Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
International Microbiology
versão impressa ISSN 1139-6709
INT. MICROBIOL. vol.7 no.1 Mar. 2004
| RESEARCH NOTE | |||
|
| |||
| Simultaneous PCR detection
Summary. Recent data show that more than 50% of catheter-associated bloodstream infections are caused by staphylococci. Staphylococcal infections produced by intercellular-adhesion cluster (ica) carriers can be even more problematic due to the presence of methicillin and mupirocin resistance genes. In the present study, a multiplex PCR protocol that allows the simultaneous identification of staphylococci and detection of both the ica and methicillin and/or mupirocin resistance genes was developed. Furthermore, the method allows differential detection of the ica locus from Staphylococcus aureus and Staphylococcus epidermidis. [Int Microbiol 2004; 7(1): 63 - 66] Key words: Staphylococcus aureus · Staphylococcus epidermidis · intercellular adhesion gene cluster · antibiotic resistance · multiplex PCR | ||
| |||
| Detección simultánea del cluster ica y de los genes de resistencia a meticilina y mupiricina en Staphylococcus aislados de catéteres Resumen. Estudios recientes han demostrado que más del 50% de las septicemias asociadas al uso de catéteres están causadas por estafilococos. Las infecciones estafilococales producidas por cepas portadoras del operón de adhesión intercelular (ica) pueden agravarse por la presencia de genes de resistencia a la meticilina y/o a la mupirocina. Hemos desarrollado un protocolo de PCR múltiple que permite, simultáneamente, identificar estafilococos y detectar la presencia de ica y de los genes de resistencia a la meticilina y/o a la mupirocina. Además, dicho método permite la detección diferencial del locus ica de Staphylococcus aureus y/o S. epidermidis. [Int Microbiol 2004; 7(1):63- 66] Palabras clave: Staphylococcus aureus · Staphylococcus epidermidis · cluster génico de adhesión intercelular · resistencia a antibióticos · PCR múltiplex | Detecção simultânea do cluster ica e dos genes de resistência a meticilina e mupiricina em Staphylococcus isolados de catéteres Resumo. Estudos recentes têm demonstrado que mais de 50% das septicemias associadas ao uso de catéteres são causadas por estafilococos. As infecções estafilocócicas produzidas por cepas portadoras de operón de adesão intercelular (ica) podem agravar-se pela presença de genes de resistência a meticilina e/ou a mupirocina. Foi desenvolvido um protocolo de PCR múltiplo que permite, simultaneamente, identificar estafilococos e detectar a presença de ica e dos genes de resistência a meticilina e/ou a mupirocina. Este método permite a detecção diferencial do locus ica de Staphylococcus aureus e/ou de S. epidermidis. [Int Microbiol 2004; 7(1):63- 66] Palavras chave: Staphylococcus aureus · Staphylococcus epidermidis · cluster gênico de adesão intercelular · resistência a antibióticos · PCR multiplex |
Introduction
A major achievement within the medical field in the twentieth century was the invention and development of protesic surgical implants. However, such implants frequently become infected by bacteria [7,18,23]. This is a serious complication, especially when the infection is caused by multiresistant bacteria, which are difficult to eradicate from the protesic material. Additionally, the efficiency of some bacteria in their ability to colonize indwelling medical devices, such as catheters [6,7], poses particular problems. These bacteria develop a highly consolidated structure: the biofilm [6,7,25]. In the biofilm, microbial populations reside within a matrix that facilitates cell-to-cell and/or cell-surface adherence, resulting in an inherent structural resistance towards antimicrobial agents, such as antibiotics, disinfectants, and germicides [7,8,19,24]. In the case of staphylococci, formation of the biofilm requires polysaccharidic intercellular adhesin (PIA), which is synthesized by enzymes encoded by the intercellular adhesion cluster (ica) [5,11,14].
Recent data show that 50% of pathogens isolated from hospital-acquired bloodstream infections, normally associated with the use of central-venous catheters, are staphylococci [3,4,9]. Furthermore, many Staphylococcus aureus and Staphylococcus epidermidis strains carry the ica cluster. Staphylococcal infections produced by ica carriers can, in turn, be even more problematic due to the presence of methicillin and mupirocin resistance genes [10,15,20].
Nosocomial infections due to methicillin-resistant staphylococci have increased subsequent to the widespread use of β-lactamic antibiotics. The transmission of resistant strains among hospital departments, and the ability of bacteria to transmit resistance genes are well-known [18,22]. With respect to mupirocin, several recent studies indicate the utility of topical mupirocin application in order to avoid the colonization of indwelling medical devices. While mupirocin is not an antibiotic for treatment of infections once they occur, it is used prophylactically to prevent S. aureus strains from reaching the inner part of the device. However, this application has led to the selection of highly mupirocin-resistant staphylococci [2,4,16]. For example, in our hospital, the incidence of mupirocin resistance has increased sharply from 7.7% in 1998 to 19% in 2000 [22].
Since most S. aureus are ica carriers, the colonization of devices by isolates harboring both resistance genes and adhesion genes has become a serious problem. Rapid detection of the ica locus in hospital staphylococcal isolates, together with simultaneous detection of antibiotic-resistance genes, may allow the development of methods to prevent or reduce the ability of bacterial to invade indwelling medical devices. It should be noted that the presence of the ica locus does not guarantee its expression; thus, it does not directly reflect biofilm formation. However, anticipating and detecting the possibility of biofilm colonization of catheters before it actually occurs would be of great help in preventing infection. For this reason, we developed a method to simultaneously detect ica and methicillin- and mupirocin-resistance markers. The method described here is a rapid and easy means to verify that catheters are not being colonized by mupirocin-resistant, methicillin-resistant staphylococci harboring the ica cluster. The presence within the hospital of these staphylococci would not only make the preventive use of mupirocin useless, it could also lead to an increased risk of infections.
Materials and methods
Bacterial isolates, identification, susceptibility testing, and DNA extraction method. S. epidermidis strains 1855-25, 9295-79, and 9951-79 were isolated from catheters obtained from the Oncology Service of our hospital (Nuestra Señora de Candelaria University Hospital, Santa Cruz de Tenerife, Spain). S. aureus strain 229 was isolated from the sputum of a patient with sepsis. All strains were biochemically identified, and antibiotic-resistance patterns were determined according to the standard laboratory criteria of the Microbiology Service of our hospital. S. aureus 229 and S. epidermidis 1855-25 and 9295-79 were methicillin and mupirocin resistant, whereas S. epidermidis 9295-79 was mupirocin and methicillin sensitive.
The DNA extraction method has been described previously [20,21]. After overnight culture on brain-heart infusion agar plates, one or two colonies (one from a S. aureus isolate and one from a S. epidermidis isolate) were suspended in 20 ml of sterile distilled water, and the suspension was then heated at 100ºC for 20 min. From this suspension, a 5-ml aliquot was directly used as template for PCR amplification.
Multiplex PCR amplification. The oligonucleotide primers have all been previously described [1,10,13,17,20]. icaAB-F: 5''-TTATCAATGCCGCAGTTGTC-3' and icaAB-R: 5'-GTTTAACGCGAGTGCGCTAT-3' from partial icaAB genes of S. epidermidis, icaA-S: 5'-AAACTTGGTGCGGTTACAGG-3' and icaA-E: 5'-TCT GGGCTTGACCATGTTG-3' from partial icaAB genes of S. aureus, FemB1: 5'-TTACAGAGTTAACTGTTACC-3' and FemB2: 5'-ATACAAATCCAGCACGCTCT-3' from femB, MupA: 5'-TATATTATGCGATGGAAGGTTGG-3' and MupB: 5'-AATAAAATCAGCTGGAAAGTGTTG-3' from ileS-2 and MecA1: 5'-GTAGAAATGACTGAACGTCCGATAA-3' and MecA2: 5'-CCAATTCCACATTGTTTCGGTCTAA-3' from mecA. Multiplex PCR assays were all carried out directly using the bacterial suspension obtained after the rapid DNA extraction method described above. A 5-ml aliquot of this suspension was added to 45 ml of PCR mixture consisting of 1× reaction buffer [16 mM (NH4)2SO4, 67 mM Tris-HCl (pH 8.8)], 0.2 mM of each of the four dNTPs (Promega, Madison, WI, USA), 3.5 mM MgCl2, 3.6 µM of each femB primer, 0.2 µM of each ileS-2 primer, 0.1 µM of each mecA primer, and 0.8 µM of each icaAB primer and 1.25 U of Taq DNA polymerase (Bioline, UK). For each sample, one reaction was done with the femB pair of primers to identify S. aureus strains, with the mecA and ileS-2 pairs of primers to detect both resistance markers, and with the two icaAB pairs of primers to detect the ica cluster from S. aureus, S. epidermidis, or simultaneously from both. In order to reduce the formation of nonspecific extension products, a "hot-start" PCR protocol was used. All multiple PCR assays were carried out with a negative control containing all of the reagents without DNA template. DNA was amplified in a GeneAmp PCR system 9700 thermocycler (PE, Applied Biosystems, CA, USA) with the following thermal cycling profile: an initial denaturation step at 94ºC for 5 min was followed by 10 cycles of amplification (denaturation at 94ºC for 30 s, annealing at 66ºC for 45 s, and extension at 72ºC for 60 s); 5 cycles of amplification (denaturation at 94ºC for 45 s, annealing at 64ºC for 45 s, and extension at 72ºC for 60 s); and 25 cycles of amplification (denaturation at 94ºC for 45 s, annealing at 50ºC for 45 s, and extension at 72ºC for 60 s), ending with a final extension step at 72ºC for 10 min. After PCR amplification, 5 µl were removed and subjected to 2% agarose gel electrophoresis to estimate the size of the amplification products by comparison with a 100-bp molecular size standard ladder (Roche Diagnostics, Mannheim, Germany). The gel was stained with ethidium bromide and the amplicons were visualized using a UV light.
The reaction conditions for the multiplex PCR assay were optimized to ensure that all of the target gene sequences were satisfactorily amplified. The primers used in this study differ in annealing temperatures, which increased the possibility of occurrence of unwanted bands originating from non-specific amplification. Therefore, both a "hot-start" and three rounds of amplification with different annealing temperatures were carried out. In addition, there is evidence indicating that multiplex PCR with targets that differ widely in size often favors amplification of the shorter target over the longer one, resulting in different amounts of amplified products [21]. For this reason, in order to optimize the conditions for the multiplex PCR analysis, different primer concentrations, template DNA preparations, and MgCl2 concentrations were assayed. As described above, the final quantities generated optimal results were 3.5 mM MgCl2, 180 pmol of each femB primer, 10 pmol of each ileS-2 primer, 5 pmol of each mecA primer, 40 pmol of each icaAB primer and 5 ml of the DNA solution obtained with our DNA extraction method.
Results and Discussion
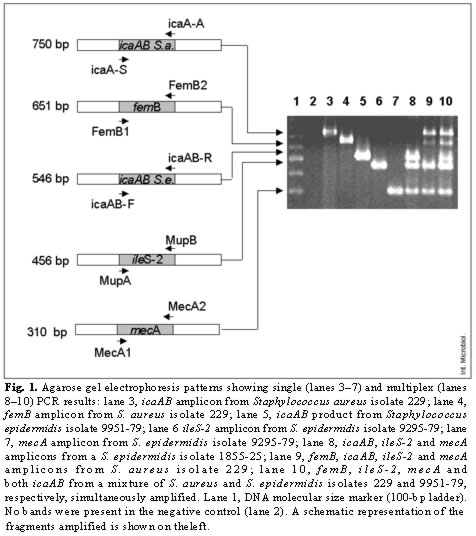
Prior to optimizing the multiple PCR, the PCR protocol was evaluated in order to ensure that it was adequate for the individual amplification of all five DNA fragments. Each individual amplification yielded a fragment of the expected size, i.e. 750-, 651-, 546-, 456-, and 310-bp, respectively. Figure 1 shows an agarose gel that illustrates results typically obtained with the optimized PCR assay. Amplification of icaAB, femB, ileS-2 and mecA targets produced distinct, easily recognizable bands corresponding to their respective molecular size (lanes 3- 7). The icaAB fragments were clearly differentiated when amplified from S. aureus or from S. epidermidis (lanes 8- 10); femB was always amplified in the case of S. aureus strains (lane 9) and never in the case of S. epidermidis (lane 8). Results obtained for the mecA and ileS-2 fragments were in accordance with the resistance pattern of the isolates: methicillin- and mupirocin-resistant isolates S. epidermidis 1855-25 and S. aureus 229 presented the mecA fragment and showed the ileS-2 marker (lanes 8- 10). PCR from mixed S. aureus 229 and S. epidermidis 9951-79 colonies permitted the simultaneous detection of the five different targets (lane 10)
This protocol, including the rapid extraction of DNA from single colonies and electrophoretic analysis of the amplified products on an agarose gel, was completed in less than 6 h. Moreover, it can be used for S. aureus and S. epidermidis and for a mixture of both staphylococci.
Nowadays, since few antibiotics, including mupirocin, constitute the last resort against MRSA, and due to the increasing incidence of catheter-associated staphylococcal bloodstream infections, a fast, sensitive laboratory method to immediately detect multiple-resistant staphylococci harboring the ica cluster is urgently needed. Although most S. aureus carry the ica cluster, confirmation of its presence in a particular isolate is a necessary step in preventing colonization by potentially biofilm-forming strains. The method described herein is highly sensitive and specific, fast and feasible, and thus provides a new tool for controlling catheter-borne infections.
Acknowledgements. This work was supported by grants 2001/020 from the Consejería de Educación, Cultura y Deportes, Canarian Autonomous Government, FIS PI 01/3150 from the Health Spanish Ministry, and Bio 2002/00953 from the Spanish Ministry for Science and Technology. S.M.A. was supported by FIS contract 99/3060 (Fondo de Investigación Sanitaria, Spain).
References
1. Anthony RM, Connor AM, Power EGM, French GL (1999) Use of the polymerase chain reaction for rapid detection of high-level mupirocin resistance in staphylococci. Eur J Clin Microbiol Infect Dis 18:30-34 [ Links ]
2. Berns JS (2003) Infection with antimicrobial-resistance microorganisms in dialysis patients. Seminars in Dialysis 16:30-37 [ Links ]
3. Bouza E, Burillo A, Muñoz P (2002) Catheter-related infections: diagnosis and intravascular treatment. Clin Microbiol Infect 8:265-274 [ Links ]
4. Centers for Disease Control and Prevention (2002) Safer, healthier people. Guidelines for the prevention of intravascular catheter-related Infections. Mor Mortal Wkly Rep. Recommendations and reports. 51(RR-10) [ Links ]
5. Cramton SE, Gerke C, Schnell F, Nichols WW, Götz F (1999) The intercellular adhesion (ica) locus is present in Staphylococcus aureus and is required for biofilm formation. Infect Immun 67:5427-5433 [ Links ]
6. Donlan RM (2001) Biofilm formation: A clinically relevant microbiological process. Clin Infect Dis 33:1387-1392 [ Links ]
7. Donlan RM, Costerton JW (2002) Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev 15:167-193 [ Links ]
8. Dunne WM Jr (2002) Bacterial adhesion: seen any good biofilms lately? Clin Microbiol Rev 15:155-166 [ Links ]
9. Eggimann P, Pittet D (2002) Overview of catheter-related infections with special emphasis on prevention based on educational programs. Clin Microbiol Infect 8:295-309 [ Links ]
10. Frebourg NB, Lefebvre S, Baert S, Lemeland JF (2000) PCR-based assay for discrimination between invasive and contaminating Staphylococcus epidermidis strains. J Clin Microbiol 38:877-880 [ Links ]
11. Galdbart JO, Allignet J, Tung HS, Rydèn C, El Solh N (2000) Screening for Staphylococcus epidermidis markers discriminating between skin-flora strains and those responsible for infections of joint prostheses. J Infect Dis 182:351-355 [ Links ]
12. O'Gara J, Humphreys H (2001) Staphylococcus epidermidis biofilms: importance and implications. J Med Microbiol 50:582-587 [ Links ]
13. Geha DJ, Uhl JR, Gustaferro CA, Persing DH (1994) Multiplex PCR for identification of methicillin-resistant staphylococci in the clinical laboratory. J Clin Microbiol 32:1768-1772 [ Links ]
14. Götz F (2002) Staphylococcus and biofilms. Mol Microbiol 43:1367-1378 [ Links ]
15. Jones SM, Morgan M, Humphrey TJ, Lappin-Scott H (2001) Effect of vancomycin and rifampicin on methicillin-resistant Staphylococcus aureus biofilms. Lancet 357:40-41 [ Links ]
16. Johson DW, MacGinley R, Kay TD, Hawley CM, Campbell SB, Isbel NM, Hollet P (2002) A randomised controlled trial of topical exit site mupirocin application in patients with tunnelled, cuffed haemodialysis catheters. Nephrol Dial Transplant 17:1802-1807 [ Links ]
17. Kobayashi N, Wu H, Kojima K, Taniguchi K, Urasawa S, Uehara N, Omizu Y, Kishi Y, Yagihashi A, Kurokawa I (1994) Detection of mecA, femA and femB genes in clinical strains of staphylococci using polymerase chain reaction. Epidemiol Infect 113:259-266 [ Links ]
18. Livermore D M (2002) Antibiotic resistance in staphylococci. Int J Antimicrob Agents S3-S10 [ Links ]
19. Mack D (1999) Molecular mechanisms of Staphylococcus epidermidis biofilm formation. J Hosp Infect 43:S113-S115 [ Links ]
20. Martín-López JV, Pérez-Roth E, Claverie-Martín F, Díez-Gil O, Batista N, Morales M, Méndez-Álvarez S (2002) Detection of Staphylococcus aureus clinical isolates harbouring the ica gene cluster needed for biofilm establishment. J Clin Microbiol 40:1569-1570 [ Links ]
21. Pérez-Roth E, Claverie-Martín F, Villar J, Méndez-Álvarez S (2001) Multiplex PCR for simultaneous identification of Staphylococcus aureus and detection of methicillin and mupirocin resistance. J Clin Microbiol 39:4037-4041 [ Links ]
22. Pérez-Roth E, Claverie-Martín F, Batista N, Moreno A, Méndez-Álvarez S (2002) Mupirocin resistance in methicillin-resistant Staphylococcus aureus clinical isolates in a Spanish hospital. Co-application of multiplex PCR assay and conventional microbiology methods. Diagn Microbiol Infect Dis 43:123-128 [ Links ]
23. Raad I, Alrahwan A, Rolston K (1998) Staphylococcus epidermidis: Emerging resistance and need for alternative agents. Clin Infect Dis 26:1182- 1187 [ Links ]
24. Rachid S, Ohlsen K, Witte W, Hacker J, Ziebuhr W (2000) Effect of Subinhibitory antibiotic concentrations on polysaccharide intercellular adhesin expression in biofilm-forming Staphylococcus aureus. Antimicrob Agents Chemother 44:3357-3363 [ Links ]
25. Stewart PS, Costerton JW (2001) Antibiotic resistance of bacteria in biofilms. Lancet 358:135-138 [ Links ]