Introduction
Limping in children can be caused by multiple traumatic, infectious, or oncologic processes, which may affect any site of the lower extremities, pelvis, and lumbar spine. Growth disorders, osteonecrosis, and osteochondrosis are common childhood diseases that cause limping1,2.
Primary osteonecrosis is a disorder of the ossification center in children. The most frequent types of avascular necrosis of the foot among this population are calcaneal apophysitis (Sever’s disease), necrosis of the tarsal navicular bone (Köhler’s bone disease), necrosis of the second metatarsal head (Freiberg’s disease), and apophysitis of the fifth metatarsal base (Iselin’s disease), all of which can be clearly recognized clinically and radiologically1,2. Other similar but less frequent entities have also been described in midfoot and cuneiform bones1,2. Osteonecrosis typically resolves spontaneously, except when it affects metatarsal (MTT) heads, as they bear significant load. A diagnosis is often made because of the pain experienced by the patient during the necrosis and fragmentation phases2.
Avascular necrosis of the first MTT bone is an exceptional condition that affects the head or distal epiphysis of the first MTT bone in children. In adults, it is usually an iatrogenic condition caused by vascular injury when performing distal osteotomy of the first metatarsal in the correction of hallux valgus3. Involvement of the proximal epiphysis of the first metatarsal bone is exceptional; to date, one case -in a 6-year-old child- has been described by Souverijns et al.4. Those authors claim that Wagner reported the first description in 1930, although no radiological images were provided. Therefore, to the best of our knowledge, we present the second case of this clinical entity in the literature and the first in the orthopedic literature.
We describe a case of avascular necrosis (AVN) of the proximal epiphysis of the first MTT, a rare cause of childhood limping that requires a high index of suspicion in order to establish the diagnosis. Knowledge of the clinical and radiological progression is important to ensure adequate management of the lesion.
Case report
A boy aged 10 years and 4 months, taken to an outpatient clinic, had an 8-month history of limping due to pain in the dorsal-medial area of the right midfoot. The patient presented with local swelling and tenderness to palpation, which caused limping and antalgic gait with internal rotation of the foot. There were no signs of phlogosis, bruising, erythema, warmth, or fever. The hematological analysis showed no abnormalities.
X-ray images revealed widening of the proximal epiphysis of the first MTT bone. A month later, fragmentation in the proximal epiphysis of the first right MTT bone was observed, with low-density and sclerosis areas (Fig. 1).

Figure 1. Initial X-ray view, at nine years of age, showing signs of avascular necrosis of the proximal epiphysis of the first metatarsal bone (arrow). Fragmentation and sclerosis are seen (arrow). A. Anteroposterior projection. B. Oblique view.
One month after the initial consultation, MRI showed changes in epiphyseal density, decreased epiphyseal width (collapse) with widening, and high-/low- density areas consistent with avascular necrosis (Fig. 2). Bone scintigraphy was not considered, as X-rays and MRI were sufficient to ascertain the diagnosis.
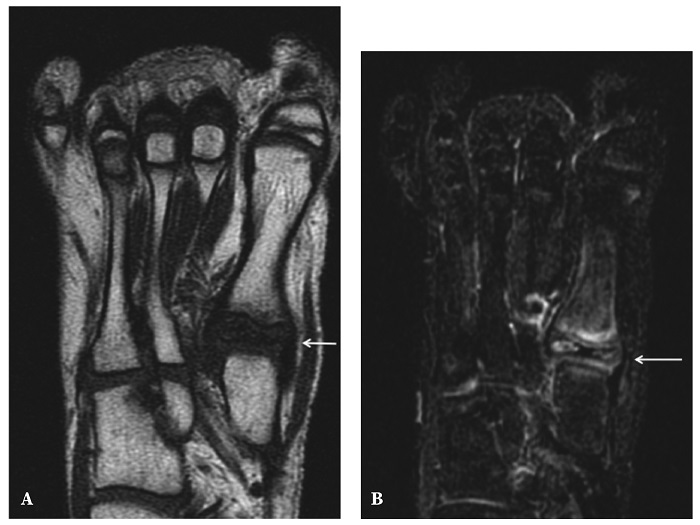
Figure 2. Magnetic resonance images one month after the onset of the symptoms. Changes in proximal epiphyseal density, reduced epiphyseal width (collapse), and enlargement with hyper- and hypodense areas are seen, consistent with avascular necrosis (arrows). A. T1-weighted image. B. T2 FSE (fast spin-echo) weighted fat saturated image.
No treatment was prescribed. The patient was only asked to avoid any physical activities that could increase the load on the foot. Symptoms gradually subsided spontaneously within six weeks and tenderness to palpation disappeared after four months. Five months later, X-ray images were normal, the patient was asymptomatic and practicing sports.
Four years later (at age 14 years and 7 months), he recovered his normal life -including athletic activities- free from symptoms. Both the footprint and the hind foot were normal and symmetrical. Deep palpation of the proximal epiphysis of the first right MTT bone caused no pain or tenderness. X-ray images at this age showed no anomalies except a slight residual proximal epiphyseal enlargement of the first MTT bone (Fig. 3).
Discussion
Osteonecrosis and osteochondrosis present with the typical radiological signs of osteonecrosis (fragmentation, sclerosis, collapse in some loading sites, and ultimately reossification); however, osteonecrosis generally develops in adulthood, whereas osteochondrosis occurs in the epiphyseal or apophyseal centers of immature bone5. To date, both terms are used interchangeably.
There are four types of osteochondrosis:
Physiological variations of ossification; usually asymptomatic with an ongoing debate as to whether it may occasionally cause symptoms1;
Changes related to bone trauma or excessive stress caused by overuse injuries or microtrauma due to repeated injuries seen in very active children;
Primary or secondary osteonecrosis due to processes involving blood supply, including traumatic or iatrogenic disruption of blood vessels, and arterial or venous intraluminal obstructions due to haemoglobinopathies or thromboembolic disorders, which cause necrosis due to local infarction from increased intramedullary pressure and venous occlusion;
Idiopathic or primary osteonecrosis, as described by Souverijns et al.4 in a reported case.
The etiology and pathophysiology of osteonecrosis remain unclear. It is speculated that the disease is triggered by the disruption of blood flow to the growth cartilage, followed by local disruption of endochondral ossification, mechanical stress, trauma, rapid growth (as occurred in our patient), anatomical conformation, and other processes that change bone´s normal structure.
Episodes of mechanical stress or microtrauma to the ossification centers have been pointed as an important factor in the development of necrosis in some bones of the hand5,6 and foot7,8, although Stanley et al.9 claimed that only 5% of cases of Freiberg’s disease could be attributed to trauma. Venous congestion, rather than arterial insufficiency, is a primary factor6; however, in other locations such as in the case of Legg-Calve-Perthes disease, it is not presently clear whether intraosseous hypertension is a final outcome or the primary cause of the disorder. Therefore, multiple etiological factors are involved in AVN of foot bones.
AVN may develop in foot bones, e.g., navicular and cuneiform bone, in which the onset of ossification occurs after walking age and before undergoing the stress of walking. Therefore, ossification prior to that age (as in the case of calcaneus, cuboid, and talus bones) seems to be a protective factor2.
In AVN, ischemic adipose cells transform into fibroblasts, and inflammatory cells transform into osteocytes. Hyperaemia and invasion of inflammatory cells cause local osteoporosis, while the infarcted areas remain denser. On X-rays, these are seen as hypodense and hyperdense areas, the typical radiographic presentation of osteonecrosis. Collapse occurs when there is subchondral resorption, as observed in the femoral head and MTT bone.
When a fused cartilage is affected, MRI may detect changes at an early stage10. In our case, as well as in that reported by Souverijns et al.4, MRI was useful for confirming the existence of osteochondrosis lesions (sclerosis, fragmentation, collapse, and later reossification). For an early diagnosis, MRI would be indicated when there is clinical suspicion for AVN but no radiological changes are already visible. Souverijns et al.4 made the initial diagnosis based on radiographs and confirmed it by MRI and scintigraphy. In our case, X-rays and MRI were sufficient; no complementary tests are necessary to achieve the diagnosis.
Epiphyseal AVN of the first MTT bone is a key element for the differential diagnosis of limping and foot pain in growing children. We ruled out other potential diagnoses, e.g., osteomyelitis, sickle cell disease, or childhood leukemia; clinical symptoms and signs, radiology, and prognosis are different in these conditions.
We are uncertain whether the load area is the only factor that makes AVN processes in lower extremity progress pathologically without restitutio ad integrum or it is a normal variant of ossification defects, as has been described for other areas of the foot1,11, with brief symptoms and spontaneous healing. Given the clinical course in our case and that described by Souverijns et al.4, it seems clear that AVN of the epiphysis of the first MTT bone is a transient self-resolving condition that requires no treatment. In children, the tendency of AVN to self-resolve in other areas of the foot (except when involving MTT bone heads, which receive direct load) and its benign course, suggest that it may go underdiagnosed when presents without symptoms or may go unnoticed because the patient is minimally symptomatic. Due to the high frequency of foot contusions and injuries during childhood, AVN are often unaccounted for, as medical attention is usually unnecessary. Should the process be asymptomatic it would go undiagnosed; thus, the real prevalence among the pediatric population remains unclear.
Given that the duration of symptoms is brief (moderate pain that lasted a few weeks in our patient), AVN can be categorized as a physiological disorder, or a normal variant when associated to other processes (Köhler’s in the navicular bone and Sever’s in calcaneus and cuneiform bones). Similarly, Gurevich et al.11 described a patient with bilateral non-synchronous AVN of the first metatarsal head that healed almost spontaneously. Although Souverijns et al.4 consider proximal AVN of the first MTT bone a form of idiopathic osteonecrosis, we consider that such lesions may be classified as normal physiologic variants, as has been described in other areas of the foot1.
Rest and/or reduction of physical exercise and symptomatic treatment with ibuprofen are recommended. Conservative treatment was effective in the case described by Souverijns et al.4 and in our patient; in both there was restitutio ad integrum in density but a slight increase in size and shape. Arch support can be used if symptoms persist.
To the best of our knowledge, we describe the second case of AVN of the proximal epiphysis of the first MTT bone. AVN is a rare cause of foot pain and limping in children that has not been described in the orthopedic literature. Recognizing it as a differentiated entity is key to avoid unnecessary complementary or diagnostic tests (laboratory tests, CT-scans, MRI, or technetium-99 bone scans). Harmful or potentially aggressive treatments should be avoided, including conservative measures such as shoe inserts, plantar orthotics, or casts, given the benign and self-resolving nature of the process. We propose that this condition should be considered a normal variant, as other self-resolving AVN in other locations of the tarsal bones.















