Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.15 no.43 Murcia jul. 2016
CLÍNICA
Factors determining non-adherence to hypertension treatment
Factores de no adhesión al tratamiento de la hipertensión arterial
Fatores da não adesão ao tratamento da hipertensão arterial
Moura, André Almeida*; Godoy, Simone de**; Cesarino, Cláudia Bernardi*** and Mendes, Isabel Amélia Costa****
*Fundamental Nursing Master by University of Sao Paulo. E-mail: andalmo@usp.br
**Pdh. Professor Nursing School. University of São Paulo.
***Associate Professor Faculty of Medicine of São José do Rio Preto
****Lecturing Professor of Nursing School of Ribeirão Preto University São Paulo, Brazil.
ABSTRACT
This study was developed to identify determinant factors of non-adherence in the treatment of hypertensive individuals in a Brazilian municipality. This cross-sectional and descriptive study with a quantitative approach was conducted from November 2012 to April 2013. A total of 138 hypertensive patients participated, 65.9% were female, aged 60.5 years old (SD=11.32) on average, 71% had incomplete primary/middle school and an individual income of 1 to 2 times the minimum wage. In regard to occupation, 39.9% were retired and 21.7% were homemakers. Among the factors contributing to non-adherence to treatment, 70.3% reported personal reasons. Adherence was at 15.9% for non-pharmacological treatment and 21% for pharmacological treatment. We verified the need for new studies within the primary health care sphere conducted with hypertensive patients and also the need for multidisciplinary actions intended to encourage treatment adherence among hypertensive patients cared for in the municipality under study.
Key words: Hypertension; Primary Health Care; Patient compliance.
RESUMEN
El presente estudio tiene como objetivo identificar factores determinantes de la no adhesión al tratamiento de los hipertensos en municipio brasileño. Estudio de corte transversal, descriptivo y de enfoque cuantitativo, en el periodo de noviembre de 2012 a abril de 2013. Participaron 138 pacientes hipertensos, siendo 65,9% de sexo femenino, con media de edad de 60,5 años (DP=11,32), 71% con la escolaridad primer grado incompleto y renta individual de 1 a 2 salarios mínimos. En relación a la ocupación, 39,9% eran jubilados y 21,7% estaban en casa. Entre los factores que contribuyen a la no adhesión al tratamiento 70,3% dos pacientes refirieron aspectos personales. La adhesión fue de 15,9% para el tratamiento no farmacológico y 21% para tratamiento farmacológico. Percibimos la necesidad de nuevas investigaciones en la atención primaria con pacientes hipertensos y desarrollar acciones multiprofesionales que busquen estimular la adhesión al tratamiento de los hipertensos asistidos en el municipio estudiado.
Palabras clave: Hipertensión; Atención primaria a la salud; Cooperación del paciente.
RESUMO
O presente estudo foi desenvolvido com o objetivo de identificar fatores determinantes da não adesão ao tratamento dos hipertensos em município brasileiro. Estudo de corte transversal, descritivo e de abordagem quantitativa, no período de novembro de 2012 a abril de 2013. Participaram 138 pacientes hipertensos, sendo 65,9% do sexo feminino, com média de idade de 60,5 anos (DP=11,32), 71% com a escolaridade primeiro grau incompleto e renda individual de 1 a 2 salários mínimos. Em relação à ocupação, 39,9% eram aposentados e 21,7% eram do lar. Entre os fatores que contribuem para a não adesão ao tratamento 70,3% dos pacientes referiram aspectos pessoais. A adesão foi de 15,9% para o tratamento não farmacológico e 21% para tratamento farmacológico. Percebemos a necessidade de novas pesquisas na atenção primária com pacientes hipertensos e desenvolver ações multiprofissionais que busquem estimular a adesão ao tratamento dos hipertensos assistidos no município estudado.
Palavras chave: Hipertensão; Atenção Primária à Saúde; Cooperação do paciente.
Introduction
Systemic Arterial Pressure (SAP) is a disease of great magnitude in Brazil. It is estimated that about 30 million individuals are hypertensive, representing 36% of the adult male population and 30% of adult females. In line with this high prevalence are the high costs generated by the hospitalization of patients who experience complications caused by this condition; hypertension is a risk factor for various diseases, such as acute myocardial infarction, stroke and chronic kidney disease(1).
Hypertension is defined as a multifactorial clinical condition characterized by high and sustained levels of blood pressure (BP) with a threshold of Systolic Blood Pressure (SBP) > 140 mmHg and/or Diastolic Blood Pressure (DBP) > 90 mmHg, validated by repeated measures taken under proper conditions on at least three occasions(1).
The medication scheme to treat hypertension is composed of groups of medications with diverse actions, the objective of which is to reduce cardiovascular morbidity and mortality. This benefit is observed regardless of the class of drug used. Note that treatment includes more than just drugs: modifying one's lifestyle is also necessary. Therefore, changing habits and behavior toward food, smoking, alcohol, and exercise is necessary. Changing one's lifestyle involves changing how one lives and the very idea of health that an individual holds(2-3).
Adherence is defined and characterized by the level of agreement between what the physician prescribes and the individual's behavior in terms of medication, nutrition and changes in lifestyle(1).
Treatment adherence is multifactorial and remains a challenge for those involved: patients and healthcare providers, especially in the context of primary health care. Hence, professionals require studies that will help them understand their working contexts and devise successful interventions to be implemented among the largest number of hypertensive patients, since few papers address the adherence of hypertensive patients to treatment in the context of primary health care(4).
Therefore, it is crucial that healthcare professionals identify, in the population under their care, which variables are involved and associated with treatment abandonment or failure to comply with therapeutic instructions, considering the structure available for this population and the need for studies assessing the implementation of strategies aimed to deal with the problem of non-adherence to treatment(5).
This study's objective was to identify factors that determine non-adherence to treatment among hypertensive patients in a Brazilian municipality.
Material and Methods
This cross-sectional and descriptive study was conducted in Santa Helena de Goiás, GO, Brazil. Data collection was divided into two phases implemented from November 2012 to April 2013.
We sought hypertensive patients enrolled in the Management System at the PHC Hypertension and Diabetes Mellitus Clinic (SISHIPERDIA) of each Family Health Unit in the municipality of Santa Helena de Goiás, GO, Brazil from November 2012 to January 2013.
To identify and include patients in the study, their medical records were assessed considering the following criteria: being older than 18 years old, both genders, having a diagnosis of hypertension for at least one year up to the data collection date, being enrolled in SISHIPERDIA, having no other non-transmissible chronic disease; and having in their records some measurement of systolic blood pressure equal to or greater than 140 mmHg and diastolic blood pressure equal to or greater than 90 mmHg, collected during any appointment attended for 2011 or 2012.
Afterwards, data from SISHIPERDIA were compared with data provided on B-HA files from the SIAB (Primary Health Care Information System) used by the community health agents of each unit. This procedure was intended to identify whether the patients were within the area covered by each Family Health Unit.
Among all the patients identified in each FHU, only those enrolled both in SISHIPERDIA and in the SIAB were included in the list.
From February to April 2013, the primary researcher visited the patients listed and invited them to participate in the study. On the same occasion, the study's objectives were clarified for the patients and those who consented to participate signed free and informed consent forms. Whenever possible the interview was held immediately after these preliminaries; otherwise, it was scheduled for a later date or for a patient to visit the most accessible FHU.
A form adapted from the one adopted by Dosse et al (2009) was used. The first part addressed the participants' sociodemographic and socioeconomic information (gender, age, education, occupation, family and individual income, housing, and number of individuals drawing on the family income)(6).
The second portion of the instrument is composed of six closed questions. The first two questions address non-pharmacological treatment and classify participants into five groups: Group 0 - those who maintain a healthy lifestyle; Group 1 - those who have at least, one unhealthy habit; Group 2 - those who have two unhealthy habits; Group 3 - those who have three unhealthy habits; and Group 4 - those who do not have healthy habits. All those who presented at least one unhealthy habit were considered non-adherent to non-pharmacological treatment. The four last questions classify adherence to pharmacological treatment according to Morisky-Green Test (MGT): patients scoring four are considered to be adherent to treatment and those who score three or less are considered to be non-adherent to treatment. The following questions were included: 1) Have you ever forgotten to take your medicine? 2) At times are you not careful about taking your medicine? 3) When you feel better, do you sometimes stop taking your medicine? 4) At times, if you feel worse when you take your medicine, do you stop taking it?.
The interviews were conducted by the researcher, who checked the options the patients indicated. Afterwards, data were double entered in an Excel spreadsheet and descriptive analyses including absolute frequencies and percentages were processed using the Statistical Package for the Social Science (SPSS), version 16.0.
The study was approved by the Institutional Review Board at the University of São Paulo at Ribeirão Preto, College of Nursing (No. 131.710) in accordance with Resolution 196/96 from the National Council of Health. There are no conflicts of interest among those involved with the study.
Results and Discussion
A total of 254 patients were identified, 138 of which were interviewed. Most, or 91 interviewees (65.9%), were women and 47 (34.1%) were men. The average age was 60.5 years old (SD=11.32); the youngest participant was 26 years old and the oldest was 82 years old.
In regard to gender and age, data found in this study coincide with those presented in the literature. Hypertension is the most frequent chronic condition found among the elderly. Studies report a prevalence of greater than 60% in this population, therefore, establishing the correct diagnosis and persistence of patients in maintaining follow-up is necessary to achieve the ideal goals of treatment and reduce cardiovascular morbidity and mortality(7-9).
In regard to gender, studies addressing adherence report that 82% of the hypertensive patients were female(10).One study addressing treatment adherence, however, found that 79.2% of the hypertensive patients hospitalized in a private hospital in the interior of São Paulo were male(11).
We present the socioeconomic characterization of patients in Table 1.
Most patients n=98 (71%) reported "incomplete primary school" and individual income from 1 to 2 times the minimum wage. In regard to occupation, 55 (39.9%) were retired and 30 (21.7%) were homemakers. In regard to family income, 101 (73.2%) hypertensive patients reported from 1 to 2 times the minimum wage; 54 (39.1%) reported two people lived with this income, while 35 (25.4%) reported three people. In regarding to housing, 123 (89.1%) owned their homes outright.
Some of the information is similar to that found in studies addressing adherence to hypertension treatment in Ceará and in the interior of Pernambuco, where 90% of the sample owned their homes and more than 60% had complete or incomplete primary/middle school(10, 12).
Though hypertension affects individuals regardless of their socioeconomic or education statuses, having a low socioeconomic status plays an important role and interferes in other health situations, such as access to healthcare services, level of information, understanding regarding the disease, and treatment adherence(13).In regard to occupation, retirement is the most frequent situation reported by studies addressing adherence to hypertension treatment(4, 8, 11).
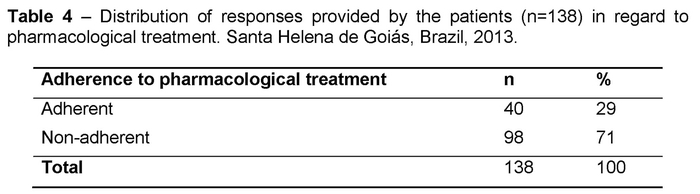
Data concerning adherence to non-pharmacological and pharmacological treatments are presented in Tables 2, 3, and 4.
Low income is an important factor in treatment adherence and was reported by 10 (7.2%) patients. The bibliographic survey revealed that, among the various factors related to the patient, low economic status plays a crucial role in the treatment adherence of hypertensive patients, as well as cultural factors, access to health services, and level of knowledge concerning the disease(14).
Age as a determinant factor was reported by 13 (9.4%) patients. The approach to adherence should be different in each age group, paying attention to the needs and difficulties presented by hypertensive patients. Additionally, hypertensive elderly individuals can help disseminate knowledge concerning this condition to younger generations in their families, providing information to improve self-care, while taking into account structural and familial aspects(15).
Behavioral beliefs, customs regarding health practices, values and perceptions of patients in regard to the disease and treatment differ from those of healthcare providers, considering these individuals belong to groups that differ in sociocultural, linguistic, and psychological terms(14).
The results reported by a study conducted in Teresina, PI, Brazil, show that most interviewees lacked information regarding their condition and treatment and, as a consequence, did not adhere to their treatment(16).
This was also the case of five (3.6%) patients included in this study who reported a lack of knowledge or inadequate knowledge regarding the treatment's benefits.
Poor familial support was reported by 19 (13.8%) of this study's participants. Given this finding, we should note that families should be directly involved in the care provided to hypertensive patients because change in habits requires effective engagement on the part of all those involved(12).
The personal factors interfering in the proper management of blood pressure reported by this study's patients include psychological factors, stress, changes in sleep patterns, and difficulty implementing lifestyle changes, n= 97 (70.3%).
This study's results are similar to those of another two studies reporting that emotional and psychological factors were the most frequently mentioned factors that hinder treatment adherence(6, 17).
The relationship between stress and hypertension has been studied for five decades and is an important risk factor for the development of coronary artery disease. It is currently believed that negative emotions and affections, not only rage and hostility, but also fear, shame and guilt, may trigger stress(18).
Changes in sleep patterns were also reported by this study's participants. Some sleep disorders can hinder proper management of hypertension or even favor its onset(19).
Another factor listed by the participants was genetics. The contribution of genetics to the emergence of hypertension is well-established in the population, though, at present there are no genetic variants used to predict the risk of individuals to develop hypertension(1).
The white coat effect, reported by many of the participants in this study, is a syndrome that has unknown determinants and is defined by the difference between measurements taken in the physician's office and outside of it, as long as this difference is equal to or greater than 20 mmHg in systolic pressure and/or 10 mmHg in regard to the diastolic pressure(1).
Waiting time was reported by one of this study's participants as a factor that interferes in treatment adherence. Note that the time patients spent in consultations, duration of therapy and therapeutic scheme influences patient behavior(20).
The presence of adverse effects was reported by 6 (4.3%) of the patients in this study. One study conducted in the interior of the state of São Paulo addressing adverse effects and treatment adherence reports that none of the patients experiencing adverse effects adhered to the hypertension treatment(21).
Still in regard to the therapy, three patients (2.2%) reported that the schedule on which they are supposed to take the medicine was a factor that hindered treatment adherence. Another three hypertensive patients reported that the frequency and number of drugs was a factor that interfere in adherence. In regard to these aspects, a bibliographic study suggests that the simplification of doses for the convenience of patients is a tool that favors treatment adherence(14).
Another element reported by those interviewed in this study was difficulty accepting and adapting to a different lifestyle, n=58 (42%). A study addressing the reasons that patients abandoned follow-up reports that only one third of the patients reported having implemented changes in lifestyle to control hypertension. Modification of lifestyle involves behavioral changes that should not be considered free choices out of context(22).
Lack of symptoms and the chronic nature of the disease were the reasons reported by the patients for therapeutic failure and abandonment of medications, according to a study conducted in Teresina(16). These reasons were also reported by 14 (10.2%) participants in this study.
In regard to adherence of hypertensive patients to lifestyle changes, that is, changes not concerned with medication, 22 (15.9%) patients reported having healthy habits while 116 (84.1%) reported not following healthy habits (Table 3).
The percentage of participants who did not adhere to non-pharmacological treatment was 84.1%. This finding, together with factors affecting BP such as difficulty accepting and adapting to lifestyle changes, n=58 (42%), shown in Table 2, reveals that patients face difficulties modifying their behaviors.
Providing guidance in regard to a healthy lifestyle, such as not consuming alcohol, not smoking, planning a diet low in sodium and calories, managing stress and exercising regularly, should be part of the care provided to hypertensive patients. Patients experience improved quality of life when they adopt a healthier lifestyle, which positively influences the management of blood pressure(4).
The VI Brazilian Guidelines of Hypertension lists the benefits for decreased BP in the face of changes in lifestyle, such as: adopting the Dietary Approach to Stop Hypertension (DASH) can reduce SBP from 8 to 14 mmHg; decreasing salt consumption by 2 grams a day, at most, reduces SBP from 2 to 8 mmHg; moderate consumption of alcohol decreases it from 2 to 4 mmHg; and at least 30 minutes of exercises a day three times a week reduces BP from 4 to 9 mmHg(1).
Following a low-sodium diet was reported by approximately 64% of the participants, a finding very similar to that reported in a study conducted in the interior of São Paulo in which 60% of the participants reported restricted salt consumption(22).
Twenty-one individuals (15.2%) in this study were smokers. This finding differs from a study conducted in Januária, MG, Brazil in which a smaller percentage was found; 7.4% of the patients reported smoking in that study(3).
A total of 63.8% of the individuals did not exercise regularly, which is in agreement with a study conducted in the city of Ribeirão Preto and which also reported that fewer than half of the individuals adhered to the regular practice of exercise, despite recommendations(7).
According to the MGT, 40 (29%) patients adhered to pharmacological treatment, while 98 (71%) scored below or equal to 3; that is, the latter were classified as non-adherent (Table 4).
Due to low treatment adherence, the percentage of individuals with blood pressure measurements within normal parameters is low, despite evidence showing that anti-hypertensive treatment is efficient in reducing cardiovascular morbidity and mortality(1). Studies using MGT report that from 72% to 86% of the patients does not adhere to pharmacological treatment proposed(6, 8 23).
In regard to adherence to pharmacological therapy to treat hypertension, studies addressing patients who regularly take medication show that they may occasionally miss some doses, which has an impact on the anti-hypertensive effect and imposes a risk of cardiovascular disease. Therefore, anti-hypertensive drugs with sustained efficacy beyond a 24-hour period may minimize doses that may be missed during the treatment(2).
The results presented show that lack of adherence is multifactorial, such that diverse measures should be adopted to maintain treatment adherence. These measures should be based on clinical evidence and associated with multidisciplinary mobilization in order to promote greater engagement of patients during their treatment(20).
A practice widely used is health education focused on self-care, encouraging self-perception regarding the disease and sharing responsibility with the patient so that these individuals can achieve the highest level of health and quality of life possible. A review of the Brazilian literature addressing educational actions promoted by nurses between 1990 and 2010 directed to hypertensive patients shows that about 50% of the papers address education in health as a tool to encourage treatment adherence. Coupled with that, the papers also always indicate the need for a multidisciplinary practice of health education; that is, this should not be an integrated part only of nursing professionals but for all those providing care to hypertensive patients(12, 24).
Additionally, public and institutional policies involving healthcare providers should be implemented to improve adherence and, consequently, lead to a better prognosis among patients(25).
Final Considerations
Hypertension is a cardiovascular disease with important repercussions for primary health care and has multifactorial causes. It is the primary risk factor for heart attack, stroke, and chronic kidney disease.
The results also show that further research is needed to identify the factors that lead to treatment non-adherence on the part of hypertensive patients.
The population under study presented the following characteristics: most were female aged 60.5 years old on average, had low educational level, presented low rates of treatment adherence, and reported that psychosocial factors or stress along with difficulty to implement changes in lifestyle hindered treatment adherence.
We suggest the design and implementation of projects with multidisciplinary actions directed to this population to encourage treatment adherence, improving existing technologies and/or devising new technologies to strengthen the adherence of patients to treatment and to qualify healthcare providers, especially those from the Centers that Support the Family Health Strategy, in order to improve care delivered to this specific group.
Therefore, actions in primary health care to promote health and prevent complications arising from hypertension are very relevant and contribute to reducing public expenditure, hospitalizations due to clinical complications, and to improving the quality of life of this population.
Received: February 4, 2015
Aceppted: April 18, 2015
References
1. Sociedade Brasileira de Cardiologia, Sociedade Brasileira de Hipertensão, Sociedade Brasileira de Nefrologia. VI Diretrizes Brasileiras de Hipertensão Arterial. Revista Brasileira de Hipertensão. 2010; 17 (1): 1-65. [ Links ]
2. Mion Jr. D, Ortega KC. Adesão ao tratamento de acordo com os medicamentos utilizados. In: Nobre F, Mion Jr., D (Org.). Adesão ao tratamento - o grande desafio das doenças crônicas e da hipertensão arterial. São Paulo: Leitura Médica, 2013. [ Links ]
3. Oliveira TL, Miranda LP, Fernandes OS, Caldeira AP. Eficácia da educação em saúde no tratamento da hipertensão arterial. Acta Paulista de Enfermagem.2013; 26(2): 179-84. [ Links ]
4. Pierin AMG, Marroni SN, Taveira LAF, Benseñor IJM. Controle da hipertensão arterial e fatores associados na atenção primária em unidades básicas de saúde localizadas na região oeste da cidade de São Paulo. Ciência & Saúde Coletiva. 2011; 16 Suppl 1: S1389-400. [ Links ]
5. Reineirs AAO, Azevedo RCS, Vieira MA, Arruda ALG. Produção bibliográfica sobre adesão/não-adesão de pessoas ao tratamento de saúde. Ciência & Saúde Coletiva. 2008; 13 Suppl 2: S2299-306. [ Links ]
6. Dosse C, Cesarino CB, Martin JFV, Castedo MCA. Fatores associados à não adesão dos pacientes ao tratamento da hipertensão arterial. Revista Latino-Americana de Enfermagem. 2009; 17 (2): 201-6. [ Links ]
7. Bastos-Barbosa RG, Ferriolli E, Moriguti JC, Nogueira CB; Nobre F; Ueta J; Lima NKC. Adesão ao tratamento e controle da pressão arterial em idosos com hipertensão. Arquivos Brasileiros de Cardiologia. 99 (1): 636-41. [ Links ]
8. Cavalari E, Nogueira MS, Fava SMCL, Cesarino CB, Martin JFV. Adesão ao tratamento: estudo entre portadores de hipertensão arterial em seguimento ambulatorial. Revista de Enfermagem da UERJ. 2012; 20(1): 67-72. [ Links ]
9. Girotto E, Andrade SM, Cabrera MAS, Matsuo T. Adesão ao tratamento farmacológico e não farmacológico e fatores associados na atenção primária da hipertensão arterial. Ciência & Saúde Coletiva.2013; 18 (6): 1763-72. [ Links ]
10. Bezerra DS, Silva AS, Carvalho ALM. Avaliação das características dos usuários com hipertensão arterial e/ou diabetes mellitus em uma Unidade de Saúde Pública, no município de Jaboatão dos Guararapes-PE, BRASIL. Revista de Ciências Farmacêuticas Básica e Aplicada.2009; 30 (1): 69-73. [ Links ]
11. Calixto AATF. Adesão ao tratamento: estudo entre portadores de hipertensão arterial internados em um hospital privado no interior paulista (dissertação). Ribeirão Preto: Escola de Enfermagem de Ribeirão Preto/USP; 2010.109 p. [ Links ]
12. Santos ZMSA, Frota MA, Cruz DM, Holanda SDO. Adesão do cliente hipertenso ao tratamento: análise com abordagem multidisciplinar. Texto & Contexto Enfermagem. 2005; 14 (3): 332-40. [ Links ]
13. Faria HTG. Fatores relacionados à adesão do paciente diabético à terapêutica medicamentosa (dissertação). Ribeirão Preto: Escola de Enfermagem de Ribeirão Preto/USP; 2008. 127 p. [ Links ]
14. Santos MVR, Oliveira DC, Arraes LB, Oliveira DAGC, Medeiros L, Novaes MA. Adesão ao tratamento anti-hipertensivo: conceitos, aferição e estratégias inovadoras de abordagens. Revista da Sociedade Brasileira de Clínica Medica. 2013; 11 (1):55-61. [ Links ]
15. Lima NKCL. Adesão ao tratamento nas diversas faixas etárias. In: Nobre F, Mion Jr D (Org.). Adesão ao tratamento - o grande desafio das doenças crônicas e da hipertensão arterial. São Paulo: Leitura Médica, 2013. [ Links ]
16. Carvalho ALM, Leopoldino RWD, Silva JEG, Cunha CP. Adesão ao tratamento medicamentoso em usuários cadastrados no Programa Hiperdia no município de Teresina (PI). Ciência & Saúde Coletiva. 2012; 17 (7): 1885-92. [ Links ]
17. Fonseca FCA, Coelho RZ, Nicolato R, Malloy-Diniz LF, Silva Filho HC. A influência de fatores emocionais sobre a hipertensão arterial. Jornal Brasileiro de Psiquiatria. 2009; 58 (2): 128-34. [ Links ]
18. Pereira AAM. Aspectos psicológicos envolvidos na não adesão. In: Nobre F, Mion Jr D (Org.). Adesão ao tratamento - o grande desafio das doenças crônicas e da hipertensão arterial. São Paulo: Leitura Médica, 2013. [ Links ]
19. Duarte RLM, Silva RZM, Silveira FJM. Ronco: diagnóstico, consequências e tratamento. Pulmão RJ. 2010; 19 (3-4): 63-67. [ Links ]
20. Giorgi DMA. Estratégias para melhorar a adesão ao tratamento anti-hipertensivo. Revista Brasileira de Hipertensão. 2006; 13 (1): 47-50. [ Links ]
21. Palota L. Adesão ao tratamento da hipertensão arterial: estudo entre usuários cadastrados no Centro de Saúde de um município do interior paulista (dissertação). Ribeirão Preto: Escola de Enfermagem de Ribeirão Preto/USP; 2010. 96 p. [ Links ]
22. Duarte MTC, Cyrino AP, Cerqueira ATAR, Nemes MIB, Iyda M. Motivos do abandono do seguimento médico no cuidado a portadores de hipertensão arterial: a perspectiva do sujeito. Ciência & Saúde Coletiva. 2010; 15(5): 2603-10. [ Links ]
23. Eid LP, Nogueira MS, Veiga EV, Cesarino EJ, Marchi Alves LM. Adesão ao tratamento anti-hipertensivo: análise pelo Teste de Morisky-Green. Revista Eletrônica de Enfermagem. (Internet). 2013 (acesso em: 29 abril 2014); 15(2): 362-7. Disponível em: http://www.revistas.ufg.br/index.php/fen/article/view/15599/14787. [ Links ]
24. Moura AA, Nogueira MS. Enfermagem e educação em saúde de hipertensos: revisão da literatura. Journal of Management and Primary Health Care. 2013; 4 (1): 36-41. [ Links ]
25. NOBRE F. Fatores envolvidos e consequências da não adesão ao tratamento. In: NOBRE, F.; MION Jr., D (Org.). Adesão ao tratamento - o grande desafio das doenças crônicas e da hipertensão arterial. São Paulo: Leitura Médica, 2013. [ Links ]











 texto en
texto en