Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista de Psicología del Trabajo y de las Organizaciones
versión On-line ISSN 2174-0534versión impresa ISSN 1576-5962
Rev. psicol. trab. organ. vol.30 no.3 Madrid dic. 2014
https://dx.doi.org/10.1016/j.rpto.2014.11.001
Overcoming job demands to deliver high quality care in a hospital setting across Europe: The role of teamwork and positivity
La superación de las exigencias laborales para ofrecer una elevada calidad asistencial en el ámbito hospitalario en Europa: papel del trabajo en equipo y la positividad
Patrícia L. Costaa, Ana M. Passosa, Sílvia A. Silvaa, Ema Sacadura-Leiteb,c,d, Susana M. Tavaresa, Florina Spanue, Elitsa Dimitrovaf, Vera Basarovskag,h,i, Milan Milosevicj, Meral Turkk, Efharis Panagopouloul and Anthony Montgomerym
aInstituto Universitário de Lisboa – ISCTE-IUL, Lisbon, Portugal
bOccupational Health Department of Hospital de Santa Maria /CHLN, Lisbon, Portugal.
cNational School of Public Health /New University of Lisbon, Lisbon, Portugal.
dCMDT - Centro de Investigação da Malária e Doenças Tropicais - Public Health, Lisbon, Portugal
eDepartment of Psychology, Babes-Bolyai University, Cluj-Napoca, Romania
fInstitute for Population and Human Studies, Bulgarian Academy of Sciences, Bulgaria
gNeuropsychiatric Department, Institute of Occupational Health of RM, Skopje, Macedonia.
hWHO Collaborating Centre.
iGA2LEN Collaborating Centre
jSchool of Medicine, University of Zagreb, Croatia
kDepartment of Public Health, Ege University, Turkey
lMedical School, Aristotle University of Thessaloniki, Greece
mDepartment of Education and Social Policy, University of Macedonia, Thessaloniki, Greece
Financial Support: The research leading to these results has received funding from the European Union's Seventh Framework Programme [FP7-HEALTH-2009-single-stage] under grant agreement no. [242084].
ABSTRACT
Health care professionals deal on a daily basis with several job demands - emotional, cognitive, organizational and physical. They must also ensure high quality care to their patients. The aim of this study is to analyse the impact of job demands on quality of care and to investigate team (backup behaviors) and individual (positivity ratio) processes that help to shield that impact. Data was collected from 2,890 doctors and nurses in 9 European countries by means of questionnaires. Job demands have a negative impact on the quality of care delivered by health professionals. Backup behaviors had a mediating effect between job demands and quality of care. Also, the positivity ratio of professionals (ratio of positive and negative emotions experienced) was also found as a significant mediator between most job demands and quality of care dimensions. Finally, we found a double mediation between most job demands and quality of care, where backup behaviors influenced the positivity ratio. Quality of care in hospitals is closely related to job demands. Hospital managers should consider the importance of cooperation within health care professionals' teams and ought to find ways to develop teamwork in order to promote patients' safety.
Key words: Job demands. Quality of care. Teamwork. Positivity.
RESUMEN
Los profesionales de la salud tratan a diario con múltiples exigencias laborales -emocionales, cognitivas, organizacionales y físicas. También deben garantizar la máxima calidad de atención a sus pacientes. El objetivo de este estudio es analizar el impacto de las demandas laborales en la calidad de los cuidados y de investigar los procesos de equipo (backup behaviors) e individuales (positivity ratio) que ayudan a proteger al trabajador de ese impacto. Se recogieron datos de 2.890 médicos y enfermeros en 9 países europeos a través de cuestionarios. Las demandas laborales tienen un impacto negativo en la calidad de los cuidados proporcionados por profesionales de la salud. Los procesos de equipo (backup behaviors) tuvieron un efecto de mediación entre las demandas del trabajo y la calidad de los cuidados. Además, la ratio de positividad de los profesionales (proporción de emociones positivas y negativas) también se encontró como un mediador importante entre la mayoría de demandas de trabajo y la calidad del cuidado. Por último, se encontró una doble mediación entre la mayoría de las demandas de trabajo y calidad de la atención, donde los procesos de equipo influyeron en la ratio de positividad. La calidad de los cuidados proporcionados en los hospitales está muy relacionada con las exigencias del trabajo. Los directores de hospitales deben considerar la importancia de la cooperación entre equipos de profesionales de salud y encontrar formas de desarrollar el trabajo en equipo con el fin de promover la seguridad de los pacientes.
Palabras clave: Demandas laborales. Calidad asistencial. Trabajo en equipo. Positividad.
Working in hospitals as a health care professional (HP) is demanding. Doctors, nurses, and assistants must deal, on a daily basis, with emotional situations, such as the suffering of patients and relatives, cognitive challenges (for example, timely decision making and analysing several indicators in order to establish a diagnostic and a treatment plan), interpersonal tensions (conflicts between different specialties or professionals, uncooperative patients, impatient relatives), physical hassles (e.g., working nights, lifting heavy patients), and logistic complexity, such as the lack of necessary resources, time consuming bureaucratic processes, and heavy workload (e.g., Ghodse & Galea, 2009). High rates of burnout are reported in health care professionals in both Europe and the U.S. (Aiken et al., 2012; Soler et al., 2008). Consequently, the well-being and health of HPs is likely to be impaired, and their ability to work effectively may also be diminished. Stress, anxiety, and burnout have consistently shown positive relationships with decreased performance in HPs and also with maladaptive coping strategies, such as substance abuse (Firth-Cozens, 1995). Nonetheless, while working under these conditions, health professionals must assure that all the patients are given the best possible quality of care (QoC). Indeed, the quality of organizations is one antecedent of its competitive advantage. Considering quality of care in health services, there are also other fundamental issues at stake, namely human life, human rights, and human dignity. Yet, the Institute of Medicine (1999) reports that tens of thousands of American patients die every year due to suboptimal care. The existence of quality of care problems is widespread and is not restricted to the United States. For example Bartlett, Blais, Tamblyn, Clermont, and MacGibbon (2008) claim that in Norway three people might die every day due to poor hospital quality. Also, according to the European Commission (2008), it is estimated that between 8% and 12% of patients admitted to hospitals will suffer from adverse effects while receiving healthcare. Therefore, patient safety was identified as a key area for action in the Commission's Health Strategy White Paper of October 2007.
Considering the importance of quality within healthcare, the aim of the present study is to analyse the impact of job demands on quality of care and to investigate possible team and individual processes that will help to buffer the impact of high work demands on the quality of care delivered to patients, therefore ensuring their safety.
Quality of Care - A Multidimensional Concept?
According to McGowan et al. (2011), the definition and measurement of quality of care in healthcare lack consistency across studies. The Institute of Medicine defines QoC as "the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge" (IOM, 1999). This institute defines six main pillars fundamental for delivering a high quality of care: health care must be safe, effective, patient-centred, timely, efficient, and equitable (IOM, 2001). For another author (Donabedian, 1980), QoC is also a multifaceted concept. It encompasses health outcomes, the process of care delivery (such as information obtained and coordination) as well as the structure where it is delivered (equipment, administrative processes, etc.). Campbell, Roland, and Buetow (2000) define QoC as "whether individuals can access the health structures and processes of care which they need and whether the care received is effective" (p. 1614). For the authors, the consequences of care reflect the effectiveness of the structure and processes and are assessed by the health status of patients and by user evaluation.
Job demands in Hospital Settings
According to the Job Demands-Resources Model (Demerouti, Bakker, Nachreiner, & Schaufeli, 2001), job demands are "those physical, social, or organizational aspects of the job that require sustained physical or mental effort and are therefore associated with certain physiological and psychological costs" (p. 501). Within job demands that can be found in a hospital setting, we can name, for example, time pressure, physical workload, shift work, or recipient contact. According to the model, when meeting those demands requires a high level of effort from the employee and an adequate recovery from that effort is not possible, then the development of job strain develops. Consequently, workers may develop a health impairment process (because of an increased autonomic and endocrine activation and of the increased subjective effort) and their task performance may deteriorate indirectly because of the need for strategic adjustments (e.g., narrowing of attention) and of fatigue after-effects, such as risky choices.
An extensive review of all the possible job demands found in hospital settings is beyond the scope of this paper. As an example, Ecklebery-Hunt et al. (2009) searched for the antecedents of residents' burnout symptoms and found several factors: lack of control over schedule, poor relationships with colleagues, difficult and complicated patients, excessive paperwork, not enough time in the day, and perfectionism (to name a few). In Isikhan, Gomez, and Danis' (2004) study, unfairness in promotion opportunities, imbalance between jobs and responsibilities, conflict with colleagues, lack of appreciation of efforts by superiors, responsibilities of role, long and tiring work hours, inadequacy of equipment, and problems experienced with patients and their relatives were the main factors associated with the stress experienced by health professionals working with cancer patients. Other studies focused on specific stressors and their relationship with health professionals' well being, such as aggression towards them (e.g., Winstanley & Whittington, 2004).
These job demands impact on professionals' well-being and performance. Shanafelt, Bradley, Wipf, and Back (2002), as well as Toral-Villanueva, Aguilar-Madrid, and Juárez-Pérez (2009) concluded that the presence of stressors and acute stress on HPs was associated with self-reported suboptimal practices. Other studies report the relationship between job demands and decreased productivity (e.g., Kazmi, Amjad, & Khan, 2008) and between job stress and increased medical errors (e.g., Fahrenkopf et al., 2008; West et al., 2006) and mental health impairment in HPs, mainly depression and anxiety (e.g., Caplan, 1994; Chambers, Wall, & Campbell, 1996; Toral-Villanueva et al., 2009; Weinberg & Creed, 2000).
Therefore, considering this evidence, it is likely that job demands at the hospital will impact on quality of care either directly (for example, lack of resources needed, too many patients to diagnose in little time, etc.) or indirectly (through the depletion of health and cognitive and emotional resources of HPs).
H1. Job demands are negatively related to quality of care.
Job Resources in Hospital Settings
Parallel to the existence of job demands, in every job there are also job resources, defined as the physical, psychological, social, or organizational aspects of the job that reduce job demands and the associated costs, that are in achieving work goals, and stimulate personal growth and development (Demerouti et al., 2001). Resources are seen as motivation boosters, either through an intrinsic or extrinsic path. Some authors (e.g., Richter & Hacker, 1998) posit the resources can be either organizational (such as feedback, job control, supervisory support, or task variety) or social (e.g., support from colleagues and peers). Xanthopoulou Bakker, Demerouti, and Schaufeli (2006) proposed also personal resources (self-efficacy, organizational-based self-esteem and optimism) as important in facing demanding work environments. In a similar reasoning, Sweetman and Luthans (2010) suggest that self-efficacy, optimism, hope, and resilience (that they name as PsyCap) are positive agentic resources that have a motivational impact on workers and leads to desired work outcomes.
Another important premise of the Job Demands-Resources model (J D-R) is that job resources will buffer the impact of job demands on job strain. More specifically, resources will have the potential to reduce the tendency of organizational properties to become or generate stressors, to alter the perceptions evoked by those stressors, or to reduce the health impairment consequences of the stress response. Finally, the model postulates that the positive impact of job resources on both diminishing the negative impact of job demands and fostering workers motivation will be higher in situations where job demands are high. This model has received empirical support across several occupations (e.g., Bakker, Demerouti, & Schaufeli 2003; Bakker Demerouti, & Verbeke, 2004; Demerouti et al, 2001; Hakannen, Bakker, & Schaufeli, 2006).
In the present study, we will focus on two possible job resources that, to our knowledge, have not been studied in the hospital context: backup behaviors of team members and individual emotions. The analysis of these specific resources is critical, for HPs often work in teams (e.g., surgical teams) and the ability of those teams to perform well in a context of high demands is critical for patients' health outcomes and, in more general terms, for quality of care. Indeed, as Krokos, Baker, Alonso, and Day (2009) point out, "health-care workers perform interdependent tasks (e.g., removing a patient's appendix) and function in specific roles (e.g., surgeon, anesthesiologist, surgical assistant) while sharing the common goal of providing safe care to patients" (p. 384-385). Moreover, the emotions of individual HPs accounts for the emotional dimension of work, often overlooked by scholars (Ashkanasy, 2003), should be taken into account. Since some of the demands faced by health professionals have an emotional nature, we must, then, consider emotional resources as important factors for health professionals well-being and effectiveness.
Backup Behaviors in Teams
In 2003, Porter et al. proposed the construct of backing up behaviors, defined as "the discretionary provision of resources and task-related effort to another member of one's team that is intended to help that team member obtain the goals as defined by his or her role when it is apparent that the team member is failing to reach those goals" (p. 319-320). According to those authors, back up behaviors emerge when team members recognize that the distribution of workload is inaccurate and may cause trouble in task and social performance of their team. For example, backup behaviors happen when a team member fills in for a co-worker who is unable to meet the demands of his or her role at a specific moment. They can be either physical (helping lifting a heavy patient or dealing with complex equipment) or verbal (suggestions, cautioning advice, or feedback).
Within the literature on teams, backup behaviors have been labelled one of the "big five" in teamwork (Salas, Sims, & Burke, 2005), together with team leadership, mutual performance monitoring, adaptability, and team orientation. Indeed, it is seen as a skill "at the heart of teamwork, for it makes the team truly operate as more than the sum of its parts" (McIntyre & Salas, 1995, p. 26). According to Salas, Rosen, Burke, and Goodwin (2009), backup behaviors support team performance in three ways: allowing members to provide (1) assistance during task performance, (2) timely feedback so that performance processes can be adjusted, and (3) help to teams, so that dynamically adjust their performance strategies and processes when a detrimental imbalance of the workload is detected.
Therefore, the relevance of backup behaviors for hospital teams social and task performance is explained by the teams' ability to reduce work overload (considered a job demand) and by its impact on team processes, resulting in a higher degree of adaptability in face of environmental and situation changes. Faced with challenging demands, hospital teams will differ on the degree of backup behaviors they provide team members. Depending on the accuracy and timeliness of these backup behaviors, the impact of the job demands on quality of care may be diminished - workload is better divided between HPs, reducing the degree of stress, and diminishing the need to rush or, in other words, reducing job demands.
H2. Backup behaviors will mediate the impact of job demands on quality of care.
Positivity
While working at the hospital, HPs have the opportunity to experience many positive and negative feelings. This is true for every job and maybe more so in a health context, where not only is there the need to deal with people but also the emotional valence of disease, ageing, and suffering. Being able to maintain a positive mood may, thus, be a challenge.
Following the trend of positive psychology (Seligman & Csikszentmihalyi, 2000), Fredrickson and Losada (2005) proposed that the positivity ratio (ratio of pleasant feelings and sentiments to unpleasant ones over time) would predict subjective well-being. The benefits of positive affect have already been documented and ranged from resilience and physical and mental health (Fredrickson, Tugade, Waugh, & Larkin, 2003) to happiness (Fredrickson & Joiner, 2002) and increased intuition (Bolte, Goschkey, & Kuhl, 2003) and creativity (Isen, Daubman, & Nowicki, 1987). Indeed, according to the broaden-and-build theory of positive emotions (Fredrickson, 2001), positive emotions will widen the array of thoughts and actions available, resulting in more behavioral flexibility, generativity, and adaptability. Moreover, overtime, the benefits of the broader repertoires of thought and action will, as a consequence, build enduring personal resources, such as coping mechanisms, social connections, and environmental knowledge.
Therefore, the positivity ratio of HPs is likely to influence how they are able to cope with job demands - the higher the positivity the more likely they are to be able to overcome difficulties - to be able to find more than one solution for a problem and find creative solutions for problems. Consequently, the quality of care they will be able to deliver to patients will also be increased in a context of a high positivity.
H3. The positivity ratio of HPs will mediate the impact of job demands on quality of care.
Backup Behaviors and Positivity - A Process Relationship
Receiving a helping behavior from a coworker in a moment where one feels that he or she is unable to successfully accomplish his or her tasks is likely to generate a positive feeling. According to Bakker and Demerouti (2007) social support is the best well-known variable that buffers against job strain. The receiver of backup behaviors will perceive social support from the colleagues and also may feel less pressure from an excessive workload - all of these are events that most likely will be perceived as positive. Therefore, the presence of backup behaviors in a team is likely to influence the positivity ratio of team members, which, in turn, will impact on the quality of care they are able to provide patients with, according to the broaden-and-build theory of positive emotions (Fredrickson, 2001). It wouldn't be completely odd to consider a reverse causality relationship: the higher the positivity ratio the higher the well-being and happiness of an individual and his/her willingness to invest in social relationships. Nonetheless, backup behaviors are not just helping or social behaviors - by definition they happen in a context of an uneven distribution of workload. Therefore, the existence of an uneven distribution of workload is a precondition for backup behaviors to happen; only after those backup behaviors will team members increase their positivity ratio, since before that they were experiencing trouble in workload distribution.
H4. The impact of job demands on quality of care is sequentially moderated by backup behaviors and positivity.
Method
Participants and Procedure
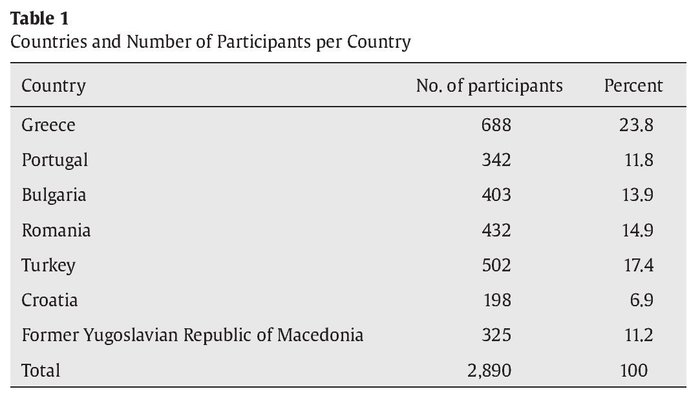
Data were collected within the scope of ORCAB project ("Improving quality and safety in the hospital: The link between organizational culture, burnout and quality of care"), a 7th Framework Program financed by the European Commission. A total of 9 European countries participated in this project and six countries collected the same data on one or more teaching hospitals between September and December 2011 (cf. Table 1).
After the formal agreement of the Administration Boards and Ethics Committees of the participating hospitals, questionnaires were either emailed to all of the health professionals or collected on site. From all countries, 2,890 health professionals completed the questionnaire. On average, participants were 39 years old (SD = 10.26) and had been working at their hospital for, in average, 12 years (SD = 10.73). Seventy four percent of participants were female. Considering their staff position at the hospital, 50.5% were nurses, 22.1% were physicians, 20% were residents and 7.4% had other positions (e.g., pharmaceutics, social workers, etc.).
Measures
The following scales were used in the present study:
Job demands. The Hospital Work-Experience Scale1 was constructed as part of the ORCAB project (ORCAB, 2012). The scale comprised six items (Cronbach's α = .57) for organizational demands (e.g., "The communication between hospital departments is problematic"), six items (Cronbach's α = .68) for emotional demands (e.g., "I have to deal with verbally abusive patients"), seven items (Cronbach's α = .78) for physical/environmental demands (e.g., "I have too much paperwork to do") and five items (Cronbach's α = .73) for cognitive demands (e.g., "I have to take decisions under time pressure"). Participants answer in a 5-point scale (1 = never, 5 = always).
ORCAB Quality of Care Scale1. In order to capture the complexity and multidimensionality of the construct, a three-factor model of QoC was developed via the ORCAB project (Orcab Report, 2012). The ORCAB project is concerned with improving quality and safety in the hospital via the link between organizational culture, burnout, and quality of care. This multi-centre study among hospitals in 9 European countries utilized systematic reviews, focus groups, surveys, and action research to identify the key mechanisms within quality of care.
Patient Centeredness, Effectiveness, and Personal Barriers to Providing Good QoC were identified as key dimensions of QoC. Informed by the IOM's framework, the project used a bottom-up approach to develop both a model and an instrument that measures the construct. Items were generated based on interviews and focus-groups conducted with HPs - certified physicians, residents and nurses - in seven European countries. The three-factor model was found to be consistent across HPs' organizational position and gender.
Patient Centeredness captures the quality of the one-on-one interaction with patients, referring to the availability of HPs in terms of time, information provided to patients, pleasantness, and equity in providing medical care. Effectiveness captures the effort to provide the best medical care possible, considering the resources available, mainly in terms of expertise. Personal Barriers to Providing Good QoC captures failures to perform as expected when interacting with patients as a result of personal hindrances interfering with professional life.
The scale comprises the dimensions of patient centeredness, measured with four items (Cronbach's α = .77) (e.g., "I was able to ensure good and pleasant communication with patients"), effectiveness, measured with three items (Cronbach's α = .70) (e.g., "I was able to provide the patient with the best medical care available") and personal barriers to providing good care, measured with two items (Cronbach's α = .67) (e.g, "Sometimes my personal problems impact on the quality of care"). Participants answer in a 10-point scale (1 = never, 10 = always).
Backup behaviors. Backup behaviors were assessed using four items (Cronbach's α = .68) from the Hospital Survey on Patient Culture, US Agency for Healthcare Research and Quality (2004) (e.g., "When one area in this unit gets really busy, others help out" ; "When a lot of work needs to be done quickly, we work together as a team to get the work done"). Participants answer in a 5-point scale (1 = never, 5 = always).
Positivity. We computed the positivity index by the ratio of positive/negative emotions. Positive and negative emotions were assessed by the short version (Thompson, 2007) of PANAS (Watson, Clark, & Tellegen, 1988), including five positive (Cronbach's α = .73) (e.g., inspired, active) and five negative (Cronbach's α = .70) (e.g., ashamed, afraid) emotions. Participants answer in a 5-point scale (1 = very slightly or not at all, 5 = extremely).
Statistical Analysis
Considering the low reliability (Cronbach's α = .57) of the scale measuring organizational demands, this scale was removed from further analysis. For testing hypothesis 1, we calculated simple linear regressions in SPSS, using the method Enter (inclusion of all variables at the same time). In order to test hypothesis 2 to 4, we followed the method presented by Preacher and Hayes (2008) and used the SPSS PROCESS macro provided by Hayes (2012) to run the analysis. These authors propose a procedure for assessing the significance of the indirect effects of one variable on another through the influence of the mediator, which is in line with the objectives of the present paper. Their method allows for testing indirect effects in samples where researchers should not theoretically assume a normal distribution, by using bootstrapping, a nonparametric resample procedure. The output of the analysis yields confidence intervals for the indirect effects. Since the authors strongly recommend using the bootstrap procedure, we decided to perform our analysis in accordance, using a bootstrapping of 5,000 samples in each analysis, as recommended (Preacher & Hayes, 2008). For hypothesis 2 and 3 (simple mediations), we used the model 4 of the PROCESS macro (Hayes, 2012).
Results
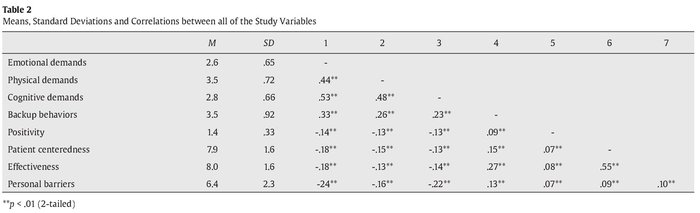
In Table 2 we present the correlations and descriptive statistics for all of the variables in the study. All of the variables were significantly correlated (p < .05), and the correlations were in the expected direction. Job demands showed positive and correlations between them (values ranging from r = .48 between physical and cognitive demands to r = .44 between physical and emotional demands). All of the job demands correlated negatively with backup behaviors (values ranging from r = -.26 for physical demands to -.23 for cognitive demands) and, with smaller magnitude, with positivity (r = -.14 for emotional demands and -.13 for physical and cognitive demands). All of the dimensions of quality of care (patient centeredness, effectiveness, and personal barriers) correlated negatively with all of the job demands, and positively with backup behaviors and positivity. Correlations amongst the dimensions of quality of care were higher between patient centeredness and effectiveness (r = .55) than between personal barriers and any of the other two (r = .08 with effectiveness and r = .10 with patient centeredness).
Considering H1 (see Table 3), the existence of job demands (cognitive, emotional, and physical) significantly predicted patient centeredness (p = .0001), effectiveness (p = .000), and personal barriers (p = .000). Therefore, H1 was supported. The value of the betas shows relationships of greater magnitude between job demands and the personal barriers dimension of QoC. Considering effectiveness, physical demands are its weakest predictor and cognitive demands are the ones with lowest impact on patient centeredness.
Table 4 presents the results of testing hypotheses 2 and 3, providing the value for the indirect effect for each model and the confidence intervals (at 95%) for testing the significance of the indirect effect. Indirect effects are considered significant (signaled with **) when 0 falls out of the confidence interval (Preacher & Hayes, 2004, 2008).
The indirect effects of job demands on quality of care through backup behaviors were found to be significant, supporting our second hypothesis for all of the dimensions of quality of care. The hypothesized indirect effect of job demands on quality of care through positivity (hypothesis 3) was also significant, except considering the effect of emotional demands on personal barriers (indirect effect = -.0190; 95% CI: -.0408, .001 with 5,000 resamples).
The indirect effects are mostly higher when quality of care effectiveness dimension is the output, when emotional demands are the independent variable, and considering backup behaviors as the mediator. The greater indirect effect was found in the relationship between emotional demands and quality of care effectiveness, mediated by backup behaviors (indirect effect = -.1964; 95% CI: -.2397, -.1596 with 5,000 resamples).
The test of the final hypothesis (hypothesis 4) was also made using the PROCESS macro, but choosing model 6 (Hayes, 2012), a double mediation model. Results are presented in Table 5.
Only two of the double mediations were not significant, both considering personal barriers as the dependent variable (indirect effect = -.0017, 95% CI: -.0046, -.0000 with 5,000 resamples for cognitive demands as independent variable and indirect effect = -.0019, 95% CI: -.0062, -.0000 with 5,000 resamples for emotional demands as independent variable). Thus, hypothesis 4 was partially supported. The higher indirect effects of the double mediation were found between physical demands and the personal barriers of quality of care (indirect effects = -.0021).
Discussion
The main goal of the present paper was to contribute to our understanding of the relationship between job demands and quality of care in hospital settings, and to specifically highlight the role of backup behaviors and positivity as dampers of that negative relationship. Our results shed some light on this relationship and on hospital dynamics.
Firstly, considering the direct effects, as expected, job demands predicted quality of care: the existence of physical, emotional, and cognitive demands tends to worsen the quality of care provided. Job demands show a greater direct impact on personal barriers to providing good quality of care. Therefore, it seems that demands are central, have a stronger direct impact on health professionals' health and well-being (e.g., tiredness) and, consequently, on their ability to focus on their tasks and patients.
Secondly, the impact of job demands on the personal barriers dimension of QoC is likely to be direct, while backup behaviors and positivity are important mediators between job demands and the patient centeredness and the effective dimensions of QoC, and more so with this last dimension.
The existence of backup behaviors may foster the positivity ratio of HPs. However, the magnitude of the double mediation effect is smaller than the effects obtained through simple mediations. It would not be completely odd to consider a reverse causality relationship: the higher the positivity ratio the higher the well-being and happiness of an individual and his/her willingness to invest in social relationships. In addition, backup behaviors have a more relevant role, indicating that the improvement of QoC is more likely to happen in a cooperative context (backup behaviors). Hence, for the time being and in terms of practical implications, it is central to consider team dynamics when thinking about improving the quality of care in the hospital. We must then go beyond a rather simplistic view of what will facilitate providing adequate quality of care - having the right equipment and facilities, adequate cognitive challenging activities, support from co-workers and supervisors, and an adequate administration of resources do not alone account for all the fluctuations in QoC. In a demanding context, where professionals usually have a high workload and work under time pressure (Carayon & Gurses, 2005; Linzer et al., 2000; Silva et al., 2013), having the ability to detect and act upon situations where co-workers have a workload that goes beyond what they can actually achieve (i.e., backup behaviors) is fundamental for the effectiveness of the professionals. This implies that HPs are not only attentive to detect those situations but also willing to reach out to their peers and team members. However, providing backup behaviors may also have negative effects. According to Barnes et al. (2008), backup behavior providers risk neglecting their own work and backup behaviors receivers may decrease their investment in taskwork in a subsequent task, particularly when they are aware that other team members can recognize their workload. This may lead to situations where workload becomes, again, unevenly distributed, generating the noxious consequences already mentioned. The monitoring of adequate amounts of backup behaviors might be an important function of the team leader (for example, the department leader/coordinator or the chief nurse in a specific service). Indeed, Teng, Lee, Chu, Chang, and Liu (2012) found that employees' intention to help their co-workers is negatively related to their supervisor's negative mood when the employee-supervisor relationship is weak.
Third, the personal barriers dimension of QoC presents a somewhat different pattern of relationships than the other two QoC dimensions. Indeed, one unexpected finding was the non-significance (although closely reaching significance) of the indirect effect of emotional demands on personal barriers in providing good quality of care through positivity. We would have anticipated that positivity could be a powerful mediator specifically between those two variables since all are related to affective experiences and it was not the case. The results of the double mediation are also non-significant, considering the effects of both emotional and cognitive demands on personal barriers. However, positivity as a simple mediator has a greater impact on physical demands' relationship with this dimension of QoC, in comparison with the other two. It seems then that the prevalence of positive experiences and emotions over negative ones is not sufficient to influence the impact of emotional demands, such as the fear of doing something wrong or the spillover of work life into family life, on the tiredness of HPs, or on their personal problems and its influence on the quality of care they deliver. At the same time, an investment in decreasing physical strain may result in a bigger improvement on this particular dimension of QoC, especially when backup behaviors exist. Indeed, considering physical demands, the double mediation has a greater effect precisely with the personal barriers dimension of QoC, and not with effectiveness or patient centeredness, which show similar effect values.
To sum up, the results of this study imply that quality of care in hospital settings is closely related to job demands. Interventions aimed at improving the effectiveness and patient centeredness of QoC will have greater success if they are directed at physical demands. Also, hospital managers should not overlook the importance of cooperation within teams and should find ways to develop teamwork. For example they should foster shared cognitions (e.g., team shared mental models, team situation awareness), provide opportunities for team training (e.g., in explicit communication skills) (Salas, Cooke, & Rosen, 2008), and develop teamwork adjustment behaviors such as intra-team coaching or collaborative problem solving and task related collaborative behaviors (e.g., coordination, information exchange) (Rousseau, Aubé, & Savoie, 2006). This will impact quality of care indirectly in all of its dimensions.
Health care around several European countries is moving towards a patient-centred and consumer-focused system based on a market-oriented approach (Sofaer & Firminger, 2005) that requires a careful consideration and monitoring of its quality of care. Furthermore, some studies (Arocena & García-Prado, 2007) show an improvement in hospital performance mainly driven by an increase of quality of care. In the end, improving QoC in the hospital reflects an improvement of human life, human rights, and human dignity.
Conflict of Interest
The authors of this article declare no conflict of interest.
Acknowledgements
We thank all the partners from ORCAB project in both collecting data and contributing with their input to the final manuscript.
1Both the Hospital Work-Experience Scale and the ORCAB Quality of Care Scale have been developed using focus groups, interviews and survey data. Qualitative and quantitative information on the scales can be provided by the 9th author upon request.
References
1. Aiken, L. H., Sermeus, W., Van den Heede, K., Sloane, D. M., Busse, R., McKee, M., ... Kutney-Lee, A. (2012). Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. British Medical Journal, 344, e1717. doi:10.1136/bmj.e1717. [ Links ]
2. Arocena, P., & Garcia Prado, A. 2007. Accounting for Quality in the Measurement of Hospital Performance: Evidence from Costa Rica. Health Economics 16, 667-685. doi: 10.1002/hec.1204. [ Links ]
3. Ashkanasy, N. M. (2003). Emotions in organizations: A multilevel perspective. In F. Dansereau & F. J. Yammarino (Eds.), Research in multi-level issues, vol. 2: Multi-level issues in organizational behavior and strategy (pp. 9-54). Oxford, UK: Elsevier Science. [ Links ]
4. Bakker, A. B., & Demerouti, E. (2007). The Job Demands-Resources model: State of the art. Journal of Managerial Psychology, 22, 309-328. doi: 10.1108/02683940710733115. [ Links ]
5. Bakker, A. B., Demerouti, E., & Schaufeli, W. B. (2003). Dual processes at work in a call centre: An application of the Job Demands a Resources model. European Journal of Work and Organizational Psychology, 12, 393-417. doi: 10.1080/13594320344000165. [ Links ]
6. Bakker, A. B., Demerouti, E., & Verbeke, W. (2004). Using the Job Demands Resources model to predict burnout and performance. Human Resource Management, 43, 83-104. doi: 10.1002/hrm.20004. [ Links ]
7. Barnes, C. M., Hollenbeck, J. R., Wagner, D. T., DeRue, D. S., Nahrgang, J. D., & Schwing, K. M. (2008). Harmful help: The costs of backing up behavior in teams. Journal of Applied Psychology, 93, 529-539. [ Links ]
8. Bartlett, G., Blais, R., Tamblyn, R.M., Clermont, R., & MacGibbon, B. (2008). The impact of patient communication problems on the risk of suffering preventable adverse events in acute care settings. Canadian Medical Association Journal, 178, 1555-1562. [ Links ]
9. Bolte, A., Goschkey, T., & Kuhl, J. (2003). Emotion and intuition: Effects of positive and negative mood on implicit judgments of semantic coherence. Psychological Science, 14, 416-421. doi: 10.1111/1467-9280.01456. [ Links ]
10. Campbell, S. M., Roland, M. O., & Buetow, S. A. (2000). Defining quality of care. Social Science & Medicine, 51, 1611-1625. [ Links ]
11. Caplan, R. P. (1994). Stress, anxiety, and depression in hospital consultants, general practitioners, and senior health service managers. British Medical Journal, 309, 1261-1263. doi: 10.1136/bmj.309.6964.1261. [ Links ]
12. Carayon, P., & Gurses, A. (2005). Nursing workload and patient safety in intensive care units: A human factors engineering evaluation of the literature. Intensive and Critical Care Nursing, 21, 284-301. doi: 10.1.1.182.7072. [ Links ]
13. Chambers, R., Wall, D., & Campbell, I. (1996). Stresses, coping mechanisms and job satisfaction in general practitioner registrars. British Journal of General Practice, 46, 343-348. [ Links ]
14. Demerouti E., Bakker, A. B., Nachreiner, F., & Schaufeli, W. B. (2001). The Job Demands - Resources model of burnout. Journal of Applied Psychology, 86, 499-512. Doi: 10. i037//002i-9010.86.3.499. [ Links ]
15. Donabedian, A. (1980). The definition of quality: A conceptual exploration. Explorations in Quality Assessment and Monitoring, 1, 3-31. [ Links ]
16. Eckleberry-Hunt, J., Lick, D., Boura, J., Hunt, R., Balasubramaniam, M., Mulhem, E., & Fisher, C. (2009). An exploratory study of resident burnout and wellness. Academy of Medicine, 84, 269-277. doi: 10.1097/ACM.0b013e3181938a45. [ Links ]
17. European Comission (2008). Communication and Recommendation on Patient Safety, including the Prevention and Control of Healthcare-Associated Infections - Summary of the Impact Assessment. European Commission, Brussels. [ Links ]
18. Fahrenkopf, A. M., Sectish, T. C., Barger, L. K., Sharek, P. J., Lewin, D., Chiang, V. W., ... Landrigan, C. P. (2008). Rates of medication errors among depressed and burnt out residents: prospective cohort study. British Medical Journal. 336, 488-491. doi: org/10.1136/bmj.39469.763218. [ Links ]
19. Firth-Cozens, J. (1995). Stress in doctors: a longitudinal study. Leeds: University of Leeds. [ Links ]
20. Fredrickson, B. L. (2001). The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist, 56, 218-226. doi: 10.1037//0003-066X.56.3.218. [ Links ]
21. Fredrickson, B., & Joiner, T. (2002). Positive emotions trigger upward spirals toward emotional well-being. Psychological Science, 13, 172-175. doi: 10.1111/1467-9280.00431. [ Links ]
22. Fredrickson, B. L., & Losada, M. (2005). Positive affect and the complex dynamics of human flourishing. American Psychologist, 60, 678-686. doi: 10.1037/0003-066X.60.7.678. [ Links ]
23. Fredrickson, B. L., Tugade, M. M., Waugh, C. E., & Larkin, G. R. (2003). What good are positive emotions in crisis? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. Journal of Personality & Social Psychology, 84, 365-376. [ Links ]
24. Ghodse, H., & Galea, S. Misuse of drugs and alcohol (2006). In J. Cox, J. King, A. Hutchinson, & P. McAvoy (Eds.), Understanding doctors Performance (pp. 38-48). Oxford: Radcliffe Publishing. [ Links ]
25. Hakannen, J. J., Bakker, A. B., & Schaufeli, W. B. (2006). Burnout and work engagement among teachers. Journal of School Psychology, 43, 495-513. doi:10.1016/j. jsp.2005.11.001. [ Links ]
26. Hayes, A. F. (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling (White paper). Retrieved from http://www.afhayes.com/public/process2012.pdf. [ Links ]
27. Institute of Medicine (1999). To err is human: Building a safe health system. Washington, DC: National Academy Press. [ Links ]
28. Isen, A. M., Daubman, K. A., & Nowicki, G. P. (1987). Positive affect facilitates creative problem solving. Journal of Personality and Social Psychology, 52, 1122-1131. doi: 10.1037/0022-3514.52.6.1122. [ Links ]
29. Isikhan, V., Gomez, T., & Danis, M. Z. (2004). Job stress and coping strategies in health care professionals working with cancer patients. European Journal of Oncology Nursing, 8, 234-244. doi: 10.1016/j.ejon.2003.11.004. [ Links ]
30. Kazmi, R., Amjad, S., & Khan, D. (2008). Occupational stress and its effect on job performance. A case study of medical house officers of district Abbottabad. Journal of Ayuberdic Medicine College Abbottabad, 20, 135-139. [ Links ]
31. Krokos, K. J., Baker, D. P., Alonso, Al., & Day, R. (2009). Assessing team processes in complex environments : challenges in transitioning research to practice. In E. Salas (Ed.), Team effectiveness in complex organizations: cross-disciplinary perspectives and approach (pp. 383-408) Routledge: New York. [ Links ]
32. Linzer, M., Konrad, T. R., Douglas, J., McMurray, J. E., Pathman, D. E., Williams, E. S., ... Rhodes, E. (2000). Managed care, time pressure, and physician job satisfaction: results from the physician work life study. Journal of General Internal Medicine, 15, 441-450. doi: 10.1046/j.1525-1497.2000.05239.x. [ Links ]
33. McGowan, Y., Humphries, N., Morgan, K., Conry, M., Montgomery, A., Panagopoulou, E., & McGee, H (2011). Defining quality of care in hospitals: A ten year systematic review of literature 2000-2010 (Chapter IV). In K. Vedhara, E. Panagopoulou, & A. Montgomery (Coords.). Deliverable D3.1 Systematic review: Improving quality and safety in the hospital: The link between organizational culture, burnout and quality of care - ORCAB. Retrieved from http://orcab.web.auth.gr/orcab/. [ Links ]
34. McIntyre, R. M., & Salas, E. (1995). Measuring and managing for team performance: Emerging principles from complex environments. In R. A. Guzzo & E. Salas (Eds.), Team effectiveness and decision making in organizations (pp. 9-45). San Francisco: Jossey-Bass. [ Links ]
35. Porter, C. O. L. H., Hollenbeck, J. R., Ilgen, D. R., Ellis, A. P. J., West, B. J., & Moon, H. K. (2003). Towards understanding backing up behaviors in work teams: The role of personality and the legitimacy of need for backing up others. Journal of Applied Psychology, 88, 391-403. [ Links ]
36. Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879-891. doi: 10.3758/BRM.40.3.879. [ Links ]
37. Richter, P., & Hacker, W. (1998). Workload and strain: Stress, fatigue, and burnout in working life. Heidelberg, Germany: Asagner. [ Links ]
38. Rousseau, V., Aubé, C., & Savoie, A. (2006). Teamwork behaviors: A review and an integration of frameworks. Small Group Research, 37, 540-570. doi: 10.1177/1046496406293125. [ Links ]
39. Salas, E., Cooke, N. J., & Rosen, M. A. (2008). On teams, teamwork, and team performance: Discoveries and developments. Human Factors, 50, 540-547. doi: 10.1518/001872008X288457. [ Links ]
40. Salas, E., Rosen, M. A., Burke, C. S., & Goodwin, G. F. (2009). The wisdom of collectives in organizations: An update of the teamwork competencies. In E. Salas, G. F. Goodwin, & C. S. Burke (Eds.), Team Effectiveness in Complex Organizations. Cross- Disciplinary Perspectives and Approaches (pp. 39-79). New York: Psychology Press. [ Links ]
41. Salas, E., Sims, D. E., & Burke, C. S. (2005). Is There A Big Five In Teamwork? Small Group Research, 36, 555- 599. doi: 10.1177/1046496405277134. [ Links ]
42. Seligman, M., & Csikszentmihalyi, M. (2000). Positive psychology: An Introduction. American Psychologist, 55, 5-14. doi: 10.1037/0003-066X.55.1.5. [ Links ]
43. Shanafelt, T., Bradley, K., Wipf, J., & Back, A. (2002). Burnout and self-reported patient care in an internal medicine residency program. Annals of Internal Medicine, 136, 358-367. [ Links ]
44. Silva, A. S., Costa, P. L., Costa, R., Tavares, S. M., Leite, E. S., & Passos, A. M. (2013). Meanings of quality of care: Perspectives of Portuguese health professionals and patients. British Journal of Health Psychology, 18, 858-873. doi: 10.1111/bjhp.12031. [ Links ]
45. Sofaer, S., & Firminger, K. (2005). Patient perceptions of the quality of health services. Annual Review of Public Health, 26, 513-559. doi: 10.1146/annurev. publhealth.25.050503.153958. [ Links ]
46. Soler, J. K., Yaman, H., Esteva, M., Dobbs, F., Asenova, R. S., Katiæ, M., ... Ungan, M. (2008). Burnout in European family doctors: the EGPRN study. Family Practice, 25, 245-265. doi:10.1093/fampra/cmn03. [ Links ]
47. Sweetman, D., & Luthans, F. (2010). The power of positive psychology: psychological capital and work engagemen", in A. B. Bakker & M. P. Leiter (Eds.), Work Engagement: A handbook of Essential Theory and Practice (pp. 54-68). Hove, UK: Psychology Press. [ Links ]
48. Teng, C., Li, I.-C., Chu, T.-L., Chang, H.-T., & Liu, T.-W. (2012). How can supervisors improve employees' intention to help colleagues? Perspectives from social exchange and appraisal-coping theories. Journal of Service Research, 15, 332-342. doi: 10.1177/1094670511435538. [ Links ]
49. Thompson, E. R. (2007). Development and Validation of an Internationally Reliable Short-Form of the Positive and Negative Affect Schedule (PANAS). Journal of Cross-Cultural Psychology, 38, 227-242. [ Links ]
50. Toral-Villanueva, R., Aguilar-Madrid, G., & Juárez-Pérez. C. A. (2009). Burnout and patient care in junior doctors in Mexico City. Occupational Medicine, 59, 8-13. doi: 10.1093/occmed/kqn122. [ Links ]
51. Watson, D., Clark, L. A., & Tellegen, A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54, 1063-1070. [ Links ]
52. Weinberg, A., & Creed, F. (2000). Stress and psychiatric disorder in healthcare professionals and hospital staff. Lancet, 355, 533-537. doi: 10.1016/S0140-6736(99)07366-3. [ Links ]
53. West, C. P., Huschka, M. M., Novotny, P. J., Sloan, J. A., Kolars, J. C., Habermann, T. M., & Shanafelt, T. D. (2006). Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. The Journal of the American Medical Association, 296, 1071-1078. doi:10.1001/jama.2011.1274. [ Links ]
54. Winstanley, S., & Whittington, R. (2004). Aggression towards health care staff in a UK general hospital: variation among professions and departments. Journal of Clinical Nursing, 13, 3-10. doi: 10.1111/j.1365-2702.2004.00807.x. [ Links ]
55. Xanthopoulou, D., Bakker, A. B., Demerouti, E., & Schaufeli, W. B. (2007). The role of personal resources in the Job Demands-Resources Model. International Journal of Stress Management, 14, 121-141. doi: 10.1037/1072-5245.14.2.121. [ Links ]
![]() Correspondence:
Correspondence:
Patrícia L. Costa.
Office 2W8 (Building I).
Av.a das Forças Armadas.
1649-026 Lisbon, Portugal.
E-mail: patricia_costa@iscte.pt
Manuscript received: 01/05/2014
Revision received: 20/09/2014
Accepted: 15/10/2014