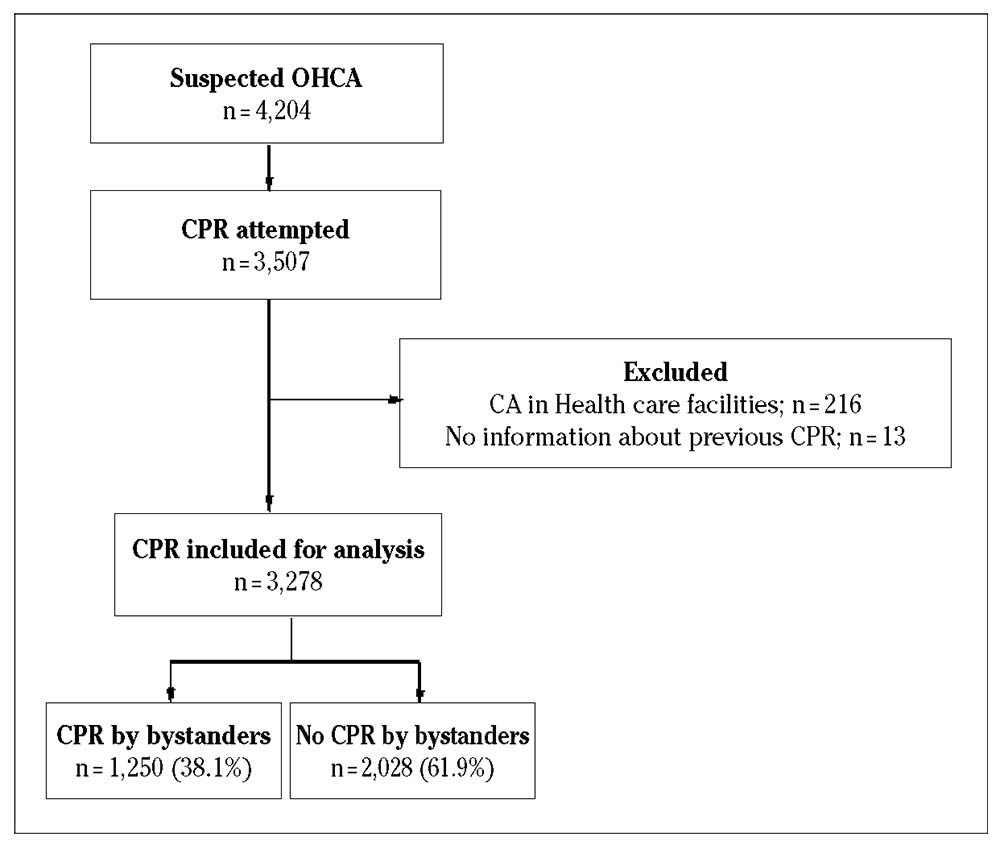
OHCA: out-of-hospital cardiac arrest; CPR: cardiopulmonary resuscitation; CA: cardiac arrest.
Figure 1. Flow chart of inclusion of cases in the study.
A statistically significant association (p < 0.001) was observed among the CA was not attended by a witness or bystander before the arrival of the healthcare resource and patients who were female or over 64 years of age, the event happening in the patient's usual residence or in the daytime, the CA was not witnessed and no telephone dispatcher-assistance was offered in order to start CPR. Furthermore, the CAs not attended by bystanders presented a lower proportion of defibrillable rhythms when the ambulance arrived, a longer clinical response time from activation of the EMS until commencement of life support manoeuvres and a more unfavourable clinical evolution (Table 1). The distribution of cases by age is shown in Figure 2.
Table 1. Characteristics of the events studied according to whether or not cardiopulmonary resuscitation was practiced by witnesses or bystanders prior to the arrival of the first healthcare resource (n = 3,278)
| Total | Prior CPR | p (χ2) | Data not recorded | ||
|---|---|---|---|---|---|
| No | Yes | ||||
| n (%) | n (%) | n (%) | n | ||
| Patient characteristics | |||||
| Age (years)* | 68 (55-79) | 71 (58-81) | 63 (52-76) | < 0.001 | 0 |
| Age ≥65 years | 1873 (57.1) | 1281 (63.2) | 592 (47.4) | < 0.001 | 0 |
| Female | 868 (26.5) | 580 (28.6) | 288 (23) | < 0.001 | 0 |
| Characteristics of cardiac arrest | |||||
| Night-time (22:00-8:00) | 835 (25.8) | 562 (28.1) | 273 (22.1) | < 0.001 | 40 |
| Urban setting | 2813 (85.8) | 1773 (87.4) | 1040 (83.3) | 0.001 | 1 |
| At home | 2156 (65.8) | 1490 (73.5) | 666 (53.3) | < 0.001 | 0 |
| Not witnessed | 759 (23.5) | 523 (26.3) | 236 (19) | < 0.001 | 48 |
| Telephone dispatcher-assisted CPR | 2495 (77.6) | 1766 (88.6) | 729 (59.6) | < 0.001 | 61 |
| Evolution of the cardiopulmonary resuscitation | |||||
| First non-defibrillable rhythm detected | 2450 (74.7) | 1648 (81.3) | 802 (64.2) | < 0.001 | 0 |
| Time (minutes:seconds) from activation of the EMS until the start of LS* | 11:00 | 10:00 | 09:00 | < 0.001 | |
| (9:00-15:00) | (8:00-14:00) | (7:00-11:00) | |||
| Time (minutes:seconds) from start of LS until ROSC* | 21:00 | 24:00:00 | 21:00 | 0.714 | |
| (13:00-30:00) | (14:30-30:00) | (14:30-30:00) | |||
| Outcome | |||||
| Exitus in the first 24h | 2677 (85.5) | 1757 (89.6) | 920 (78.8) | < 0.001 | 148 |
| Exitus during hospitalization | 218 (7) | 125 (6.4) | 93 (8) | ||
| Release with CPC 1-2 | 212 (6.8) | 69 (3.5) | 143 (12.2) | ||
| Release with CPC 3-4 | 23 (0.7) | 11 (0.6) | 12 (1) | ||
CPR: cardiopulmonary resuscitation; χ2: Chi-square; *: median (interquartile range), compared by Mann Whitney U test; EMS: Emergency Medical Service; LS: life support manoeuvres carried out by the first healthcare resource; ROSC: return of spontaneous circulation; CPC: clinical condition of the patient evaluated according to the Glasgow-Pittsburgh Cerebral Performance Categories scale, 1-2 = without disability or mild disability, 3-4 = severe disability or very severe.
Table 2. Predictors of not performing cardiopulmonary resuscitation prior to the arrival of the first healthcare resource by means of a multivariate logistics regression model
| Variables | OR | 95 %CI | p |
|---|---|---|---|
| No telephone dispatcher-assistance | 6.25 | 5.15-7.58 | < 0.001 |
| CA at home | 2.94 | 2.48-3.48 | < 0.001 |
| CA not witnessed | 1.56 | 1.28-1.89 | < 0.001 |
| Age ≥ 65 years | 1.48 | 1.26-1.74 | < 0.001 |
| Urban setting | 1.29 | 1.04-1.62 | 0.023 |
OR: odds ratio; 95%CI: confidence interval at 95 %; CA: cardiac arrest.
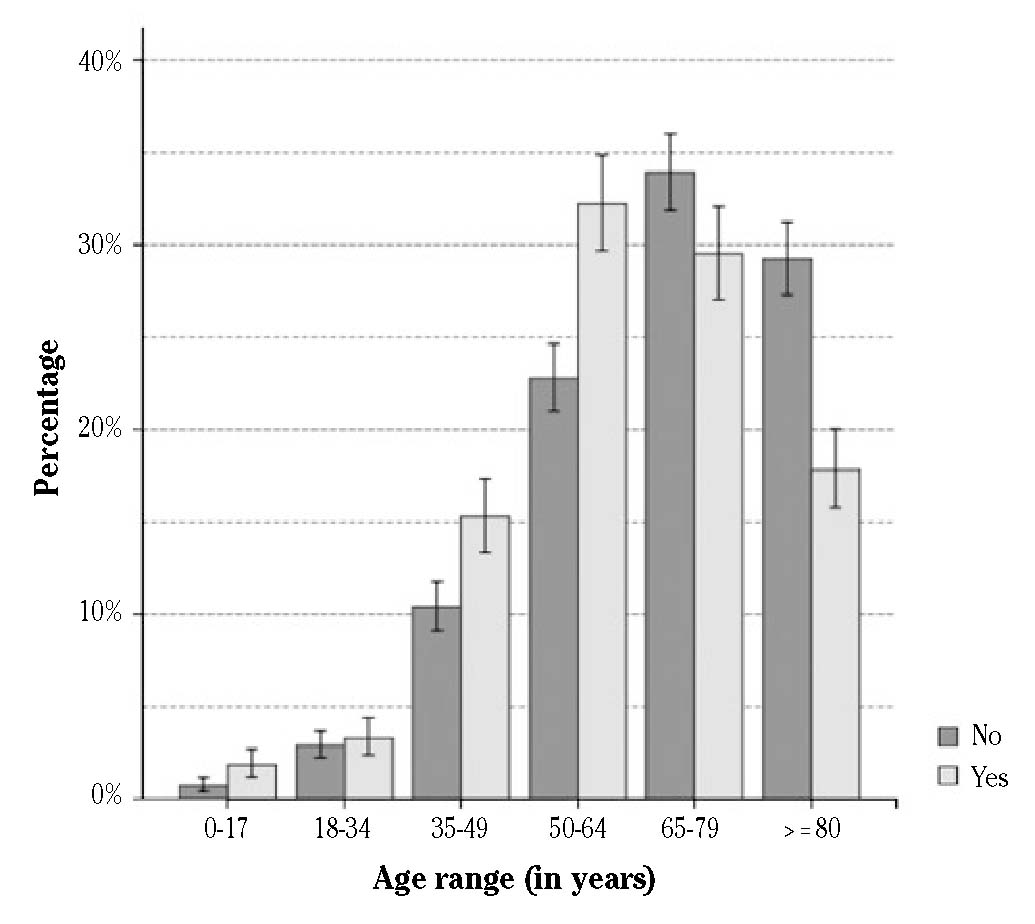
Figure 2. Proportion of cardiac arrests assisted by witnesses or bystanders before the arrival of the first healthcare resource by age ranges of the victim. Bar graph with 95% confidence intervals.
In the logistical regression model, seven independent variables were entered (age, sex, town, location of the event, time (day or night), whether the CA was witnessed and if telephone instructions were offered), of which five were found to be statistically significant (Table 2). The factors most strongly associated with no one starting CPR before the healthcare team were the absence of telephone instructions by the EMS (OR: 6.25; 95 %CI: 5.15-7.58), and that the event took place in the home (OR: 2.94; 95 %CI: 2.48-3.48).
Discussion
This paper highlights the existence of differentiated characteristics in CAs according to whether or not CPR was started by witnesses or bystanders before the ambulance arrived. These characteristics may be interpreted as factors that can determine the decision of a potential rescuer to attempt resuscitation and that will also condition the evolution of the event.
In our series, limited to cases that occurred in the Basque Country over a five-year period, the proportion of CPRs initiated by bystanders was estimated at 38.1%. This proportion is higher than the ones documented by other older series coming from the same3 and other Spanish autonomous communities4, with figures at around 20 %. This difference seems to indicate a good increase in first-aid knowledge and/or awareness of CA in the population, probably related to the gradual adoption of political and technical measures such as the regulation of training, authorization and installation of external automatic defibrillators outside the healthcare setting5 or a gradually growing number of initiatives aimed at implementing teaching of basic CPR in schools6, among others.
Studies that have specifically explored the factors associated with bystanders initiating CPR are not abundant, and, although their findings are similar to those reported in our context7,8, the results in this paper show some noteworthy differences. For example, in Germany a lower probability of resuscitation was reported when the CA is witnessed9, attributed to the confusion that agonal breathing can generate. The indications of a lower probability of being resuscitated when the CA occurs in a suburban area may also be highlighted. It is still within the limit of statistical significance, unlike in other European reports10. Perhaps an expected delay in the arrival of the ambulance (whose bases are more frequently located in urban areas) encourages the initiation of CPR by bystanders. In any case, any of these situations merit a differentiated and more detailed analysis.
The multivariate analysis excluded the patient's sex variable from the model, which may represent the most noteworthy difference in comparison to the findings of other foreign studies11,12, where a lower probability of being resuscitated before the ambulance arrives if the victim is female has been described. It has been speculated that this difference could be due to sociocultural or economic causes between regions13,14. The effect of rotating shifts was not a predictive factor either, contrasting with other studies15 in which a lower proportion of resuscitations initiated by bystanders in night time hours was observed.
It is noteworthy that telephone instructions are the variable that most seems to influence the initiation of CPR without waiting for the arrival of the emergency services, since it is the only independent predictor that has the possibility of intervention. The need/opportunity that the telephone instructions offer to guide CPR has been known for decades16, although in Spain it was not until 2015 when the first recommendations for telephone support to CPR from the emergency coordination centres was agreed17, although, by then some EMS already had specific internal protocols18. In fact, telephone instructions appear to still be in the process of consolidation, in view of the discrete rate of guided CPR shown in our study.
Lastly, and as expected, since the survival after CA is time-dependent, the evolution of the CA resuscitated early by bystanders was more favourable: they presented a lower prevalence of rhythms not requiring defibrillation, lower response times and a lower rate of immediate mortality.
This study has some limitations which need to be considered. Firstly, it was limited to a certain geographical area (Basque Country). Therefore, the external validity of the results must be taken with caution. Secondly, the personal characteristics or prior knowledge of the first person to respond was not considered; neither was the socioeconomic level of the neighbourhood where the CA took place. Some authors have confirmed that these variables could affect the initiation of CPR manoeuvres by citizens7. On the other hand, since it is known that quality CPR maximizes the probabilities of recovery, in our study the quality of the CPR practiced by the first responders was not assessed. The quality of the telephone instructions supplied by the EMS was not evaluated either. Nonetheless, previous studies lead us to presume that the quality of the resuscitation manoeuvres or the telephone instructions were suboptimal19,20,21. Finally, the variable corresponding to the presumable aetiology of the CA was not introduced in our model. This limitation responds to the fact that this variable was not included in a uniform or standardized manner in the analysed records and the retrospective characteristics of this study made the options of recovering this information impossible.
In conclusion, this paper shows that there are differences in the characteristics of cardiac arrests according to whether or not CPR was initiated by witnesses or bystanders. Given that these characteristics could have an influence on the decision of the potential rescuer to begin resuscitation and therefore on its evolution, the data from this study point towards the need to adopt measures to improve OHCA care. The strategy which shows the greatest impact is highlighted here, and is one of the few variables where we would be able to play a part: the program of telephone dispatcher-assistance for CPRs from emergency coordination centres.














