Introduction
In 2020, the COVID-191 pandemic caused more than 79 million cases of infection and took more than 1.7 million lives worldwide, with the Americas being the most severely affected region2. The number of cases in Peru was over one million, and the disease killed more than 37,000 people, one of the highest death rates per million inhabitants on the entire continent2,3.
The World Health Organisation has issued a set of recommendations to reduce the risk of transmission, which include measures for personal hygiene and social distancing4. However, the situation in prisons, characterised by overcrowding, limited access to basic services, poor ventilation5 and inadequate healthcare6, along with other factors such as the high prevalence of chronic diseases7 and alcohol and drug abuse8, make the prison populations of countries on the American continent highly vulnerable to infectious diseases5,9.
The living conditions in Peruvian prisons in terms of housing, nutrition, etc. do not meet international standards or constitutional guarantees that protect inmates' rights10. Reduced, overcrowded spaces where prisoners are forced to live and sleep, limited access to water and drainage, precarious living conditions, the social problems caused by cohabitation, a greater load of chronic diseases and lack of healthcare result in a very high risk of infection for the Peruvian prison population from COVID-19, and a more severe evolution of the disease when compared to the general public. The outbreak of COVID-19 in the prison population also represents a public health problem, since the inmates evacuated to external health centres and prison staff represent a vector of transmission to the community at large11,12.
The international standard for establishing COVID-19 infection is testing that detects the nucleic acid of the virus13. However, the diagnostic strategy in Peru is based mainly on rapid antigen tests14, although such tests only enable the immune response to infection to be assayed15.
Despite the importance of this phenomenon for the health system, there are still no studies in Peru on the evolution of COVID-19 in prisons. We need to know more about the characteristics of the persons who are affected to create the appropriate responses to enable the prison system to deal with new waves of the pandemic. The aim of this study is to describe the clinical and epidemiological characteristics of infections and fatalities amongst inmates as a result of COVID-19 in Peru, according to the Peruvian National Prisons Institute from April to October 2020.
Material and method
Descriptive, retrospective and transversal study
Population and sample
The benchmark population consisted of 87,754 inmates in October 2020 distributed in 68 prisons around the country, with a total occupation indicator of 215%. The region of Lima held the majority of the prison population (47.8%)16. 88.9% of the total population was screened at the end of the mass screening with the antibody serological test (Core tests® COVID-19 IgM/IgG Ab Test) in October 2020. The study sample was made up of all the inmates who reacted to the Core tests® COVID-19 IgM/IgG Ab Test (n = 37.103). The sample was a convenience, non-probabilistic census type. Non-reactive inmates, subjects who did not receive the rapid test or whose official registry results were missing were excluded. Lethality was calculated as number of fatalities caused by COVID-19 from amongst the total number of confirmed cases of COVID-19 according to the rapid test. All the fatalities were confirmed by rapid testing.
The PR Core tests® COVID-19 IgM/IgG Ab Test qualitatively detects the IgM and IgG antibodies of COVID-19 in serum/plasma or whole blood of human origin. The sensitivity of IgM and IgG is 97.6%; the specificity of IgM and IgG, is 100%; and there is a total coincidence of 98.8%17.
The study period chosen was the months between April and October 2020. The reason for this was: the first confirmed case of COVID-19 in Peruvian prisons was reported in April 2020; mortalities from COVID-19 in Peruvian prisons were recorded between April and October 2020; mass screening of the prison population with rapid tests was completed in October 2020.
Data gathering technique
The documentary analysis technique was used to gather data18. The data sources were the prison records, clinical histories, epidemiological records, the data base of the Integrated System for COVID-19 (SISCOVID), reference sheets of the Ministry of Health, evacuation reports and death certificates. The analysis unit was inmates infected by COVID-19.
The data was gathered by both researchers between August and December 2020. A data gathering sheet prepared by the authors was used. The sheet consisted of 16 items; seven of which were about epidemiological characteristics, while nine were about clinical aspects. The instrument used was duly subjected to peer review, and the Aiken validity coefficient value was over 0.90 in all the items. The information obtained was exhaustively reviewed by the researchers to ensure consistency and quality. The inmates were codified and their identities kept secret at all times.
Statistical analysis
Once the information quality control and data base were completed, the results were analysed by means of a descriptive statistical procedure involving SPSS v26 software (SPSS Inc., USA) for Windows. The data was presented as absolute numbers, medians, standard deviation and range for the absolute variables and absolute and relative frequencies for the qualitative variables.
Ethical aspects
The research was reviewed and approved by the Institutional Committee on Ethics in Research (Norbert Wiener Private University, Lima, Peru) under proceeding no. 061-2020 of 18 June 2020. The standards of the Helsinki Declaration were complied with19. No informed consent was required to use the secondary data source. The information was kept confidential and securely stored throughout the entire process. The appropriate institutional permits were obtained.
Results
37,103 inmates were analysed out of a total prison population of 87,754, all of whom were reactive to the rapid test.
The 37,103 inmates (42.3% of the total) had an average age of 39.9 ± 12.6 years (range 18-91); 95.5% were male and 67.6% were convicted prisoners. As regards the total reactivity to the Core tests® COVID-19 IgM/IgG Ab Test, 60.1% (n=22.290) were IgG reactive; 36.1% (n=13.390), IgM/IgG reactive and 3.8% (n=1.423), IgM reactive. The time distribution according to type of reactivity can be seen in Figure 1.

Figure 1. Time distribution of inmates reactive to the Core tests® COVID-19 IgM/IgG Ab Test (n = 37.103) according to type of reactivity, according to data from the Peruvian National Prisons Institute, April-October 2020. Source: compiled by authors.
20.1% of the reactive inmates (n=7,458) had symptoms compatible with COVID-19 when the rapid test was carried out. Figure 2 shows the time distribution of the number of inmates screened with rapid testing, the percentage of reactivity and of inmates with symptoms of COVID-19.

Figure 2. Time distribution temporal of inmates screened with RT that indicates the percentage of reactive inmates and of inmates with symptoms of COVID-19 disease when the test was carried out, according to data from the Peruvian National Prisons Institute, April-October 2020.
Other clinical-epidemiological characteristics of the inmates infected with COVID-19 can be seen in Table 1.
Table 1. Clinical-epidemiological characteristics of inmates infected with COVID-19 according to RT* test results (INPE, April-October 2020)
| n | % | |
|---|---|---|
| Origins (n = 37.103) | ||
| Lima Metropolitana and Callao | 14.259 | 38.4 |
| Coast. except Lima and Callao | 9.585 | 25.8 |
| Mountain region | 9.723 | 26.2 |
| Jungle region | 3.154 | 8.5 |
| Other country | 382 | 1.1 |
| Educational level (n = 37.103) | ||
| Illiterate | 725 | 2.0 |
| Primary | 7840 | 21.1 |
| Secundary | 25.269 | 68.1 |
| Vocational training | 1.810 | 4.9 |
| Higher education | 1.459 | 3.9 |
| Occupation outside prison (n = 37.103) | ||
| Unemployed or casual work | 264 | 0.7 |
| Construction labourer | 9.723 | 26.2 |
| Employee | 10.948 | 29.5 |
| Farmer | 5.261 | 14.2 |
| Driver | 5.491 | 14.8 |
| Sales | 2.924 | 7.9 |
| Technician | 964 | 2.6 |
| Professional | 817 | 2.2 |
| Student | 711 | 1.9 |
| Marital status (n = 37.103) | ||
| Cohabiting | 16.715 | 45.1 |
| Single/a | 15.857 | 42.7 |
| Married/a | 3.546 | 9.5 |
| Widow(er) | 281 | 0.8 |
| Divorced | 187 | 0.5 |
| Separated | 517 | 1.4 |
| Clinical severity of COVID-19 (n = 37.103) | ||
| Asymptomatic | 29.645 | 79.9 |
| Slight | 5.916 | 15.9 |
| Moderate | 1.515 | 4.1 |
| Serious | 27 | 0.1 |
| Symptoms of COVID-19 (n = 7.458) | ||
| Headache | 4.149 | 55.6 |
| General malaise | 3.705 | 49.7 |
| Fever | 3.656 | 49.0 |
| Cough | 3.579 | 48.0 |
| Sore throat | 3.276 | 43.9 |
| Difficulty breathing | 1.743 | 23.4 |
| Blocked nose | 1.588 | 21.3 |
| Diarrhoea | 1.553 | 20.8 |
| Nausea. vomiting | 815 | 10.9 |
| Muscle pain | 456 | 6.1 |
| Other | 675 | 9.1 |
| Risk factors for COVID-19 (n = 37.103) | ||
| Over 60 years of age | 3.111 | 8.4 |
| High blood pressure | 1.050 | 2.8 |
| Diabetes mellitus | 905 | 2.4 |
| Chronic lung disease | 486 | 1.3 |
| Obesity | 272 | 0.7 |
| Cardiovascular disease | 41 | 0.1 |
| Others | 38 | 0.1 |
Note. COVID-19: coronavirus disease 2019; INPE: Peruvian National Prisons Institute; RT*: Core tests® COVID-19 IgM/IgG Ab Test. Source: compiled by authors.
The figures for mortality caused by COVID-19 showed 445 deaths in total (Figure 3). The prison with the most deaths (n=43) was Miguel Castro Castro (Lima). Total lethality stood at 1.2% of the infected inmates. which in age terms was 0.65% in older adults (n = 241), 0.52% in the age group between 30 and 59 years (n = 193); and 0.03% amongst the youngest inmates (n = 11). 96.6% of the deaths were amongst males. The largest number of deaths occurred amongst inmates from the Peruvian mountain region (36.4%), followed by the Lima Metropolitana and Callao districts (29.0%) and the coast (23.2%). 1.8% (n = 8) of the deceased were foreigners. Table 2 shows other characteristics relating to mortality.
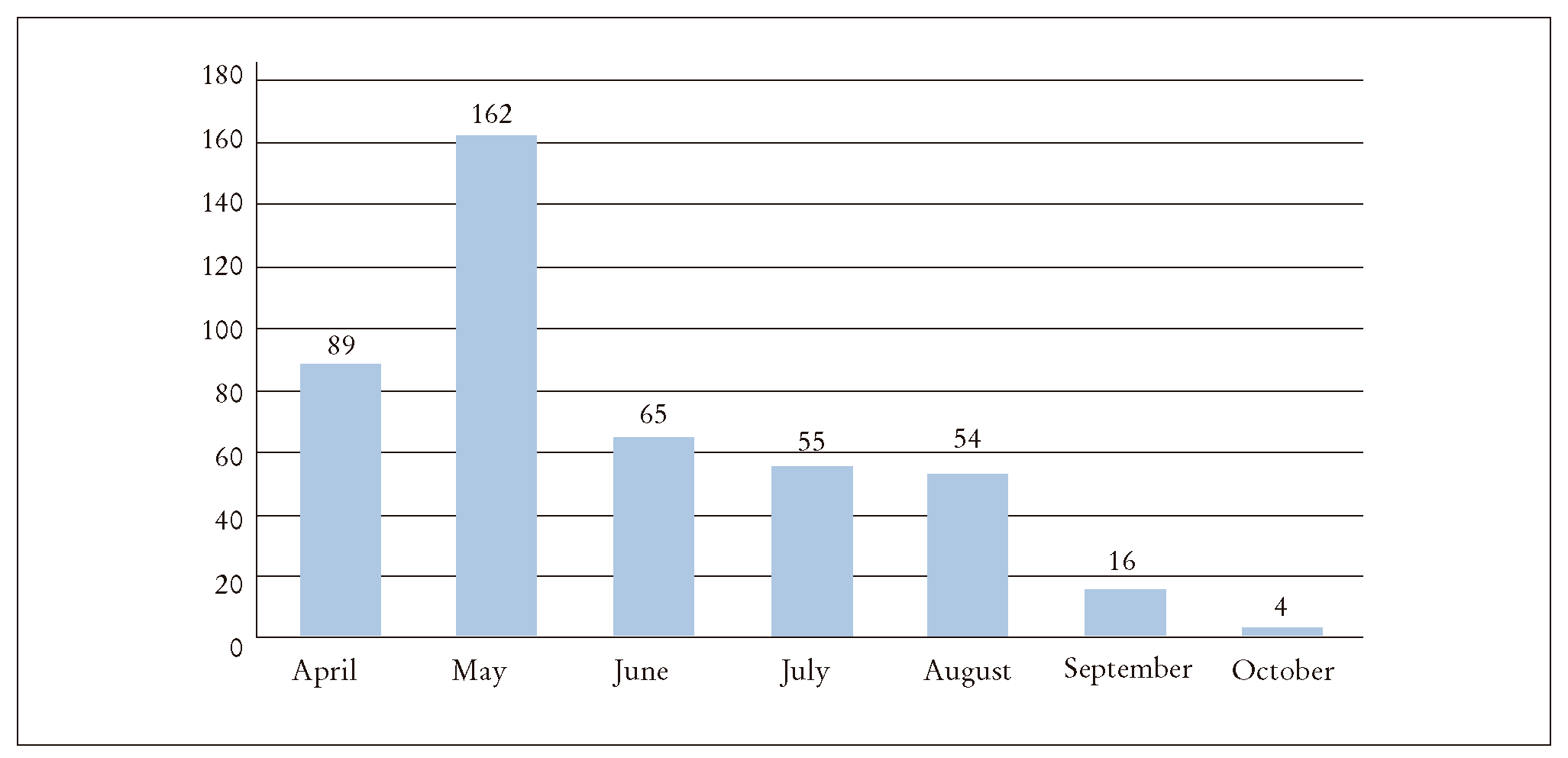
Figure 3. Time distribution of inmates who died from COVID-19 (n = 445), according to data from the Peruvian National Prisons Institute, April-October 2020. Source: compiled by authors.
Table 2. Characteristics of inmates who died from COVID-19 (INPE, April-October 2020)
| n | % | |
|---|---|---|
| Place of death (n = 445) | ||
| In prison | 46 | 10.3 |
| At public referring hospital with medical care | 387 | 87.1 |
| At public referring hospital without medical care | 5 | 1.1 |
| During transfer to referring hospital | 6 | 1.3 |
| At hospital entrance (hospital did not receive patient) | 1 | 0.2 |
| Direct cause of death (n = 445) | ||
| Respiratory failure | 426 | 95.7 |
| Multi-organ failure | 16 | 3.6 |
| Septic shock | 2 | 0.5 |
| Myocardial infarction | 1 | 0.2 |
| Risk factors (n = 445) | ||
| Over 60 years | 241 | 54.2 |
| High blood pressure | 80 | 17.9 |
| Diabetes mellitus | 67 | 15.1 |
| Chronic lung disease | 38 | 8.5 |
| Obesity | 14 | 3.2 |
| Chronic kidney disease | 10 | 2.3 |
| HIV/AIDS | 8 | 1.8 |
| Cancer | 6 | 1.4 |
Note. COVID-19: coronavirus disease 2019; INPE: Peruvian National Prisons Institute; HIV: human immunodeficiency virus. Source: compiled by authors.
Discussion
This study is the first one in Peru to describe the clinical-epidemiological characteristics of inmates who have been infected and died from COVID-19. It sets out to offer the necessary input to generate preventive-promotional and corrective measures to manage epidemics and pandemics in the Peruvian prison system.
In principle, the results obtained from the research show significant differences between the sample studied and the official data of the Peruvian Ministry of Health on the general public with regard to infection and death from COVID-1920. The total reactivity to type 2 coronavirus causing severe acute respiratory syndrome in the prison population that was screened (47.6%) exceeded the accumulated positivity amongst the general public in late October 2020 (19.9%).
However, the total lethality rate in the sample (1.2%) was significantly lower than amongst the general public infected in the same period (3.8%). The lethality in this study amongst age groups of young people from 18 to 29 years (0.12%), adults from 30 to 59, (0.77%) and adults over 60 years (7.75%) was lower than in the general public (0.20, 1.91 and 15.19%, respectively). The proportion of infected older adults reported by the Ministry of Health (17%) was higher than the one found in this study (8.4%). The distribution of reactive persons according to sex amongst the general public was almost identical, while the absolute majority in the prison population were men (95.5%), which can be explained by the initial gender distribution amongst the inmates.
While symptomatic cases in Peru increased notably from March 2020 and reached their maximum levels in August20, most cases of the disease in the prison population appeared between April and June, as shown in the findings, which also matches the results relating to deaths reported in this study.
It should be mentioned that polymerase chain reaction testing on asymptomatic patients and rapid antigen tests on symptomatic ones would be more accurate in this type of screening. This approach would also be effective as an early detection strategy when inmates enter prison.
However, the Peruvian National Prisons Institute lacked rapid tests in the first months of the pandemic and mass screening took place in late July. The results obtained, such as the predominance of IgG in total reactivity (60.1%), confirm the notion that most inmates were infected months before. There is room to suspect that the pandemic in the prison system developed in line with the epidemiological patter found amongst the Peruvian general public (Figure 4), which was not duly noted due to the lack of specific diagnostic resources from the moment the pandemic commenced.
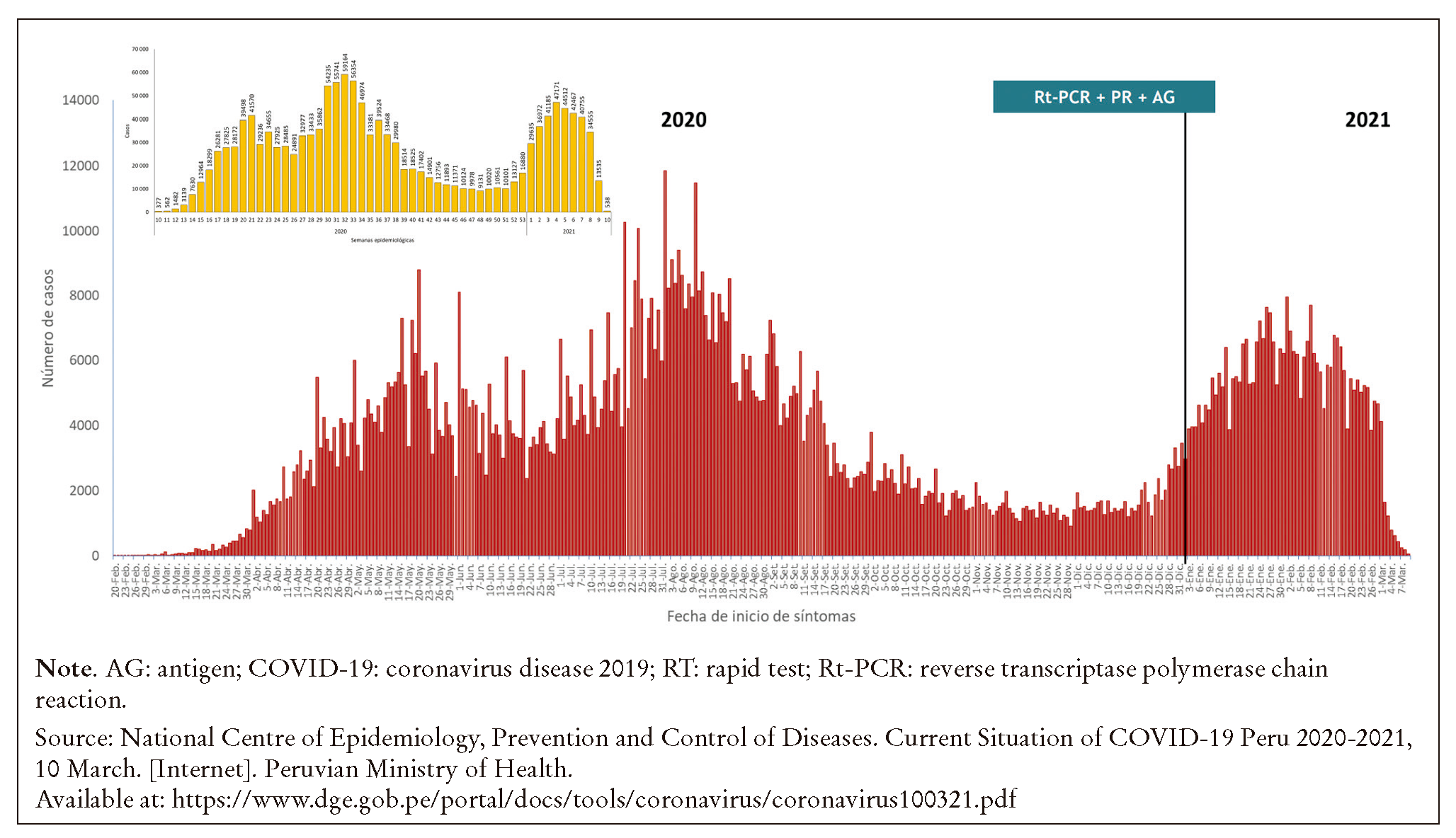
Figure 4. Confirmed cases of coronavirus disease 2019, according to date when symptoms commenced, in Peru 2020-2021.
It should be noted that current prison conditions in Peru do not allow the international recommendations on isolation of cases with COVID-19 to be complied with.
No deaths from COVID-19 were recorded in Peruvian prisons over the period dating from the end of the period of the study (October 2020) to the completion of this article, while the number of symptomatic patients has been around 10%. These results may be interpreted as a type of herd immunity effect caused by prison conditions (overcrowding, inadequate infrastructure).
International data shows relatively adequate control of the pandemic in the prisons of most industrialised countries, while the data for more disadvantaged contexts is very scarce21.
The figures for inmates and federal prisons in Canada for October 2020 showed 5.1% of COVID-19 positive cases in the screened population and a lethality of 0.5% amongst infected patients22. There were 153,236 cases registered in the USA over the same period, with a lethality rate of 0.7%23. These figures are lower than those for reactivity and fatality in this study (47.6 and 1.2%, respectively). Prison records for Spain also show significantly lower figures21. Research on 485 convicted inmates in Italy showed only 0.61% of IgM/IgG24 positive cases, which is way below the findings in this article (36.1%). In the UK, the infection rate amongst inmates over 60 years of age in September 2020 was 1.6%, while the same group in this study showed levels of 8.4%25.
On the other hand, the rate of cases of COVID-19 amongst convicts in the USA was 5.5 times higher than amongst the general public, and the adjusted mortality rate in the prison population was three times higher26. However, our study showed a reactivity in the prison population that was 2.4 times higher, but with a level of lethality that was three times lower than amongst the general public.
Finally, amongst other limitations of the study is the fact that the identification of cases of COVID-19 in the prison system was late, incomplete and with rapid antibody serology tests, which may have led to under-reporting. No other clinical, radiological or laboratory data of inmates with or without clear symptoms of COVID-19 could be included due to the almost total lack of data.
Conclusions
The main clinical-epidemiological characteristics of inmates who were infected and died from COVID-19 in Peruvian prisons from April to October 2020 were described. The findings show that the approaches used to managing epidemics in the prison context need to be different from those used amongst the general public. The structure and functioning of the prison system when faced with epidemics should be reconsidered. More studies are also required to enable results to be compared with those of other countries, especially those with a similar economic, social and cultural context, to define more effective corrective and preventive-promotional strategies that also focus on human rights.
The current COVID-19 pandemic has shown how changes in the biosphere and techno-sphere are endangering human life and health. The short and long term perspectives are uncertain, but there is a clear need to reorganise the prison health system, to prioritise and modernise it. The long-delayed reform of the prison system and the measures that set out to halt the spread of COVID-19 in prisons form a part of this necessary process.














