My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Educación Médica
Print version ISSN 1575-1813
Educ. méd. vol.15 n.2 Jun. 2012
Studying Medicine in Germany
Estudiar medicina en Alemania
Pedro Mestres-Ventura, Kurt W. Becker
Institute of Anatomy and Cell Biology. Faculty of Medicine. Saarland University. Homburg Saar, Alemania.
ABSTRACT
This article gives a general overview on the organization, structure and curriculum of medical studies in Germany. The regulations governing these studies, called Approbationsordung, were reviewed and amended in 2002, in adaptation to the new rules created by the European Union. The curriculum dedicates six years and three months to the study and training of students (two years of basic sciences, three years of clinical sciences, and a final year dedicated to clinical work in hospital). Any candidate applying for a course at a German University must meet certain requirements, regardless of whether or not he or she is member of the EU. Assessment of progress is carried out at different levels during the course. Essential here is the state exam in Medicine, which is divided into two parts, the first part dealing with the basic and the second with the clinical period. The new Approbationsordung (AppOÄ) brought a series of changes that are still under implementation. Specialization takes place in the postgraduate period of medical studies. At the end of this period the doctor obtains a specialist (Facharzt) title granted by the College of Physicians. Traditionally the organization of these studies lies in the hands of the trainees themselves; however, this is lined up for substantial modification. As a specialist the doctor is obliged to participate in ongoing education programs, with periodic performance evaluation. A controversial topic at present is the Doctor title in Medicine and its medical relevance. Many research programs are emerging thematically in a clinical context and apparently some past deviations can be corrected. Links and sources to obtain information about studying in different faculties in Germany have been included.
Key words: Curriculum medicine. Evaluation. Germany. Postgraduate medical education. Undergraduate medical education.
RESUMEN
Este artículo da una visión general de la organización, la estructura y el currículo de estudios de medicina en Alemania. La normativa que regula estos estudios, denominada Approbationsordnung, fue revisada y modificada en 2002, adaptándola a las nuevas reglas creadas por la Unión Europea. El plan de estudios dedica seis años y tres meses al estudio y formación de los estudiantes (dos años de ciencias básicas, tres de ciencias clínicas y un último año dedicado al trabajo clínico en el hospital). Cualquier candidato que solicite una plaza para estudiar en una universidad alemana debe cumplir ciertos requisitos, independientemente de si proviene o no de un país miembro de la Unión Europea. La evaluación del estudio se lleva a cabo a diferentes niveles durante el curso. Esencial aquí es el examen de estado en medicina, que se divide en dos partes: la primera parte trata de las ciencias básicas y la segunda se refiere al período clínico. La nueva Approbationsordnung (AppOÄ) trajo consigo una serie de cambios que todavía están en fase de ejecución. La especialización se lleva a cabo en el período de posgrado de los estudios de medicina. Al final de este período, el médico obtiene un título especialista (Facharzt) otorgado por el Colegio de Médicos. Tradicionalmente, la organización de estos estudios está en manos de los propios alumnos, pero ello está en vías de sufrir una modificación sustancial. Como especialista, el médico está obligado a participar en los programas de educación continuada, con una evaluación periódica de sus rendimientos. Un tema controvertido en la actualidad es el título de Doctor en Medicina y su importancia médica. Muchos programas de investigación están surgiendo dentro de un contexto clínico, lo que puede contribuir a corregir algunas desviaciones del pasado a este respecto. Se han incluido enlaces web y fuentes para obtener información sobre los estudios en las diferentes facultades en Alemania.
Palabras clave: Alemania. Currículo de medicina. Educación médica de posgrado. Educación médica de pregrado. Evaluación.
Introduction
The Training Regulations (Ausbildungsordnung) in Germany had, from the beginning, four main objectives: 1st to unify the medical profession, 2nd to control the quality of education through state exams, 3rd to ensure scientific based education and practice of future physicians and 4th to adjust the catalogs of knowledge to scientific progress [1,2].
With the introduction of Trade Regulations (Gewerbeordnung) and Licensing Regulations (AppOÄ) in the federation of North German States in 1869 the image of the medical profession was unified in terms of medical training. In fact this image did not change until the EU created new requirements, valid for all EU-States [2,3].
In 1869 the quality of education was controlled by state exams, flanked by the obligatory participation in lectures, practicals and compliance with a minimum duration of studies. In 1970 a new AO was promulgated which reduced the length of study to 6 years, while modifying the catalog of knowledge required.
Over the past 100 years the balance between practical and theoretical education has undergone considerable change. Early last century most of the time was devoted to practical education. In following time, medical teaching became more theoretical and, the same time, more dependent on single chairs, not a situation favourable to the development of integrated medical thinking. The splitting up of interests that arose through chair-oriented study created serious problems with regard to study effectiveness and significantly extending study duration. The consequences for the education of physicians were remarkable. In recent decades all these trends have been corrected and corresponding changes are continuing, reflecting the aims of AppOÄ 2002 (law governing these studies that came into force in 2003) and the regulations issued for the education and training of physicians [4].
This paper deals with medical education in Germany, giving information on its organization and contents during undergraduate and postgraduate periods as well as considering briefly the situation of the continuing education (MCE) for practicing physicians.
Admission and allocation of study places
Abitur, the General Certificate for University Entrance, is a prerequisite for studying at a university in Germany. Approximately 39% of young school leavers pass Abitur [5]. Same level certificates obtained in other countries of the European Community (EU) are automatically recognized in Germany. Those obtained in countries outside the EU must undergo a process of equivalence assessment.
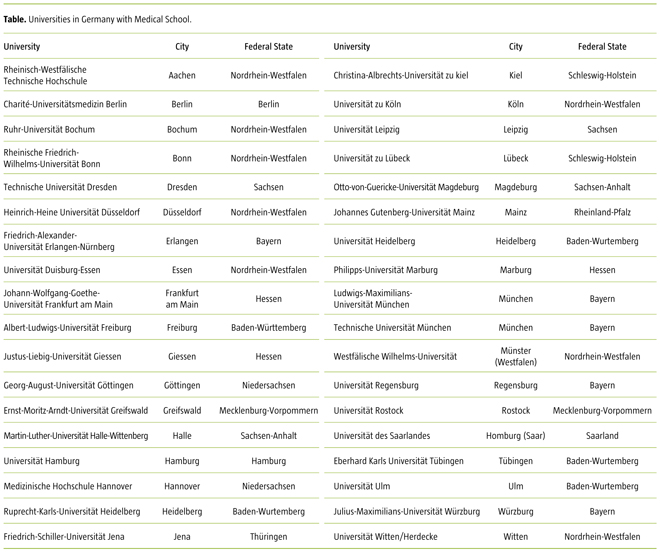
Germany has 36 state medical schools (Table)1. A total number of about 80,000 medical students are enrolled at the colleges listed above. At present about 10,000 students begin studies each year, while the number of graduates is about 6,000 per year [5]. As higher education falls within the competence of the Bundesländer (federal states) the universities may differ with regard to university tuition fees etc. (please refer to the respective university homepage). In Germany the number of study places available in medicine (as also with dentistry, veterinary medicine and pharmacy) is restricted by numerus clausus. For the academic year 2011-2012 there were approx. 37,400 applicants; only approx. 8,500 places are available for allocation. Admission to undergraduate medical studies is organized by a central national office, Stiftung für Hochschulzulassung (Foundation for University Admission: www.hochschulstart.de), where applicants have to register individually and exclusively online. The applicants are selected according to exactly defined regulations 2: 20% school leaving grading; 20% time of waiting after a prior application, 60% selected by the universities themselves according to self-defined criteria (e.g. school leaving grades, interviews, written tests, pre-university qualifications).
The criteria applied in these selection procedures may differ between Faculties, and for this reason some of them have reverted to the reinstatement of the so-called medical admission test (Test für Medizinische Studiengänge), that was used nationwide until 1996, and which is comparable to the American Medical College Admission Test (MCAT) [5-7].
A certain number of places is reserved for example for handicapped people, German army students, hardship applications or international students.
General information on the structure of medical studies
The undergraduate period
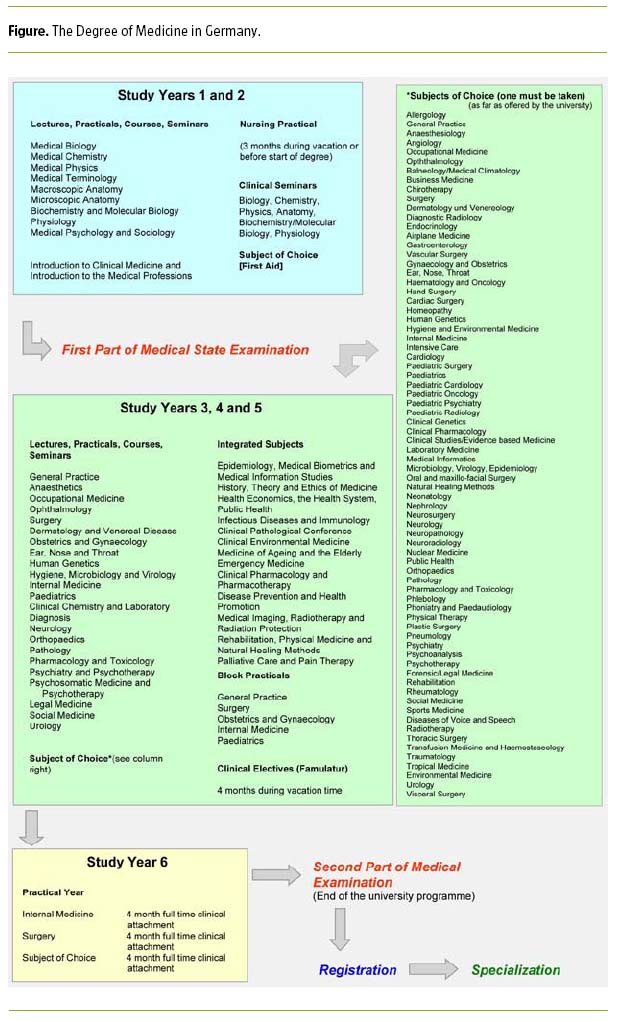
At present medical education in Germany includes the following [4,5]:
- A six-year medical degree, the last year of which comprises up to 48 weeks of practical training.
- A first aid course.
- Three months nursing experience.
- Four months of clinical electives.
- The Medical State Examination, which is split into two parts.
The time needed to obtain a degree in medicine, including the state exams, is six years and three months.
The medical State Examinations are taken as follows: a) the First Part of the State Examination after a study period of two years and b) the Second Part after a further four years including the Practical Year.
The conveyance of knowledge and the development of skills in medical teaching are achieved through the application of a number of various activities or strategies. Lectures, practical exercises and seminars are offered by the university, to ensure that the students receive the support needed to pass the state exams and become competent general practitioners.
Practical exercises are held, as far as possible, in small groups of students and are intended to enable the student, especially after the first state exam has been successfully completed, to become competent in medical practice (medical history taking, examination, diagnosis, therapy of patients, etc.). After the first part of the medical state exam, not less than 20 % of studying time should be spent in practicals, accompanied by theory learnt, for example in seminar groups.
Bedside teaching can only be carried out in small groups: a) teaching by demonstration on a patient in groups of no more than 6 students and b) examination of a patient by students with no more than three students per group.
In teaching with the help of patients half the available time is dedicated to demonstrations and the other half to the examination of the patient. The total number of hours of bedside teaching is not less than 476. Practical blocks for a period of one to six weeks are organized in order to teach the strategies of differential diagnosis and therapeutic treatments of daily medicine. After the first part of the medical examination at least 20% of practicals have to be in blocks.
The seminars aim to teach medical practice in greater depth and comprise a mixture of lectures, presentation of patients, discussions, practical exercises and students own study preparation. The number of students per seminar should not exceed 20. Moreover, topics emerging from the practical exercises, seminars and lectures can be treated in groups in which the students have the opportunity to learn how to handle problems independently. Such an approach is particularly important when clinical problems are under discussion.
These classical strategies are additionally supported in the German medical schools by modern computer learning systems and simulators offering a wide range of educational instruments that have progressively been incorporated into the curricula, first in clinical (emergency medicine, anesthesiology, radiology...) and later in preclinical (anatomy, physiology...) disciplines, thus improving the learning facilities [8-12].
Courses, practicals, seminars and lectures are regularly evaluated. The students receive certificates for successful participation in the respective teaching events, which are necessary to achieve eligibility for the state exams. A subject of choice has to be completed in the period before the first part of the Medical State Exam and a second one before the commencement of the practical year.
The University usually offers courses separately for the first and the second part of the medical examination; the student can freely choose two subjects. Performance in the elective subjects, clinical courses and practices is evaluated by means of appropriate tests.
Practical year
The practical year is the last year of medical study. It begins in the second half of April or October and is divided into 16-week sections in Internal Medicine, Surgery and a subject of choice (General Practice or one of the other clinical areas).
The practical year either takes place in the university clinics or in other hospitals or general medical practices, chosen for their suitability by the university itself.
The main objective of the practical education in this year could be summarized by saying that it is the practical application of the theoretical knowledge gained during the first five years of study. The student must participate in the daily activities of the hospital and be actively involved in clinical and clinical-pathological conferences, and in therapeutic decisions, with the help of the medical staff of the institution.
First aid
The mandatory training in First Aid and Emergency Medicine takes place in the preclinical study years (Emergency Medicine is taught in more detail during the clinical years). This training can also be carried out in non-university hospitals or institutions (e.g. Red Cross), but must be certified before entering for the first part of Medical State Exam.
Nursing training
This training, which lasts for three months, has either to be completed before studies commence or during the academic break prior to registration for the first part of the Medical State Exam. During this time the student acquires basic subject knowledge and also gains an insight into hospital work.
Clinical elective
The clerkship (Famulatur) 3 for medical students lasts four months, which should be completed as practical training in a hospital or a doctor's surgery.
The internship is to be completed between the first and second part of the medical examination and, as stipulated in the Approbationsordnung, comprises two months in a hospital and a month spent in a doctor's office. The remaining month can be either in a hospital or a doctor's office.
Clerkships in an outpatient clinic, a clinic or emergency unit can be declared as Praxisfamulatur. Some universities offer the possibility of a clerkship in certain clinical and theoretical university institutes (e.g., forensic medicine, pathology, pharmacology, microbiology) as an equivalent to a Praxisfamulatur. In some Bundesländer (federal states), such clerkships are also rated as Praxisfamulatur even if they are time-split.
Exams and assessment process
The first and second parts of the Medical State Exam comprise written, practical and oral tests. Each part of the state exam can only be repeated twice.
Written tests
The Institute for Medical and Pharmaceutical Examination Questions (IMPP) is a central institution of the German federal states with its headquarter in Mainz. The institute was founded in 1974 and it is dedicated to the creation and evaluation of the written parts of the state examinations (multiple choice tasks) in medicine and pharmacy. For this purpose, it also created the so-called object- or theme-catalogs, which are an important source of orientation for students and teachers.
Oral tests
The oral practical examinations of the medical state exams are performed by an examination committee established by the responsible federal state board. For the first part of the exam, the committee consists of two or maximum three examiners, whereas the second part may be held by a minimum of 3 or a maximum of 4 examiners. The committees may comprise faculty and teaching staff members, but also competent individuals from outside the university can be engaged particularly for the second (clinical) part of the exam.
Some comments on the examination procedure
In the first part of the state exam the student's knowledge and skills are assessed according to the subjects listed in the figure. The written test includes 320 multiple-choice questions. Prior to the oral test the candidate is presented with some exercises, the results of which are then presented to the committee. This test lasts for 45 to a maximum of 60 minutes per candidate.
The items or topics corresponding to the second part of the state exams are listed in the figure. The written part of this examination includes testing knowledge and abilities of the candidate; he or she should possess the qualities needed to become a doctor capable of making independent and responsible decisions. The exam is built around clinical situations and case presentations and the subject matters are mainly the practical clinical demands on a doctor, the most important clinical disease pictures and questions covering all subjects and common problems. The exam takes place on three consecutive days and lasts five hours each time. There are 320 multiple-choice questions.
The oral-practical part of the examination takes place on two days. It lasts a minimum of 45 and a maximum of 60 minutes per candidate (with a maximum of four candidates per group) on each day. The first day is the proper practical exam with patient presentation and including patient-related questions from internal medicine, surgery and from the chosen subject from his practical year. Prior to commencement of the examination, the committee presents one or more patients to the candidate, who has to record the clinical history and conduct a clinical examination of the patient. After that the candidate prepares a report, which includes medical history, examination, diagnosis, prognosis and treatment/therapy as well as a synopsis of the case. Upon completion of the report, it is retained by a member of the committee and later presented during the oral exam, being relevant to the final grade.
The postgraduate period
The qualification of specialist (Facharzt) requires clinical training in the chosen field over a period of several years. This training /education is defined by a framework of educational stipulations laid down by the Medical Board (Ärztekammer) and usually commences immediately after undergraduate studies.
In Germany - unlike other countries - medical specialist training (Weiterbildung) is not restricted exclusively to universities. Even though the curriculum is defined by regulations of the German Medical Board (Bundesärztekammer) and the respective Federal State Medical Boards (Landesärztekammern) fulfillment of the requirements with regard to training content and duration is widely in the hands of the trainee, who is often confronted with an education or training less formalized and not conventionally organized [4,5,13].
This state of affairs is considered unsatisfactory and changes towards a more structured organization of specialist training are already under consideration. This new concept of specialization training not only covers trainee education but also pursues improvements in working conditions (particularly personnel and equipment facilities) and takes into consideration the dedication of the existing teaching staff, which is very often completely overrun by its own working volum [4,14].
With regard to continuing education, or, as it is now called, continuing professional development 4,5, it should be emphasized that the medical specialist is required to regularly attend lectures, participate in conferences, workshops, or be involved in continuing education circles using for instance, modern computer systems. Points are awarded for participation in these activities (250 in 5 years minimum), otherwise specialists may be penalized with cuts in the budget. This obligation applies not only to free-lance doctors but also to those working in clinics and hospitals. The system still suffers from certain deficiencies, but there are initiatives to improve the situation and one of them is the creation of departments of medical education in the German medical schools. In support of these developments, a Master in Medical Education has already been introduced in some faculties [4].
Other considerations
Following the success of the reform of medical studies in Germany brought about by the AppOÄ 2002, now, as already stressed, it is necessary to structure the education in the postgraduate period, mainly by improving and developing the curriculum. Initial experience in this area has produced encouraging results [15].
Furthermore, the question arising from the Bologna process, as to whether undergraduate study courses should be subject to further modification, has yet to be decided. Although Germany, from the beginning, supported the Bologna process, German medical schools and medical organizations fiercely argue the application and consequences in this field. Promises of student mobility, flexibility and comparability of the studies seem only partly fulfilled. On the other hand, the Bachelors and Masters division is facing severe criticism, especially in view of the work perspective for these graduates.
Another important question refers to the postgraduate doctoral degree in medicine [16]. In an excellent article Nikendei et al [4] discusses the value of the title "Doctor of Medicine" in the future. This title is not a condition sine qua non to undertake postgraduate studies or to practice medicine. In Germany about 90% of the cohort obtains the title Doctor in Medicine. However, this does not necessarily guarantee improved patient care. On the contrary, the pursuit of doctoral work in basic scientific research projects can often create delays in the completion of the study of medicine, to the extent that students cannot devote sufficient time to the development of clinical skills, attendance at classes etc.
The situation is changing and the attainment of a Doctor title is currently formalizing a contract signed between the Faculty, doctoral instructor and doctor candidate. This will benefit all participants and enable, from the beginning, assessment of the concept or topic, allowing the exclusion of those projects which do not fulfill the required conditions of scientific quality.
The scientific training of medical students seems to be most promising and beneficial if it develops within graduate clinical research programs [4,17,18].
Concluding remarks
Education in the field of health sciences is a process of ongoing improvements and adaptations. The new regulations governing the Physicians degree (AppOÄ) in Germany has given teaching a high-focus priority position in university activities and is well attested by excellent projects underway in many German universities [4,6,7,19], created to enable future physicians address the existing needs. This paper is based on the organization and structure of medical education after the application of the new law of regulation, which is still being implemented. Obviously, a thorough analysis of the teaching activities in the 36 medical schools exceeds the scope of this article. However, this is very necessary and will have to be addressed with the creation of a suitable system for regular evaluation and accreditation of these institutions.
Acknowledgments
The authors are indebted to Mrs. Ann Soether for revising the English version of the manuscript.
1 http://www.medknowledge.de/germany/study/medschools/german_medical_schools.htm, and a medical school located in a semi-private university (http://www.uni-wh.de/gesundheit).
2 Verordnung über die zentrale Vergabe von Studienplätzen durch die Stiftung für Hochschulzulassung (http://hochschulstart.de/fileadmin/downloads/Gesetze/G03.pdf).
3 http://www.gesetze-im-internet.de/_appro_2002/__7.html.
4 Transparenz und Leistungsfähigkeit im deutschen Gesundheitswesen. Beschlussprotokoll des 106. Deutschen Ärztetages 2003.
5 (Muster-) Satzungsregelung Fortbildung und Fortbildungszertifikat. Beschlussprotokoll des 107. Ärztetages 2004.
![]() Correspondence:
Correspondence:
Pedro Mestres-Ventura,
Prof. Dr. med. Institute of Anatomy and Cell Biology.
Faculty of Medicine.
Saarland University.
66421 Homburg Saar (Germany).
Fax: +49 6841/16-26121
E-mail: pedro.mestres@uks.eu
Conflict of interests: None declared.
References
1. Bargmann W. Medical education in Germany. J Med Educ 1957; 32: 422-6. [ Links ]
2. Steudel WI. 100 Jahre Reform des Medizinstudiums in Deutschland. In Mestres P, ed. Perspektiven des Medizinstudiums. St. Ingbert: Röhrig Universitätsverlag; 1999. p. 93-112. [ Links ]
3. Mestres P. Vorwort. In Mestres P, ed. Perspektiven des Medizinstudiums. St. Ingbert: Röhrig Universitätsverlag; 1999. p. 5-11. [ Links ]
4. Nikendei C, Weyrich P, Jünger J, Schrauth M. Medical education in Germany. Med Teach 2009; 31: 591-600. [ Links ]
5. Chenot JF. Undergraduate medical education in Germany. GMS Ger Med Sci 2009; 7: Doc 2 [ Links ]
6. Hissbach J, Klusmann D, Hampe W. Reliability of a science admission test (HAM-Nat) at Hamburg medical school. GMS Ger Med Sci 2011; 28: Doc 44. [ Links ]
7. Huwendiek S, Kadmon M, Jünger J, Kirschfink M, Bosse HM, Resch F, et al. Umsetzung der deutschen Approbationsordnung 2002 im modularen Reformstudiengang Heidelberger Curriculum Medicinale (HeiCuMed). ZFHE 2008; 3: 17-27. [ Links ]
8. Cook DA. The research we still are not doing: an agenda for the study of computer-based learning. Acad Med 2005; 80: 541-8. [ Links ]
9. Eich C, Timmermann A, Russo SG, Nickel EA, McFadzean J, Rowney D, et al. Simulator-based training in paediatric anaesthesia and emergency medicine -thrills, skills and attitudes. Br J Anaesth 2007; 98: 417-9. [ Links ]
10. Zausig YA, Bayer Y, Hacke N, Sinner B, Zink W, Grube C, et al. Simulation as an additional tool for investigating the performance of standard operating procedures in anesthesia. Br J Anaesth 2007; 99: 673-8. [ Links ]
11. Ten Eyck RP. Simulation in emergency medicine training. Pediatr Emerg Care 2011; 27: 333-44. [ Links ]
12. Pommert A, Höhne KH, Burmester E, Gehrmann S, Leuwer R, Petersik A, et al. Computer-based anatomy: a prerequisite for computer-assisted radiology and surgery. Acad Radiol 2006; 13: 104-12. [ Links ]
13. Plat E, Scherer M, Bottema B, Chenot JF. Postgraduate training for general practitioners in The Netherlands -a model for Germany? Gesundheitswesen 2007; 69: 415-9. [ Links ]
14. Harden RM. Trends and future of postgraduate medical education. Emerg Med J 2006; 23: 798-802. [ Links ]
15. Bosse HM, Nikendei C, Hoffmann K, Kraus B, Huwendiek S, Hoffmann GF, et al. Communication training using 'standardized parents' for paediatricians -structured competence-based training within the scope of continuing medical education. Z Ärztl Fortbild Qualitätssich 2008; 101: 661-6. [ Links ]
16. Díez C, Arkenau C, Meyer-Wentrup F. The German medical dissertation -time to change? Acad Med 2000; 75: 861-3. [ Links ]
17. Hartmann M, Wild B, Herzog W, Nikendei C, Zipfel S, Henniggsen P, et al. Der klinische Forscher in der psycho-somatischen Medizin: Status, Kompetenzen und Leistungen. Phychother Psychosom Med Psychol 2008; 58: 230-7. [ Links ]
18. Löwe B, Hartmann M, Wild B, Nikendei C, Kroenke K, Niehoff D, et al. Effectiveness of a 1-year resident training program in clinical research: a controlled before-and-after study. J Intern Med 2008; 23: 122-8. [ Links ]
19. Dieter PE. Quality management of medical education at the Carl Gustav Carus Faculty of Medicine, University of Technology Dresden, Germany. Ann Acad Med 2008; 37: 1038-40. [ Links ]











 text in
text in